In a Danish Hospital, 70% of all activations of the rapid response team (RRT) in 2016 were related to adult patients with respiratory insufficiency. The most frequent RRT intervention was continuous positive airway pressure (CPAP). However, there was no systematic follow-up and patients could not receive CPAP outside of daytime hours. The aim of the study was to implement and evaluate a CPAP intervention to improve healthcare.
Patients and methodsA quality inter-professional intervention project was conducted. The interventions consisted of: theoretical and practical education in respiratory insufficiency (including use of CPAP) of nurses and physicians from the general wards, physiotherapists and staff from the RRT; development of an instruction leaflet and video; an update of the existing guidelines. The interventions entailed patients being able to receive CPAP a minimum of 3 times for 5–10min within a 24-h period. All RRT activations were registered and compared in a before–after evaluation of the intervention. Additionally, all staff groups received an electronic questionnaire after implementation.
ResultsAfter implementation, respiratory insufficiency was still the highest primary course for RRT activation. The use of CPAP increased, and the number of patients needing a transfer to the intensive care unit decreased. The response rate for the questionnaire was 44% (203 out of 465), and staff experienced new competences, improved inter-professional cooperation and improved healthcare. However, a substantial number of staff did not feel sufficiently trained or that the intervention was well-implemented.
ConclusionThe intervention entailed new competences for the staff, as well as improved system performance, inter-professional cooperation and healthcare. However, there is a need for continuous focus on the intervention.
En un hospital danés, el 70% de todas las activaciones del equipo de respuesta rápida (RRT) en 2016 estuvieron relacionadas con pacientes adultos con insuficiencia respiratoria. La intervención de RRT más frecuente fue la presión positiva continua en las vías respiratorias (CPAP). Sin embargo, no había un seguimiento sistemático y los pacientes no podían recibir CPAP fuera del horario diurno. El objetivo del estudio era implementar y evaluar una intervención CPAP para mejorar la atención médica.
Pacientes y métodosSe llevó a cabo un proyecto de intervención de calidad interprofesional. Las intervenciones consistieron en: educación teórica y práctica en insuficiencia respiratoria (incluido el uso de CPAP) de enfermeras y médicos de las unidades generales, fisioterapeutas y personal de la RRT; desarrollo de un folleto de instrucciones y un video; una actualización de las directrices existentes. Las intervenciones causaron que los pacientes pudieran recibir CPAP un mínimo de 3 veces durante 5-10min en un período de 24h. Todas las activaciones de RRT se registraron y compararon en una evaluación antes y después de la intervención. Además, todos los grupos de personal recibieron un cuestionario electrónico después de su implementación.
ResultadosDespués de la implementación, la insuficiencia respiratoria seguía siendo la causa primaria más alta para la activación de RRT. El uso de CPAP aumentó, y el número de pacientes que necesitaba una transferencia a la unidad de cuidados intensivos disminuyó. La tasa de respuesta al cuestionario era del 44% (203 de 465), y el personal experimentó nuevas competencias, mejoró la cooperación interprofesional y la atención sanitaria. Sin embargo, un número cuantioso de empleados no se sintió suficientemente capacitado o pensó que la intervención no estaba bien efectuada.
ConclusiónLa intervención implicó nuevas competencias para el personal, así como un mejor rendimiento del sistema, la cooperación interprofesional y la atención sanitaria. Sin embargo, es necesario un enfoque continuo en la intervención.
Acute respiratory failure is one of the most common acute organ failures experienced by hospitalised patients. Patients with acute respiratory failure have a 6-month mortality rate of 30%, increased hospital admissions and impaired function.1,2 Clinical respiratory deterioration can be seen 8–48h prior to a critical care intervention and recognition is frequently delayed, which is associated to more severe outcomes.3,4
Continuous positive airway pressure (CPAP) is a respiratory supportive treatment for patients with spontaneous breathing. It prevents and treats respiratory deterioration. The application of the CPAP face mask maintains the patient's positive end expiratory pressure, which keeps the airways open.5,6 CPAP improves lung mechanics, reduces the work of breathing, and improves oxygenation by recruiting atelectasis alveoli and decreasing intrapulmonary shunt.7,8
A prospective study from 2009 found that 39% of patients reported immediately reduced dyspnoea with CPAP.9 CPAP is a cost-effective technique, which does not require sophisticated equipment, and the CPAP face mask is easy to apply.10
In 2004, the Institute for Healthcare Improvement aimed to reduce hospital mortality.11 One of the strategies was implementation of rapid response teams (RRT), also known as medical emergency teams.11–13 RRT consists of different healthcare professionals and provide care to patients admitted to hospital wards by identifying, screening and treating patients with signs of clinical deterioration.12,14–16
Failure to recognise the development of respiratory failure is the most common reason for delayed RRT activation which has been associated with increased in-hospital mortality.17,18
In 2016, a retrospective review from our hospital showed that 70% of RRT activations were related to adult patients with respiratory insufficiency as the primary problem. The RRT consists of intensive care nurses, who can call the intensivist if needed. At the hospital, CPAP was a physician-prescribed specialist treatment and was initially provided by physiotherapists during daytime hours or by the RRT during the remaining hours. There was no systematic follow-up by nurses from the general ward or physiotherapist after the CPAP was initiated by the RRT. Nurses in the general wards were not accustomed to using CPAP, nor did they have the skills to administer it. Furthermore, because there was no physiotherapist at work outside of daytime hours, patients did not receive CPAP in the evening or during the night. The managements of the RRT, physiotherapists and general wards agreed that it was a problem that a patient could not receive CPAP outside daytime. An extended possibility to receive CPAP in an early and more responsive phase might lead to patients being able to remain on the general wards.10
The aim of the study was to implement and evaluate an intervention to all hospitalised patients with respiratory insufficiency by providing CPAP for all patients 24/7.
