The pursuit of commercialization is at the core of economic activity, and limited commercialization success is generally ascribed to the lower scalability or potential of the venture. Drawing on the anti-profit-taking socio-institutional perspective and innovation resistance theory, commercialization of a value-creating technology could be resisted from the demand side. We use a 3D surgical video technology developed at a Swedish hospital along with Potentially All Pairwise RanKings of all possible alternatives (PAPRIKA) based on conjoint analysis completed by 1437 elderly individuals. We find that, despite the value benefits for the surgeon and the overall social benefits of the technology, the most preferred part-worth utility (i.e., weight) of relative importance is a preference for not commercializing the technology for profit. These findings carry implications for entrepreneurship and institutional theory related to medical innovations in countries with universal healthcare.
The commercialization of inventions is driven by markets, entrepreneurs, venture capital, technology transfers, creative destruction, and economic geography, among others (Kirchberger & Pohl, 2016). Implicit in these theoretical discourses is the profit motive that superseded Aristotelean theory on anti-profits as a mechanism to lower perverse incentives from profits (Child, 1998). Although Thomas Aquinas and Adam Smith focused on labor as a value of exchange, the Schumpeterian logic of commercialization is explicitly linked to profit taking (Child, 1998). Whether the implicit notion of profit taking represents a challenge in certain socio-institutional contexts is an important consideration and is distinct from non-profit organizations delivering public goods and social services where market failure occurs (Beaton & Dowin Kennedy, 2021) and from the social entrepreneurship literature that has focused on profit taking to ensure sustenance (Dacin et al., 2010; Langley et al., 2017). We take a socio-institutional perspective on an early stage of innovation to highlight whether profit-taking implications are a core concern of value-creating inventions (Haeussler, 2011; Leydesdorff, 2013).
We ask whether demand-side individuals in a universal health care system approve or oppose the commercialization of technology with underlying health and social benefits. We use the context of 3D surgical video recording technology in seeking to understand the feasibility of developing an open-source platform hosting 3D surgical videos of the elderly. The platform, with videos only accessible to patients, is useful because it provides a full medical record and allows surgeons to revisit their surgical actions. Elderly patients can carry their medical history anywhere in the world so that other doctors and surgeons can readily access their detailed medical records. The anonymized collections of surgical videos allow medical professionals to develop learning tools to improve surgical skills, provide learning opportunities for medical students, and develop artificial learning algorithms in the future to understand and improve surgical performance. The 3D surgery data are especially important for the elderly who suffer from a multitude of co-morbidities, and the availability of shared data allows any physician or surgeon to understand the prior history of the patient more fully, lessen errors, and enhance patient well-being.
Although the economic and social benefits of the technology are clear, commercialization of the technology may not be desired by the demand side for socio-institutional reasons. The Swedish universal health care system may imbue values and norms that lead individuals to consider commercialization a “dirty” word. Colloquial evidence in the news media has highlighted this perspective for the universal healthcare system in the UK, the NHS (Mackintosh & Koivusalo, 2005; Sterckx & Cockbain, 2014). Commercialization is seen as incompatible with the social mission of healthcare organizations, which are generally organized as non-profits, even in countries such as the US. However, in countries with universal health care systems, reticence toward commercialization may be acute. Isomorphic forces and public good considerations may be salient in limiting preferences for commercialization (Bromley & Meyer, 2017). The unique socio-institutional context could increase norms around commercialization for profit, even to the extent of considering healthcare innovation as a moral good driven to improve society overall.
Therefore, whether demand-side participants in countries with a universal healthcare system may be averse to commercialization for profit is an important question for scholars, service providers, and policy makers (Child et al., 2015). This investigation draws on 1437 elderly individuals who participated in a pair-wise ranking conjoint analysis. Using a pilot study with surgeons and nurses, we identified eight attributes on two levels. The features focused on patient outcomes, societal concerns, trust, and privacy. Despite the significant benefits of the technology and its associated platform that were acknowledged by the respondents, we find that commercialization for profit was significantly and negatively rated by the participants. The findings suggest that value creation may not be sufficient, and socio-institutional factors could act as a necessary retardant to commercialization efforts. The findings offer the following contributions.
First, the perceptual reactions of demand-side patients to commercialization in a universal health care system is an important consideration. Perceptions molded by institutional factors determine how individuals react to less familiar information about the invention and rely on prior cognitive heuristics related to the universal healthcare system to evaluate the information presented (Hietschold & Voegtlin, 2021). This study illustrates how sector-specific institutional structures may influence how people perceive healthcare commercialization. Results show that there is a significant effect of sector stereotypes (Xu, 2019) on perceptions of commercialization for profit.
Second, the study addresses how the demand-side stakeholders of preferred public goods respond to commercialization efforts (James, 1983; Weisbrod, 2009). Hospitals in universal healthcare countries rely on tax revenues and government support. In evaluating for-profit commercialization, demand-side stakeholders may be less receptive to further commercialization of health services, which they believe they are paying for indirectly through taxes. This leads on to questioning the pragmatic and moral legitimacy of such commercialization efforts (Suchman, 1995).
Third, the study aims to assess the institutional implications for the commercialization literature (Markman et al., 2009). We center our attention on a context where focusing on profit could receive a negative reaction because individuals may perceive a mismatch with their ideologies about the healthcare system (DiMaggio & Anheier, 1990). Given the potential uncertainty over the implications of the proposed 3D surgical video commercialization, individuals may rely on institution-imbued heuristics to develop their judgments and substitute their perceptions of the roles and responsibilities of the healthcare system in developing their assessment of commercialization (Guercini & Milanesi, 2020).
Fourth, with many of the healthcare systems failing to meet the needs of the uninsured in countries such as the US, universal healthcare systems are designed to avoid such market failure (Ilhan, 2013). However, such systems are subject to increased pressure to maintain service levels under conditions of reduced funding. Commercialization could provide the necessary slack to improve resource allocation and abate the decline in services. Even though stakeholders may perceive commercialization as a market mechanism that could lead to worse outcomes in the long term, commercialization is important for universal healthcare systems to consider as a means to improve efficiencies. Here, modern business models could be viewed as a way to improve financial reserves while increasing efficiency in service delivery. A somewhat hybrid organization with more porous boundaries into universal healthcare systems is worth considering.