Material and methodsInterventionThe intervention had a Plan-Do-Study-Act (PDSA) based approach and consisted of a change in CPAP practice in the hospital organisation so that all patients could receive CPAP 24/7.19 The intervention included an increased focus on respiratory insufficiency, inter-professional collaboration among nurses, physicians and physiotherapists, and education in the use and administration of a CPAP system without connection with mechanical ventilation.
Education sessions were conducted in small groups and were based on theoretical and physiology reviews including symptoms of respiratory insufficiency and indications, practical instruction and dialogue.
The education material had been standardised before the education sessions and was afterwards available on the hospital intranet. The education sessions were one hour in duration. The teaching period lasted for approximately two months from December 2016 to February 2017, with an offer of additional sessions if needed. Furthermore, a staff information leaflet with theory and instructions for the use, adjustment and administration of CPAP was developed, and the guidelines for CPAP were updated. Additionally, an instructional video with physiological theory was produced. It contained demonstration on how to apply the CPAP face mask, perspectives and arguments from the management of each of the three professions. A pulmonologist presented physiology of the lungs and indications for CPAP. The head nurse from the medical ward talked about the ward nurses’ role in recognising, assessing and responding to clinical signs of respiratory deteriorations of the patients. The adjustment and administration of CPAP was presented by the chief physiotherapist. The instructional video was available for all staff on the hospital intranet.
When CPAP was initiated by the RRT, the RRT nurse made sure that the ward nurse was conversant with use of the system and if not, instructed in use. The RRT could assist 24/7 if the ward nurses needed help in relation to CPAP.
The intervention entailed patients being able to receive CPAP a minimum of three times for 5–10min over a 24-h period, morning and afternoon by the physiotherapist, and in the evening, where necessary, by the ward nurses. If patients needed frequent CPAP, they had to be transferred to the intensive care unit.
DesignA quality inter-professional intervention project with before–after evaluation of effects was conducted. Participants were physiotherapists, nurses and physicians from the general wards and staff from the RRT (which consisted of intensive care nurses and intensivists).
BaselineAll RRT activations had been electronically registered since 2015. Baseline data consisted of numbers of RRT activations (including numbers and categories of RRT interventions) with respiratory insufficiency as the primary problem from November 2015 to October 2016.
Effect assessmentThe effect assessments consisted of two elements.
The first element was the electronically registered data, which included a review of numbers of RRT activations with respiratory insufficiency as the primary problem from November 2017 to October 2018. The data included categories (ex. oxygen supply and transfers to the intensive care unit) of interventions made by the RRT.
The second element was an electronic questionnaire survey. It was sent to all physiotherapists, nurses and physicians from the general wards, and RRT staff regardless of whether they had participated in the education sessions or not. The electronic questionnaire was developed based on interviews with nine nurses from three different general wards. They were asked about their experiences and the pros and cons of the use of CPAP.
The questionnaire was pilot-tested in December 2018 by six staff members with all staff groups represented. The questionnaire consisted of 29 questions with options for free-text comments. In January 2019, all staff received information and the questionnaire via e-mail and, if no response, a reminder e-mail.
Data analysisQuantitative data were analysed with descriptive statistics. Qualitative data (free-text comments from the questionnaire) were analysed using content analysis, where data were categorised and condensed into main themes.20
EthicsAccording to Danish law, the study did not need approval from the Regional Committee on Health Research Ethics for Southern Denmark. Participants in the questionnaire survey were informed that participation was voluntary and responses would be confidential. Completion of the questionnaire was considered as consent for use of the data.
ResultsInterventionThe CPAP education was conducted in all the general wards with two-three formal education sessions conducted in each ward for nurses, RRT staff and physiotherapist, and one-two sessions for physicians. Approximately 150 staff members of a total of 450–490 (31–33%) participated. Additionally, all quality improvement staff were introduced to and educated in CPAP treatment.
Registered dataBefore the intervention, the baseline showed that 67% (121 out of 181) of all RRT activations had respiratory insufficiency as the primary problem with an average of 2.4 interventions. The effect assessment showed that 73% (153 out of 210) of all RRT activations had respiratory insufficiency as the primary problem with an average of 2.5 interventions.
In all RRT activations with patients with respiratory insufficiency as the primary problem, the most frequent intervention in both periods was the initiation of CPAP, which increased from 73% (88 out of 121) at baseline to 83% (127 out of 153) in the effect assessment. The second most frequent intervention was arterial blood gases, which had a frequency of 29% at baseline (35 out of 121) and 30% (46 out of 153) in the effect assessment. Oxygen supplementation as an intervention decreased from 26% (32 out of 121) to 16% (24 out of 153) and the initiation of elevated headboards was 17% (20 out of 121) and 21% (32 out of 153), respectively.
At baseline, for 26% (31 out of 121) of all RRT activations on patients with respiratory insufficiency as the primary problem, the patient was transferred to the intensive care unit in relation to the activation. In the effect assessment, 17% (26 out of 153) of patients were transferred.
After the implementation of the extended possibility of CPAP, some of the RRT activations were specific to the initiation of CPAP. In March 2018, the registration of RRT activations added “Initial start of CPAP” as a new option for the primary course for the activation of the RRT. An additional review of the data from March 2018 to October 2018 showed that for 24% (27 out of 112) of all RRT activations with respiratory insufficiency as the primary problem, the primary course for the activation was to initially start CPAP. In the same period, 77% (112 out of 146) of all activations of the RRT had respiratory insufficiency as the primary problem.
Questionnaire surveyA total of 203 out of 465 staff members completed the questionnaire (91 nurses from general wards, 60 physicians from general wards, 12 physiotherapists and 40 RRT staff). The overall response rate was 44% (45% for nurses from general wards, 30% for physicians, 80% for physiotherapists and 80% for RRT staff).
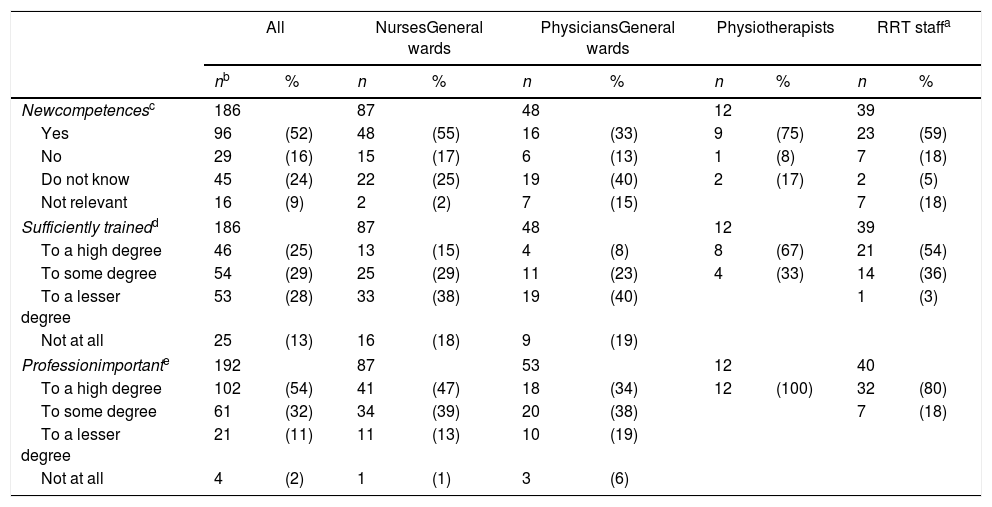
A total of 58% had received CPAP education. Almost half of all the participants (49%) had knowledge of the CPAP guidelines, but these were mostly physiotherapists (83%) and RRT staff (64%). A total of 73%, mostly physicians (87%) and nurses (87%) from the general wards, had no knowledge of the CPAP instructional video. About half of the participants found that the intervention had provided them with new competences, but few nurses and physicians from the general wards found that they had been sufficiently trained in the use and administration of CPAP (Table 1).