Theoretical backgroundAlthough not directly related to our study, an additional theoretical area associated with our research is innovation resistance theory (IRT) (Ram, 1987; Ram & Sheth, 1989). IRT proposes that resistance to innovation adoption is explained by functional barriers (usage, value, and risk) and psychological barriers of tradition and image. Usage barriers refer to the access and ease of usability that improves with service usage. Value barriers are concerned with the performance-to-price value compared to comparable products. Risk barriers refer to risk in innovation. Tradition barriers signify respect for how things are traditionally done, and image barriers denote how the use of a product or service affects status and reputational concerns. In the current context, risk and tradition barriers may be the key to explaining the identified findings. Respondents may consider the technology's longer-term risks to their ability to utilize the service without the downside of commercialization and focus on traditions based on the universal healthcare system.
According to Kaur et al. (2020), customers pose both passive and active resistance. Active resistance is associated with functional barriers linked to innovation. Therefore, active resistance raises adoption and usage hurdles, which increase concerns for value and risk. Passive resistance is rooted in the psychological barriers of tradition, image, mindset, and mores associated with the utility derived from innovation. Resistance toward user innovations (Gupta & Arora, 2017) drives a variety of consumer behaviors related to consideration, purchase, and use of services.
Commercialization refers to the process of engaging in economic transactions to derive profits from inventions (Kirchberger & Pohl, 2016). Efforts at commercialization are at the core of high-growth entrepreneurship to facilitate scalable economic transactions of goods or services at a profit. The profit-making logic is central to all commercial activity and the key feature of the economic system. While the non-profit sector has gained economic expansion from the growth of commercialization, the statistics are not a persuasive indicator that non-profit organizations successfully use their resources to satisfy social needs (Khieng & Dahles, 2015; Young et al., 2002). Therefore, the following question remains: What are the costs and benefits of commercialization in non-profit social service organizations? The outcome of commercialization is yet to be systematically tested because of performance measurement complications. Theoretically, commercial revenue, which is unrestricted by external entities, provides non-profit organizations with greater autonomy and discretion in strategic management and daily operations compared to government funding and private contributions with restrictions (Calabrese, 2012). Thus, theoretically, a larger share of commercial revenue might lead to a higher level of organizational autonomy, which might generate better performance (Pfeffer & Salancik, 2003). Therefore, non-profit organizations have sufficient freedom to increase their operational reserves in the interests of financial stability, to create new programs that better serve clients, and to invest in fundraising events. Consequently, more commercial revenue might lead to better financial health and capacity, providing important foundations for healthcare organizations to achieve their missions.
Commercialization might contribute to non-profit effectiveness by impacting market competition, which promotes managerialism, professionalism, and innovation, as suggested by pro-business beliefs. Indeed, Eikenberry (2009), Roy et al. (2021), and Suykens et al. (2020) stress that organizations that marketize their major services also apply business-like approaches to management. These include business-like goals primarily focusing on revenue generation, business-like service delivery centering on business ideas and planning, business-like management including “results-focused” approaches, and business-like rhetoric creating a new linguistic environment in the organization by using more business terminology. Therefore, commercialization may lead to systematic changes, including changes in service delivery, management, governance structure, and even organizational culture.
Whether commercialization efforts can lead to effectiveness is questionable because commercialization may present conflicting narratives on value creation with a potential clash between “selfish motives of profit-seeking firms [and] outcomes that are valued by society” (Bhattacharjee et al., 2017, p. 673). In addition, a systematic business-like framework might help non-profit organizations gain institutional legitimacy (Dart, 2004). Although service commercialization with business-like approaches might lead to pragmatic legitimacy with its stress on organizational outcomes and performance, it can also provide commercialized non-profit organizations with a balancing moral legitimacy, which refers to “more pervasive political and ideological ideas about valid organizational models” given “contemporary social fascination with market-based solutions and mechanisms” (Dart, 2004, p. 419).
Commercialization concerns in preferred public goodsDrawing on the typologies of multi-product non-profit organizations by James (1983) and Weisbrod (2009), it can be seen that commercialization is not straightforward for organizations and institutions that are not focused on profits. The central features of universal healthcare systems are: (i) collective goods that can be priced but are not allowed to be traded; and (ii) healthcare, when provided as a private good, interferes with the received institutional norms and values. These two considerations present non-trivial implications.
Healthcare services in a single-payer system are preferred public goods because the presumption is that healthcare is a shared public good irrespective of the ability to pay (Weisbrod, 2009). Commercial behavior in universal healthcare systems signals a pivot toward the provision of healthcare as a preferred private good for a fee and conflicts with the core mission of such systems. The normalization of public good provisions is embedded in institutional structures, symbols, norms, and beliefs. The reinforced language, symbols, and heuristics related to healthcare present potential resistance to commercialization efforts. The typical argument that the provision of preferred public goods can make systems more efficient is also being challenged. The fees for goods and services by non-profits have increased (Fang et al., 2021), and the cost of healthcare insurance in the US is much higher in the online health insurance marketplaces (Rasmussen & Taylor, 2021). Concerns about negative outcomes from commercialization, such as increased prices, may limit commercialization preferences. With the quality of healthcare comparable in countries with universal healthcare (e.g., the UK) to those with a private healthcare industry (e.g., US), the perceived benefits of private market competition may be quite limited (Fry et al., 2018). Although the plausible concerns from the demand side are valid, universal healthcare systems are under growing pressure to cut costs while maintaining the same level of care. With growing calls for privatization to cut costs or collaborate with the private sector, there are increased private–public sector collaborations (Jordahl & Blix, 2021). There are growing pressures on the supply side to increase the pace of commercialization while balancing such commercialization with the core mission and values. Given the financial and policy pressures on services couched in core social values, commercialization presents significant financial gains.