Staff education.
| All | NursesGeneral wards | PhysiciansGeneral wards | Physiotherapists | RRT staffa | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| nb | % | n | % | n | % | n | % | n | % | |
| Newcompetencesc | 186 | 87 | 48 | 12 | 39 | |||||
| Yes | 96 | (52) | 48 | (55) | 16 | (33) | 9 | (75) | 23 | (59) |
| No | 29 | (16) | 15 | (17) | 6 | (13) | 1 | (8) | 7 | (18) |
| Do not know | 45 | (24) | 22 | (25) | 19 | (40) | 2 | (17) | 2 | (5) |
| Not relevant | 16 | (9) | 2 | (2) | 7 | (15) | 7 | (18) | ||
| Sufficiently trainedd | 186 | 87 | 48 | 12 | 39 | |||||
| To a high degree | 46 | (25) | 13 | (15) | 4 | (8) | 8 | (67) | 21 | (54) |
| To some degree | 54 | (29) | 25 | (29) | 11 | (23) | 4 | (33) | 14 | (36) |
| To a lesser degree | 53 | (28) | 33 | (38) | 19 | (40) | 1 | (3) | ||
| Not at all | 25 | (13) | 16 | (18) | 9 | (19) | ||||
| Professionimportante | 192 | 87 | 53 | 12 | 40 | |||||
| To a high degree | 102 | (54) | 41 | (47) | 18 | (34) | 12 | (100) | 32 | (80) |
| To some degree | 61 | (32) | 34 | (39) | 20 | (38) | 7 | (18) | ||
| To a lesser degree | 21 | (11) | 11 | (13) | 10 | (19) | ||||
| Not at all | 4 | (2) | 1 | (1) | 3 | (6) | ||||
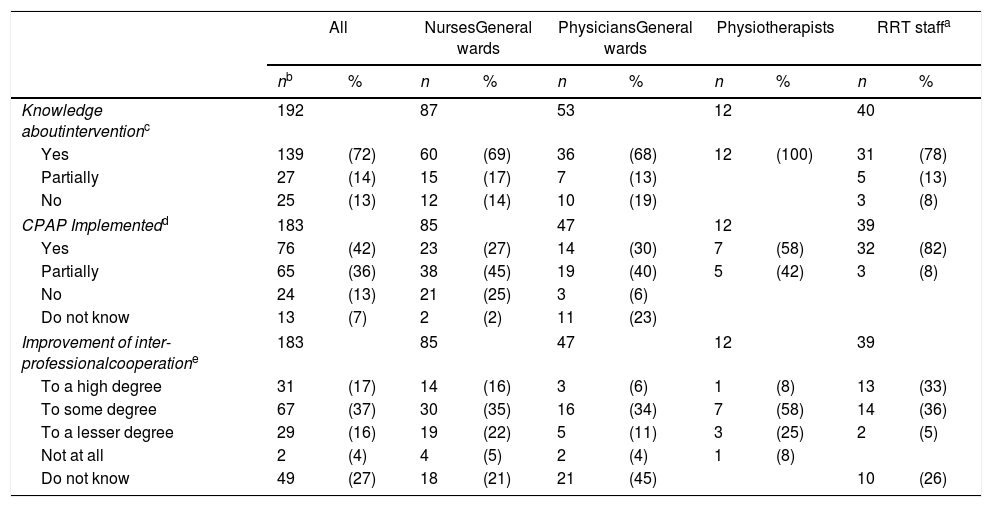
A majority of the participants had knowledge of the intervention. Most participants experienced that the intervention was well-implemented or partially well-implemented, but some of the nurses from the general wards found that the intervention was not well-implemented in their particular ward. Half of the participants experienced improved inter-professional cooperation, either to some extent or to a high degree (Table 2).
Implementation of the intervention.
| All | NursesGeneral wards | PhysiciansGeneral wards | Physiotherapists | RRT staffa | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| nb | % | n | % | n | % | n | % | n | % | |
| Knowledge aboutinterventionc | 192 | 87 | 53 | 12 | 40 | |||||
| Yes | 139 | (72) | 60 | (69) | 36 | (68) | 12 | (100) | 31 | (78) |
| Partially | 27 | (14) | 15 | (17) | 7 | (13) | 5 | (13) | ||
| No | 25 | (13) | 12 | (14) | 10 | (19) | 3 | (8) | ||
| CPAP Implementedd | 183 | 85 | 47 | 12 | 39 | |||||
| Yes | 76 | (42) | 23 | (27) | 14 | (30) | 7 | (58) | 32 | (82) |
| Partially | 65 | (36) | 38 | (45) | 19 | (40) | 5 | (42) | 3 | (8) |
| No | 24 | (13) | 21 | (25) | 3 | (6) | ||||
| Do not know | 13 | (7) | 2 | (2) | 11 | (23) | ||||
| Improvement of inter-professionalcooperatione | 183 | 85 | 47 | 12 | 39 | |||||
| To a high degree | 31 | (17) | 14 | (16) | 3 | (6) | 1 | (8) | 13 | (33) |
| To some degree | 67 | (37) | 30 | (35) | 16 | (34) | 7 | (58) | 14 | (36) |
| To a lesser degree | 29 | (16) | 19 | (22) | 5 | (11) | 3 | (25) | 2 | (5) |
| Not at all | 2 | (4) | 4 | (5) | 2 | (4) | 1 | (8) | ||
| Do not know | 49 | (27) | 18 | (21) | 21 | (45) | 10 | (26) | ||
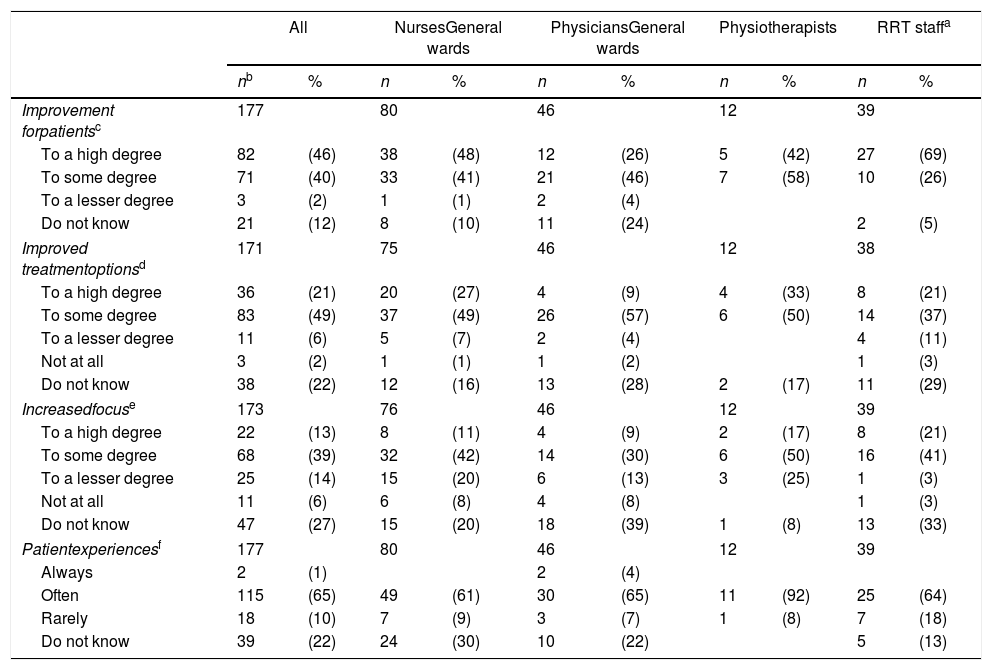
Most participants found that the intervention provided improved treatment options and improved healthcare for the patients. Half of the participants experienced increased focus on patients with respiratory problems. Over 60% from all staff groups experienced that patients often indicated that CPAP relieved their respiratory problems (Table 3).
Effect for patients.
| All | NursesGeneral wards | PhysiciansGeneral wards | Physiotherapists | RRT staffa | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| nb | % | n | % | n | % | n | % | n | % | |
| Improvement forpatientsc | 177 | 80 | 46 | 12 | 39 | |||||
| To a high degree | 82 | (46) | 38 | (48) | 12 | (26) | 5 | (42) | 27 | (69) |
| To some degree | 71 | (40) | 33 | (41) | 21 | (46) | 7 | (58) | 10 | (26) |
| To a lesser degree | 3 | (2) | 1 | (1) | 2 | (4) | ||||
| Do not know | 21 | (12) | 8 | (10) | 11 | (24) | 2 | (5) | ||
| Improved treatmentoptionsd | 171 | 75 | 46 | 12 | 38 | |||||
| To a high degree | 36 | (21) | 20 | (27) | 4 | (9) | 4 | (33) | 8 | (21) |
| To some degree | 83 | (49) | 37 | (49) | 26 | (57) | 6 | (50) | 14 | (37) |
| To a lesser degree | 11 | (6) | 5 | (7) | 2 | (4) | 4 | (11) | ||
| Not at all | 3 | (2) | 1 | (1) | 1 | (2) | 1 | (3) | ||
| Do not know | 38 | (22) | 12 | (16) | 13 | (28) | 2 | (17) | 11 | (29) |
| Increasedfocuse | 173 | 76 | 46 | 12 | 39 | |||||
| To a high degree | 22 | (13) | 8 | (11) | 4 | (9) | 2 | (17) | 8 | (21) |
| To some degree | 68 | (39) | 32 | (42) | 14 | (30) | 6 | (50) | 16 | (41) |
| To a lesser degree | 25 | (14) | 15 | (20) | 6 | (13) | 3 | (25) | 1 | (3) |
| Not at all | 11 | (6) | 6 | (8) | 4 | (8) | 1 | (3) | ||
| Do not know | 47 | (27) | 15 | (20) | 18 | (39) | 1 | (8) | 13 | (33) |
| Patientexperiencesf | 177 | 80 | 46 | 12 | 39 | |||||
| Always | 2 | (1) | 2 | (4) | ||||||
| Often | 115 | (65) | 49 | (61) | 30 | (65) | 11 | (92) | 25 | (64) |
| Rarely | 18 | (10) | 7 | (9) | 3 | (7) | 1 | (8) | 7 | (18) |
| Do not know | 39 | (22) | 24 | (30) | 10 | (22) | 5 | (13) | ||
“To which degree have you experienced improved treatment options for patients with respiratory problems in your ward since the implementation of the intervention?”