Institutional perspective – demand sideIn assessing the role of commercialization, demand-side customers grapple with the role of benefits set against the moral challenges of commercializing a preferred public good – healthcare. How will the commercialization affect future cascading changes to the healthcare system, which may reduce the availability and depth of healthcare to the public? Giving consideration to a commercialization possibility against the heuristics of receiving healthcare in a universal health system could have significant implications for the perceived value of commercialization (Unger et al., 2020). The embedded socio-institutional factors usually create intangible and non-measurable perceptions of health benefits that are seen as not non-excludable and non-rivalrous – a condition that for-profit commercialization weakens.
In addition, heterogeneous needs left by the government can sometimes be satisfied by market forces because products and services related to these needs have little to no profitability, leaving private companies with little incentive to invest (Woolhandler & Himmelstein, 2007). Therefore, a growing number of non-profit organizations have been established to meet increasing demand heterogeneity in society, which is a result of globalization and individualism (Bromley & Meyer, 2017). An increasing requirement for professionalism and mission expansion stemming from market competition and policy orientations accompanies demand heterogeneity. The cases of zoos and aquariums provided by Cain and Meritt Jr (1998) suggest that the pressure of expansion, which accelerates commercialization in this field, comes from both the avoidance of species extinction and the scientific care of species preservation. The important social role that the healthcare system fulfills and the pressures it faces call for consideration of commercialization to generate revenues and, thereby, improve its ability to provide better service.
Institutional perspective – supply sideRooted in the non-profit firm literature explaining the effect of the institutional environment, this perspective suggests that “the very steady rise in commercial activity without revenue loss elsewhere can be explained by broader outside pressures and environmental influence on nonprofit overtime” (Kerlin & Pollak, 2018, p. 700). Therefore, commercialization in the healthcare sector might be initiated by professionals or firms who may prefer commercialization as the source of financial revenue. The institutional isomorphism from the broader for-profit sector may spread to healthcare leading to boundary expansion of the potentially increasing legitimacy of the supply side (Suddaby, Bitektine, & Haack, 2017).
Commercial activity promotes “a new pro-business zeitgeist” (Dees, 1998, p. 56) to improve services in an increasingly homogenous sector. Budget restrictions and performance pressures could challenge the culturally accepted principles of healthcare on the demand side and push the economic space to improve efficiency and cut costs. Neo-institutional theories also state that the pursuit of commercialization may hurt the socio-political function of the healthcare system (Eikenberry & Kluver, 2004), where increased financial focus can come at the cost of social and political capital. Commercialization could diminish the role of healthcare institutions. An increased focus on the bottom line comes with growing challenges to managing the economic logic with the “healthcare as a right” logic. The strategic trade-offs in managing the needs of the rich against the needs of the most vulnerable could enhance the prospect of backlash and lower institutional support. Commercialization may not replace the funding received by healthcare entities in universal health care systems, and growing stakeholder resentment could lower the potential gains from commercialization. Commercialization activities could lead to equity problems and could increase government and market failure.
The discussion shows that commercialization may be negatively perceived by the demand side, despite the seeming benefits of the underlying technology. Even though commercialization has value for the demand side, the potential alienation and the time and resources required to overcome strong institutional pressures could present challenges. Based on the above discussion, we propose the research question:
Hypothesis. Demand-side individuals in a universal health care system will oppose the commercialization of technology with underlying health and social benefits.
PopulationThe study targeted Swedish pensioners. The average retirement age in Sweden is 65 years, starting from the age of 62, or earlier because of sickness or disability (Lantz et al., 2020) [1]. The age group above 65 consists of 2.4 million people, 53% men and 47% women (SCB. Statistics Sweden, 2021). In the general population, 26% live in a single-adult household, 60% live in a household with their partner, and 14% live in another type of household (living with children over 25, with three generations, in a collective, or living with friends) (SCB Statistics Sweden). Among the working population, 16% work in healthcare (including dental, disability, and elderly care) (Statistics Sweden, 2020). In the general population aged 25 to 64 years, 11% did not continue their studies after primary school, 43% have a high school degree, and 46% followed higher education. The education level in the population has increased over time and, since the survey addressed seniors, earlier data could be more representative. In 2000, 21% had a primary school education, 49% possessed a high school degree, and 30% had a university degree (Statistics Sweden, 1985-2021).
Ethics statementThe study was reviewed by the Swedish Ethical Review Authority, and ethical consent was waived following consultation with the authority. Participation was voluntary, and contact details were optional for those willing to participate in follow-up interviews.
SampleParticipants in the study were recruited through the Swedish National Organization for Pensioners, PRO (Pensionärernas riksorganisation). PRO has approximately 300,000 members (approximately 12% of the population over 65). All questions and instructions were written in Swedish. The survey was sent out to all PRO members in an electronic newsletter by PRO. It remained open for a week, and no reminders were sent. In total 2750 participants (ages 18 to 95, mean 73, SD 5.4, 59% women, 41% men, < 0.1% other) started the survey, and 1437 (52%) completed the questions (ages 53 to 93, mean 73, SD 5.3, 55% women, 45% men, < 0.1% other). Most responses were given on the first day (979 completed). The trade-offs were randomly generated, with the number ranging from 11 to 25 (mean 15.3, SD 0.8). The completion time ranged from 1 min to 4.5 h, and the average time to complete the questions was 6.4 minutes (median 5 minutes, SD 9.4 min).
Among the 1437 participants who completed the study, 15% had a primary school education, 34% had a high school education, and 52% had a university degree. This group had a higher education level than the general population, especially compared to two decades ago. Most participants, 57%, lived in a two-person household, 41% lived alone, and 2% lived together with two or more persons. In this group, 15% had worked in healthcare or medical fields, including pharmaceuticals and medical technology, which is comparable to the general population. During the last 12 months, 92% of participants had visited a hospital or healthcare facility, and 25% had visited a doctor more than five times. In total, 91% had received surgery at some point, 43% in the last 1 to 5 years, and 16% during the last 12 months.
Non-completionAmong the 1313 participants who did not complete the survey, 28% did not answer a single question, and 50% had stopped after 3 trade-offs. In this group, 19% had worked in healthcare, and the education level was slightly lower than in the group that completed the survey: 19% had a primary school education, 37% had a high school degree, and 47% had a university degree.
Methodology conjoint analysisTo test for the preferences of the 3D surgical video recording, we used partial profile conjoint analysis.
Pilot studyThe survey format was evaluated in a pilot study with 7 participants recruited from the staff at Children's Heart Center. The survey in the pilot study included 20 attributes. The feedback from the participants was that the survey was too long. To limit the number of questions, the attributes was reduced to 8. The attributes were selected with the focus on the quality of patient care and how the technology could impact the work of the surgeon or the healthcare system. Attributes that were irrelevant to a universal healthcare system, such as questions concerned with health insurance and liability, or questions related to technology, such as the use of video in computer vision applications, were excluded.
Conjoint analysis features. Based on the feedback and a desire to manage cognitive load in making decisions, we narrowed the field to a list of eight features: (i) patient safety: improves/worsens; (ii) the use of video for commercial gains: should not be allowed/should be allowed; (iii) trust in caregivers: increases/decreases; (iv) the surgeon's willingness to perform difficult operations: increases/decreases; (v) the stress level of the surgeon during surgery: decreases/increases; (vi) societal cost indirectly increases for surgical complications: decreases/increases; (vii) the protection of patient integrity: improves/worsens; and (viii) the skill of the surgeon: decreases/increases.
The features can be classified into three main categories: i) patient outcomes; ii) societal concerns; and iii) trust and privacy concerns. 3D surgical video recording could affect patient outcomes by increasing patient safety, improving surgeons’ willingness to complete complex operations, placing stress on surgeons during surgery, and influencing the skills of the surgeon. Related to patient safety, recording not only allows for activity to be documented during surgery but it improves recall. It also allows the surgeon to revisit the video several months after the surgery. In cases where patients change their care provider or surgeon, the video can provide additional details of the surgical procedure. Recording videos could influence a surgeon's willingness to perform complex procedures. More complex procedures involve higher risks, and a recording could dissuade surgeons from undertaking more complex surgeries due to liability and reputational concerns. Similarly, surgeons indicated that live recording in the operation room could further exacerbate stress during surgery. Finally, a recording could act as a basis for improving skills because surgeons can revisit their videos and identify points for improvement.
The second set of features focuses on societal concerns. The features include the use of video for commercial gain and the societal costs of surgical complications. Whether the videos could be commercially exploited is a matter of significant concern because the profit motive could exclude patients unable to afford care. Sweden has a universal healthcare system, and commercialization concerns may stem from the ingrained presumption of healthcare as a not-for-profit system. Furthermore, video recordings present ambiguous social outcomes. On the one hand, video recordings could allow for systemic improvements in health outcomes because they create an ecosystem of knowledge and skill development that could help improve overall health outcomes. The additional transparency from the features further adds to an overall lowering of societal costs.
The third set of features focused on trust and privacy concerns. The recording of surgical videos could be seen as a potential infringement of patient privacy, despite anonymization, based on concerns that protections could be breached and patient information revealed. In spite of these privacy concerns, added transparency and accountability from videos could increase trust in healthcare providers. However, recordings can create an environment of mistrust because they make healthcare provision more transactional. Healthcare providers have a greater focus on patient well-being, and the zero-sum mindset is seldom prevalent in universal healthcare systems (cf. the US healthcare system, which is strongly driven by the profit motive). The use of videos could make providers feel less worthy of patient trust.
Conjoint analysis design. Rather than the full-feature conjoint design, we focus on partial-feature conjoint design. A full-feature conjoint design requires the presentation of all features at different levels. The simultaneous presentation of features produces a significant increase in the cognitive load in decision making. Thus, when presented with multiple features at the same time, the decision maker may give selective attention to certain features. The possibility of biases and cognitive shortcuts that go unobserved in such decision making could bias the inferences.
The partial-feature conjoint design presents two features at a time. Although some studies present more than two feature sets, the two-feature set design allows for a more rigorous assessment of decision making because it presents simple partial-profile questions as the simplest of all possible questions, allowing respondents to consider trade-offs between only two alternatives. Thus, confidence in their ability to answer questions and improve the validity and reliability of inferences is increased. Even though the partial conjoint design may not represent the actual decisions or choices made in real life where individuals may consider multiple features simultaneously, studies have shown that full-profile conjoint analysis is unlikely to be valid because respondents do not have confidence in their responses and represent less informed inferences (Hansen & Ombler, 2008).
The partial profile method used in the current study is the Potentially All Pairwise RanKings of all possible Alternatives (PAPRIKA) method (Hansen & Ombler, 2008). By presenting all possible combinations of choices in pairs, the method computes part-worth utilities (weights) generated for each participant compared to other conjoint analysis methods that produce aggregate data. The method allows respondents to provide their preferences on the relative importance of the criteria or attributes of interest for the decision or choice at hand by pairwise comparing (ranking) alternatives. In the current analysis, even a pairwise ranking with eight features and two levels per attribute requires pairwise rankings of 28, making pairwise rankings not humanly possible. The PAPRIKA method resolves this problem by presenting a small fraction of potentially millions or billions of undominated pairs “identifying (and eliminating) all undominated pairs implicitly ranked as corollaries of this and other explicitly ranked pairs. Fundamental to the efficiency of the method is the application of the transitivity property of additive value models.” Additional details are available at www.1000minds.com.
Analysis approach – latent class analysisDue to the lack of an outcome variable to analyze the pairwise choices, we use latent class analysis (LCA). The traditionally proposed technique for analyzing pairwise rankings in PAPRIKA is cluster analysis. Latent class analysis (LCA) creates a categorical latent variable to capture the possibility that different profiles arise because there are underlying subgroups with distinct combinations of features (Brown et al., 2022; Hallquist & Wright, 2014). LCA is used to derive groups based on patterns of shared characteristics that distinguish members of one group from those of another (Vermunt & Magidson, 2004). Here, we used this approach to categorize pairwise rankings included in the drivers and risk considerations in the dataset into sub-groups. LCA goes beyond variable-centered approaches to reveal something meaningful about underlying sub-groups (i.e., co-occurrences of preferences) (Vermunt & Magidson, 2004). Furthermore, LCA can help to address methodological challenges that arise in sub-group analysis, including a high Type I error rate and low statistical power (Lanza & Rhoades, 2013).