Participants who had taken part in a CPAP education session were more likely to assess that CPAP was well implemented and that the inter-professional collaboration had improved compared with participants who had not taken part (supplementary material, Tables S1–S3).
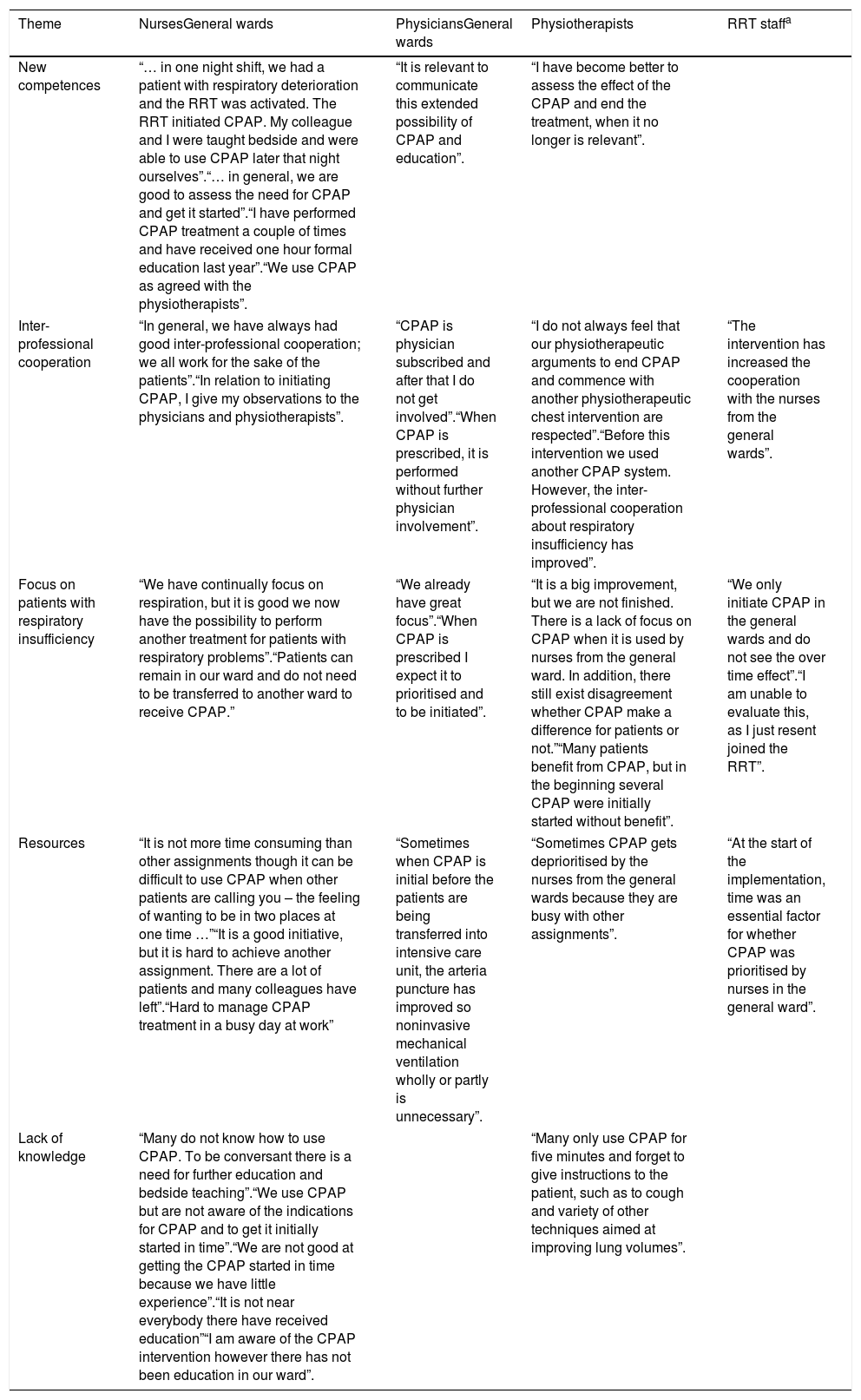
Free-text comments from the questionnaire surveyFive main themes emerged from the content analysis: new competences, inter-professional cooperation, focus on patients with respiratory insufficiency, resources and lack of knowledge. Most comments described lack of knowledge whereas comments that described inter-professional cooperation were fewest. Most comments were from nurses and physicians from the general wards (Table 4).