We control for covariates to identify conditionality in classification across groups. We control for respondent characteristics including age, sex (0=male; 1=female), and education (primary education, high school education, higher education, university, post-graduate education, PhD). Since it is related to social support, we control for respondents’ living position (I live alone, with three or more people, or with two people). On usage of the health system, we control for the number of times the respondent visited a health care facility in the past 12 months (0 times; 1-2 times; 3–5 times; or more than 5 times). Finally, on prior surgery experience, we control for whether the respondent had an operation (no, never; 1–5 years ago; during the last 12 months; or more than 5 years ago). We estimated LCA using Stata 17. The models did not converge for sub-groups higher than three sub-groups. Refer to the appendix for the full results (Table A1).
ResultsIn Table 1, we present the descriptives. The mean ranking preference for the eight features is listed. The age range in the sample was from 53 to 93 years, with a mean age of 73 years. The distribution between males and females was about even, and most of the respondents had at least a high school education. The majority of respondents were living with two people (self and a partner), the visits to healthcare facilities were somewhat evenly distributed, and most individuals had an operation more than five years ago. The correlations did not systematically vary according to the controls and the eight features. Most correlations among features and controls are small. We present the distribution of features in Fig. 1 and the distribution by gender in Fig. 2. We do not find strong differences in preferences for features by gender.
Descriptives.
| N | Mean | sd | min | p25 | p50 | p75 | max | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Patient safety: improves | 1437 | 0.1650 | 0.0488 | 0.0278 | 0.1389 | 0.1667 | 0.1944 | 0.2222 | |||||
| 2 | The use of video for commercial gains: should not be allowed | 1437 | 0.1535 | 0.0707 | 0.0278 | 0.0833 | 0.1667 | 0.2222 | 0.2222 | |||||
| 3 | Trust in caregivers: increases | 1437 | 0.1439 | 0.0481 | 0.0278 | 0.1111 | 0.1389 | 0.1944 | 0.2222 | |||||
| 4 | The surgeon's willingness to perform difficult operations: increases | 1437 | 0.1431 | 0.0542 | 0.0278 | 0.1111 | 0.1389 | 0.1944 | 0.2222 | |||||
| 5 | The stress level of the surgeon during surgery: decreases | 1437 | 0.1256 | 0.0555 | 0.0278 | 0.0833 | 0.1111 | 0.1667 | 0.2222 | |||||
| 6 | Societal cost for surgical complications: decreases | 1437 | 0.1215 | 0.0530 | 0.0278 | 0.0833 | 0.1111 | 0.1667 | 0.2222 | |||||
| 7 | The protection of patient integrity: improves | 1437 | 0.1014 | 0.0487 | 0.0278 | 0.0556 | 0.0833 | 0.1389 | 0.2222 | |||||
| 8 | The skill of the surgeon: decreases | 1437 | 0.0460 | 0.0403 | 0.0278 | 0.0278 | 0.0278 | 0.0556 | 0.2222 | |||||
| 9 | Age | 1437 | 73.1322 | 5.2818 | 53 | 69 | 73 | 76 | 93 | |||||
| 10 | Sex (0=male; 1=female) | 1437 | 0.5484 | 0.4978 | 0 | 0 | 1 | 1 | 1 | |||||
| 11 | Primary school education (1=yes; 0=no) | 1437 | 0.1510 | 0.3582 | 0 | 0 | 0 | 0 | 1 | |||||
| 12 | Higher school education (1=yes; 0=no) | 1437 | 0.3410 | 0.4742 | 0 | 0 | 0 | 1 | 1 | |||||
| 13 | Higher education university (1=yes; 0=no) | 1437 | 0.5024 | 0.5002 | 0 | 0 | 1 | 1 | 1 | |||||
| 14 | Post-graduate education PhD (1=yes; 0=no) | 1437 | 0.0202 | 0.1407 | 0 | 0 | 0 | 0 | 1 | |||||
| 15 | Living situation: With three or more people (ref. I live alone) | 1437 | 0.0153 | 0.1228 | 0 | 0 | 0 | 0 | 1 | |||||
| 16 | Living situation: With two people | 1437 | 0.5734 | 0.4948 | 0 | 0 | 1 | 1 | 1 | |||||
| 17 | Times visited health care facility in 12 months: 1-2 times (ref. 0 times) | 1437 | 0.3312 | 0.4708 | 0 | 0 | 0 | 1 | 1 | |||||
| 18 | Times visited health care facility in 12 months: 3-5 times | 1437 | 0.3354 | 0.4723 | 0 | 0 | 0 | 1 | 1 | |||||
| 19 | Times visited health care facility in 12 months: more than 5 times | 1437 | 0.2547 | 0.4358 | 0 | 0 | 0 | 1 | 1 | |||||