Free-text comments.
| Theme | NursesGeneral wards | PhysiciansGeneral wards | Physiotherapists | RRT staffa |
|---|---|---|---|---|
| New competences | “… in one night shift, we had a patient with respiratory deterioration and the RRT was activated. The RRT initiated CPAP. My colleague and I were taught bedside and were able to use CPAP later that night ourselves”.“… in general, we are good to assess the need for CPAP and get it started”.“I have performed CPAP treatment a couple of times and have received one hour formal education last year”.“We use CPAP as agreed with the physiotherapists”. | “It is relevant to communicate this extended possibility of CPAP and education”. | “I have become better to assess the effect of the CPAP and end the treatment, when it no longer is relevant”. | |
| Inter-professional cooperation | “In general, we have always had good inter-professional cooperation; we all work for the sake of the patients”.“In relation to initiating CPAP, I give my observations to the physicians and physiotherapists”. | “CPAP is physician subscribed and after that I do not get involved”.“When CPAP is prescribed, it is performed without further physician involvement”. | “I do not always feel that our physiotherapeutic arguments to end CPAP and commence with another physiotherapeutic chest intervention are respected”.“Before this intervention we used another CPAP system. However, the inter-professional cooperation about respiratory insufficiency has improved”. | “The intervention has increased the cooperation with the nurses from the general wards”. |
| Focus on patients with respiratory insufficiency | “We have continually focus on respiration, but it is good we now have the possibility to perform another treatment for patients with respiratory problems”.“Patients can remain in our ward and do not need to be transferred to another ward to receive CPAP.” | “We already have great focus”.“When CPAP is prescribed I expect it to prioritised and to be initiated”. | “It is a big improvement, but we are not finished. There is a lack of focus on CPAP when it is used by nurses from the general ward. In addition, there still exist disagreement whether CPAP make a difference for patients or not.”“Many patients benefit from CPAP, but in the beginning several CPAP were initially started without benefit”. | “We only initiate CPAP in the general wards and do not see the over time effect”.“I am unable to evaluate this, as I just resent joined the RRT”. |
| Resources | “It is not more time consuming than other assignments though it can be difficult to use CPAP when other patients are calling you – the feeling of wanting to be in two places at one time …”“It is a good initiative, but it is hard to achieve another assignment. There are a lot of patients and many colleagues have left”.“Hard to manage CPAP treatment in a busy day at work” | “Sometimes when CPAP is initial before the patients are being transferred into intensive care unit, the arteria puncture has improved so noninvasive mechanical ventilation wholly or partly is unnecessary”. | “Sometimes CPAP gets deprioritised by the nurses from the general wards because they are busy with other assignments”. | “At the start of the implementation, time was an essential factor for whether CPAP was prioritised by nurses in the general ward”. |
| Lack of knowledge | “Many do not know how to use CPAP. To be conversant there is a need for further education and bedside teaching”.“We use CPAP but are not aware of the indications for CPAP and to get it initially started in time”.“We are not good at getting the CPAP started in time because we have little experience”.“It is not near everybody there have received education”“I am aware of the CPAP intervention however there has not been education in our ward”. | “Many only use CPAP for five minutes and forget to give instructions to the patient, such as to cough and variety of other techniques aimed at improving lung volumes”. | ||
This study showed that after implementation of a CPAP intervention, the staff experienced new competences, improved inter-professional cooperation and improved healthcare for the patients. However, a substantial number of staff did not feel sufficiently trained or that the intervention was well-implemented. The use of CPAP increased, and the number of patients needing transfers to the intensive care unit decreased.
Acute respiratory failure is a common acute organ failure in hospitalised patients. The recognition of clinical respiratory deterioration is frequently delayed, as is RRT activation, which may result in less favourable outcomes.1,2,4,17,18 Therefore, interventions that improve awareness and the treatment of respiratory deterioration may have a substantial impact. In this intervention, the role of the nurses from the general ward was crucial, because nurses form one of the largest groups of employees who can determine and recognise the deterioration of the patients.21
According to a prospective observational study from New Zealand, relatively few papers have examined causes for the activation of emergency teams.22 In a study from Chicago, concern about the patient was the most frequent reason (50%) for activating the RRT whereas the second most frequent (45%) was a change in the patients’ respiratory status.23 The high frequency of RRT activation for patients with respiratory insufficiency is in accordance with the results from this study.