| 20 | Had operation: Yes, 1–5 years ago (ref. no, never) | 1437 | 0.2735 | 0.4459 | 0 | 0 | 0 | 1 | 1 | |||||
| 21 | Had operation: Yes, during the last 12 months | 1437 | 0.1559 | 0.3629 | 0 | 0 | 0 | 0 | 1 | |||||
| 22 | Had operation: Yes, more than 5 years ago | 1437 | 0.4788 | 0.4997 | 0 | 0 | 0 | 1 | 1 | |||||
| (contd.) | ||||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Patient safety: improves | 1 | ||||||||||||
| 2 | The use of video for commercial gains: should not be allowed | −0.2985* | 1 | |||||||||||
| 3 | Trust in caregivers: increases | 0.044 | −0.2064* | 1 | ||||||||||
| 4 | The surgeon's willingness to perform difficult operations: increases | −0.1658* | −0.2791* | −0.1608* | 1 | |||||||||
| 5 | The stress level of the surgeon during surgery: decreases | -0.1434* | −0.3036* | −0.2400* | 0.1555* | 1 | ||||||||
| 6 | Societal cost for surgical complications: decreases | −0.1343* | −0.1116* | −0.1115* | −0.1905* | −0.1495* | 1 | |||||||
| 7 | The protection of patient integrity: improves | 0.0743* | −0.2597* | −0.0371 | −0.1257* | −0.1458* | −0.2941 | * 1.0000 | ||||||
| 8 | The skill of the surgeon: decreases | −0.2319* | 0.1071* | −0.1475* | −0.2736* | −0.2212* | −0.0066 | −0.0409 | 1 | |||||
| 9 | Age | 0.0078 | −0.031 | 0.0603* | 0.0004 | −0.0032 | 0.0035 | −0.0186 | −0.0052 | 1 | ||||
| 10 | Sex (0=male; 1=female) | 0.0013 | 0.0496 | −0.0367 | −0.0126 | 0.0324 | −0.0238 | −0.0372 | 0.0038 | −0.0771* | 1 | |||
| 11 | Primary school education (1=yes; 0=no) | −0.0323 | −0.0515 | −0.0224 | 0.012 | 0.0009 | 0.0101 | 0.0945* | 0.0115 | 0.0877* | −0.1171* | 1 | ||
| 12 | High school education (1=yes; 0=no) | −0.0025 | −0.032 | −0.0474 | −0.0131 | 0.0871* | 0.0138 | −0.0093 | 0.0065 | −0.0770* | −0.0404 | −0.2501* | 1 | |
| 13 | Higher education university (1=yes; 0=no) | 0.0291 | 0.0701* | 0.0509 | −0.0147 | −0.0789* | −0.0072 | −0.0562* | −0.0132 | −0.0096 | 0.1261* | −0.4160* | −0.7052* | 1 |
| 14 | Post-graduate education PhD (1=yes; 0=no) | −0.0177 | 0.0053 | 0.048 | 0.0244 | −0.035 | −0.0229 | −0.0193 | 0.0238 | 0.0714* | −0.0289 | −0.0605* | −0.1032* | −0.1343 |
| 15 | Living situation: With three or more people (ref. I live alone) | 0.0203 | 0.0053 | −0.0162 | 0.031 | −0.0013 | −0.0066 | −0.0398 | 0.0022 | −0.0579* | −0.0577* | −0.0209 | −0.006 | −0.0006 |
| 16 | Living situation: With two people | 0.0054 | 0.0229 | −0.0008 | −0.0173 | −0.0341 | −0.0176 | 0.037 | 0.0032 | −0.0922* | −0.2343* | 0.0101 | 0.0149 | −0.0225 |
| 17 | Times visited health care facility in 12 months: 1-2 times (ref. 0 times) | −0.0117 | −0.0082 | 0.0286 | 0.0044 | 0.0066 | −0.0286 | 0.0016 | 0.0149 | −0.0291 | 0.0148 | 0.0790* | −0.0478 | −0.0123 |
| 18 | Times visited health care facility in 12 months: 3-5 times | −0.0189 | 0.0485 | 0.0063 | −0.0137 | −0.0157 | 0.0355 | −0.0446 | −0.0227 | 0.0272 | −0.0661* | −0.0856* | 0.0393 | 0.0231 |
| 19 | Times visited health care facility in 12 months: more than 5 times | 0.0343 | −0.0396 | 0.0132 | −0.0004 | 0.013 | 0.0086 | 0.0049 | −0.0222 | 0.0102 | 0.017 | 0.0166 | 0.0007 | −0.0124 |
| 20 | Had operation: Yes, 1-5 years ago (ref. no, never) | 0.0038 | −0.0425 | 0.013 | 0.0251 | 0.0759* | −0.004 | −0.0117 | −0.0645* | 0.0071 | 0.011 | 0.0072 | −0.0297 | 0.0298 |
| 21 | Had operation: Yes, during the last 12 months | −0.0063 | −0.0197 | 0.0142 | 0.0305 | −0.0257 | 0.0154 | −0.0005 | 0 | 0.0172 | −0.0495 | −0.0151 | 0.0146 | −0.0098 |
| 22 | Had operation: Yes, more than 5 years ago | 0.0172 | 0.0570* | −0.0535* | −0.0217 | −0.0402 | −0.0052 | 0.009 | 0.0236 | −0.009 | 0.0552* | 0.0043 | 0.01 | −0.0102 |
| 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | |||||||
| 13 | Post-graduate education PhD | * 1.0000 | ||||||||||||
| 14 | Living situation: With three or more people (ref. I live alone) | 0.0627* | 1 | |||||||||||
| 15 | Living situation: With two people | 0.0137 | −0.1446* | 1 | ||||||||||
| 16 | Times visited health care facility in 12 months: 1-2 times (ref. 0 times) | 0.0041 | −0.0155 | 0.042 | 1 | |||||||||
| 17 | Times visited health care facility in 12 months: 3-5 times | 0.0029 | 0.0195 | −0.0012 | −0.5000* | 1 | ||||||||