After the intervention, fewer patients needed transfer to the intensive care unit. To our knowledge, there are no studies about equivalent use or implementation of this type of CPAP in general wards, even though a recent study described that CPAP is particularly suitable for use in general wards with no mechanical ventilators and with low staff-patient ratios.10 The study showed improved respiratory outcomes when non-invasive ventilation in the form of CPAP was administrated in general wards for 1–3h, 3 times a day. The study also found that patients in this way could stay in a less intimidating ward and the intensive care unit would have more available beds.10
Even though a lot of effort was put into the implementation of the intervention, not all staff found it well-implemented. In a review of barriers in guideline implementation, three barrier areas were identified: personal (staff knowledge, lack of self-efficacy and attitude), guideline and external factors.24 In the current study, some of the personal factors included staff from the general wards not finding themselves sufficiently trained or educated and needing further education and bedside training. They did not have the experience and did not feel competent or conversant in the use of CPAP. Half of all staff had knowledge of the guidelines and only a few of the staff had knowledge of the instructional video. The external factors in the current study were found to be time and prioritisation. Some staff experienced CPAP as time-consuming, and some commented that it was hard to have time for other assignments. Different staff groups commented on how CPAP was prioritised by other staff groups.
Even though the staff experienced CPAP to be beneficial for patients, it was challenging to implement the change in the entire organisation and the critical mass for changes, as described by Everett M Rogers, was probably not achieved.25 A more thorough implementation plan may have decreased some barriers, such as including key persons from the general wards which could have achieved agency and contributed dissemination of the intervention and changes in the attitudes and behaviour of their colleagues.24,26
The intervention became possible due the management of the RRT, physiotherapist and the general wards and by the hospital staff who were willing to accept responsibility for the change in the CPAP practise. However, most staff did not attend the formal education sessions. The RRT offered the educations sessions but it was the management in each ward who was responsible for the provision of staff education. If the education sessions set-up were different more staff might have attended. Likewise, it might be crucial how important staff, quality improvement staff and the day to day manager in each ward found the education sessions and the intervention in general.
CPAP was previously given in the traditional and sector-divided way by physiotherapist at the hospital. By using cooperation in an inter-professional approach, this intervention is an example of “Cultural competemility”.27 This is a synergistic relationship between cultural competence and cultural humility with the belief that the combined effect is greater than the sum of their separate effects and breaks with silo thinking.27 The current intervention was an example of the overall vision of the hospital, which set the patient first and has an emphasis on patient-centred care. The intervention was a new way of delivering quality in healthcare which entailed mutually beneficial collaboration. However, the study also showed the need for monitoring the implementation process and clarifying staff experiences.
Strengths and limitationsStrengths of the study include the comparison between baseline and effect assessment of RRT data in similar time periods and a broad representation of experiences as questionnaire participants consisted of RRT staff, nurses, physicians and physiotherapists with staff from all general wards at the hospital being represented. Likewise, the questionnaire included qualitative comments which elucidated the quantitative responses.
Limitations of the study include it being a single-centre study, which decreases generalisability, and the low response rates, which induce the risk of non-responder bias. Likewise, the before–after design cannot prove that the changes found in the RRT activations were due solely to the intervention. The registration practice of RRT activation may entail information bias, as the intensive care nurse who had responded to the RRT activation did the registration. The registered data were, therefore, collected by several intensive care nurses. It would have improved this study if quantitative and qualitative patient data, measurements and outcomes had been included.
The questionnaire survey was developed for this intervention and therefore not thoroughly validated. Including all staff whether they had participated in the education sessions or not provides a realistic picture of how well the intervention has been implemented, but it reduces the survey's ability to evaluate the actual intervention. The survey did not differentiate whether staff had received education in the “formal” education sessions or bedside by an intensive care nurse in relation to an RRT activation.
The questionnaire survey was conducted almost two years after the implementation period. Some staff who had received education in the implementation period could have left the hospital. New staff was unfamiliar with how the organisation was prior to the implementation and, therefore, had not received any formal education. It would be expected that more participants had received education if the time between the intervention period and effect assessment was shorter.
ConclusionThe intervention entailed new competences for the staff, inter-professional cooperation as well as improved system performance and healthcare for patients. However, this study has also identified the need for continuous focus on the intervention, staff education and prevention of respiratory insufficiency.
ContributorsAll authors took part in designing the study. MBK and LHG were responsible for the implementation. Data was analysed by MBK with help from LHG and HIJ. MBK had main responsibility for drafting the manuscript, and all three authors critically revised the manuscript and accepted the final version.
Conflicts of interestNo competing interest declared.
FundingThere was no funding for the implementation of the intervention. The Development Council at the hospital financed data analysis and publication of the study results.
The authors would like to acknowledge the efforts of those who took part in this study and in this project.