| 18 | Times visited health care facility in 12 months: more than 5 times | 0.0183 | 0.0052 | −0.0383 | −0.4114* | −0.4153* | 1 | |||||||
| 19 | Had operation: Yes, 1-5 years ago (ref. no, never) | -0.0325 | 0.0252 | −0.0011 | −0.0437 | 0.0204 | 0.0534* | 1 | ||||||
| 20 | Had operation: Yes, during the last 12 months | 0.0202 | 0.0402 | 0.0138 | −0.1924* | 0.0076 | 0.2684* | −0.2637 | 1 | |||||
| 21 | Had operation: Yes, more than 5 years ago | 0.0111 | −0.0287 | −0.0212 | 0.1483* | −0.0082 | -0.1862* | −0.588 | −0.4119* |
Notes. *p<0.05 (two-tailed)
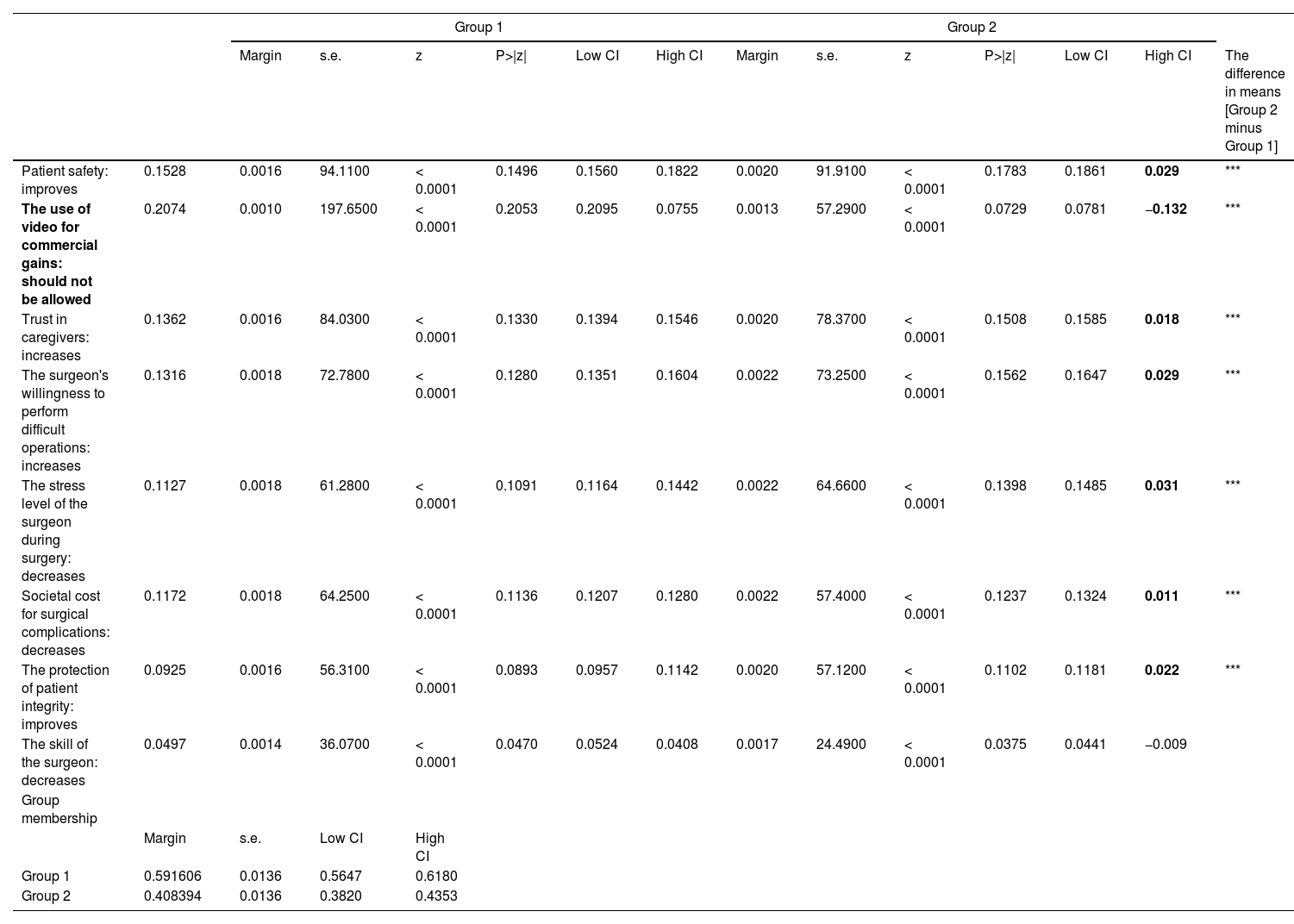
The full results with estimates for each control variable by feature for each group are presented in the appendix. We find that most of the estimates have high p-values and are generally not significant. In Table 2, we present group-wise means across features. Due to the large sample size, we do not make inferences based on small mean differences with very low p-values. In comparing the two groups, for the seven features excluding gains for commercialization, the mean differences are small (ranging from 0.01 to 0.03). However, the commercialization dimension shows a difference between the two groups. Because both groups vary little on the remaining dimensions and also have positive margin estimates, we infer little systematic variation between groups. Commercialization gains remain the highest concern, with one group (Group 1) having a stronger preference against commercialization than the other group. In summary, based on the innovation resistance theory, we find support for the proposed hypothesis.
Latent class means.
| Group 1 | Group 2 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Margin | s.e. | z | P>|z| | Low CI | High CI | Margin | s.e. | z | P>|z| | Low CI | High CI | The difference in means [Group 2 minus Group 1] | ||
| Patient safety: improves | 0.1528 | 0.0016 | 94.1100 | < 0.0001 | 0.1496 | 0.1560 | 0.1822 | 0.0020 | 91.9100 | < 0.0001 | 0.1783 | 0.1861 | 0.029 | *** |
| The use of video for commercial gains: should not be allowed | 0.2074 | 0.0010 | 197.6500 | < 0.0001 | 0.2053 | 0.2095 | 0.0755 | 0.0013 | 57.2900 | < 0.0001 | 0.0729 | 0.0781 | −0.132 | *** |
| Trust in caregivers: increases | 0.1362 | 0.0016 | 84.0300 | < 0.0001 | 0.1330 | 0.1394 | 0.1546 | 0.0020 | 78.3700 | < 0.0001 | 0.1508 | 0.1585 | 0.018 | *** |
| The surgeon's willingness to perform difficult operations: increases | 0.1316 | 0.0018 | 72.7800 | < 0.0001 | 0.1280 | 0.1351 | 0.1604 | 0.0022 | 73.2500 | < 0.0001 | 0.1562 | 0.1647 | 0.029 | *** |
| The stress level of the surgeon during surgery: decreases | 0.1127 | 0.0018 | 61.2800 | < 0.0001 | 0.1091 | 0.1164 | 0.1442 | 0.0022 | 64.6600 | < 0.0001 | 0.1398 | 0.1485 | 0.031 | *** |
| Societal cost for surgical complications: decreases | 0.1172 | 0.0018 | 64.2500 | < 0.0001 | 0.1136 | 0.1207 | 0.1280 | 0.0022 | 57.4000 | < 0.0001 | 0.1237 | 0.1324 | 0.011 | *** |
| The protection of patient integrity: improves | 0.0925 | 0.0016 | 56.3100 | < 0.0001 | 0.0893 | 0.0957 | 0.1142 | 0.0020 | 57.1200 | < 0.0001 | 0.1102 | 0.1181 | 0.022 | *** |
| The skill of the surgeon: decreases | 0.0497 | 0.0014 | 36.0700 | < 0.0001 | 0.0470 | 0.0524 | 0.0408 | 0.0017 | 24.4900 | < 0.0001 | 0.0375 | 0.0441 | −0.009 | |
| Group membership | ||||||||||||||
| Margin | s.e. | Low CI | High CI | |||||||||||
| Group 1 | 0.591606 | 0.0136 | 0.5647 | 0.6180 | ||||||||||
| Group 2 | 0.408394 | 0.0136 | 0.3820 | 0.4353 | ||||||||||
To further inform the findings, we shared our findings with the respondents. These qualitative interviews focused on eliciting the general reaction to the findings. The responses were open-ended. In Table 3, across individuals from different occupational backgrounds, we see that the empirical findings are consistent with the respondent's reactions. Most respondents are averse to the commercialization of medical technologies. This aversion does not stem from the state benefits but from the long-term snowball effects of potential increases in costs and from the institutionalized mindsets that commercialization could impinge on healthcare as a universal right.
Qualitative interviews.
| Participant id | Gender | Interview | Answers to question 1 | Question 2 | Question 3 | Comments |
|---|---|---|---|---|---|---|
| Economist | Woman 76 | 2022-09-07 14.15 | Members of PRO are left leaning and are allergic to commercialization in education and healthcare. Companies should not make money on healthcare because then the care will not be equal. | 1) Surgeon's stress level increases 2) Patient integrity decreases (d, f), in general very positive to documentation especially if it is healthcare for children, then the cost is irrelevant. | 1) Patient safety increases. 1) Surgeon's willingness to perform complex surgery increases. It is important to document and share material about difficult cases. | The study was a little bit academic and difficult to understand. |
| IT technician | Man 71 | 2022-09-07 13.15 | The seniors have not grown up with the technology and are uncertain how it works. They might be afraid to be exposed and are unsure how a company will use the material. They are not always negative to companies in the healthcare sector, such as pharmaceutical companies or companies developing vaccine, but it feels insecure to not know how the technology will be used. | 1) Surgeon's stress level increases 2) Patient integrity decreases (d, f) | 1) Patient safety increases. 2) Surgeon's skills improve. | None |
| Teacher in IT | Man 70 | 2022-09-07 14.30 | Seniors are consumers of healthcare services and have grown up in a social democratic society that was created after the Second World War. It is important not to profit from social services. There are two parts: 1) tax money should not be given to companies, and 2) personal integrity must be protected. There are of course private pharmaceutical companies and I as a patient let the healthcare providers evaluate the medical aspects. In general, I am positive towards improved documentation. It is important to have objective documentation in case something goes with the review board. I am worried about data security if this becomes common for all operations, the risk is greater that the data will leak. | 1) Surgeon's stress level increases 2) Patient integrity decreases (d, f) | 1) Trust in caregivers increases. Surgeon's willingness to perform complex surgery increases. The surgeons should be more positive to performing difficult surgeries if their work can be reviewed afterwards. | None |
| Union representative | Man 70 | 2022-09-07 14.00 | It feels insecure if the video material was sold to private companies and left the hospital. Imagine seeing an image of yourself in an ad campaign for some private healthcare provider. As long as the hospital stores the material, the trust will remain intact. Seniors are often insecure about digitalization because they feel that they do not understand the technology. I am generally positive to documentation, and the video material can be used to review the case if there is a complication. It is also good that it can be used for education. | only 1) Surgeon's stress level increases | 1) Patient safety increases. 2) Surgeon's skills improve. | None |
| Dentist, manager dental departments | Man 69 | 2022-09-08 13.00 | Our generation grew up left leaning. Commercialization in the public sector is considered wrong. Patients might worry how the commercialization will occur. Profits from tax money should be returned to citizens. | 1) Surgeon's willingness to perform complex surgery decreases. 2) Surgeon's stress level increases | 1) Patient safety increases. 2) Surgeon's skills improve. | Difficult survey, it can be difficult to answer for a normal patient. |
| Librarian | Man 80 | 2022-09-09 10.45 | PRO has an unknown network to the political left. Commercialization and profits in the public sector are considered as something negative. There is a worry about where the tax money goes. The technology is close to the patient and within the hospital and, therefore, more sensitive. I am not worried about the protection of private data, not more in this case than giving data to Facebook. There exist private elderly homes that are good, and bad of course, so private companies have their place in the system. It is about trust, we can compare it with a scientific paper, if it is financed by a company the results will be less reliable. | 1) Trust in caregivers decreases, 2) Surgeon's stress levels increase. Some people will be trusting the healthcare providers less, and some surgeons will be more stressed. | 1) Trust in caregivers increases, 2) Surgeon's stress level decreases. Some people will trust the healthcare providers more and some surgeons will be more inclined to perform difficult surgeries. | None |
| Post office worker | Woman 70 | 2022-06-20 14.00 | I think the video recordings are a sort of donation to health science. I used to work as a medical secretary The use of this contribution should primarily benefit the patients and not commercial companies. However, pharmaceutical companies are making good profit on their products that all have been developed and tested on volunteers. Could be the idea of video documentation brings along a different type of association, that you as a patient can be recognized and the connection to improved surgical care is not clear. OK, if this connection is well explained, I think most would accept the use for commercial private gain. | 1) Patient integrity decreases. 2) Increased stress to the surgeon. | 1) Patient safety increases. 2) Surgeon's skills improve. | None |
| Self-employed in the security sector | Man 71 | 2022-09-08 14.00 | I am pro development and pro research. I support all efforts that can lead to improvements. I have a background in securities for the military defense authorities and experienced firsthand the importance of research, and the need for commercial resources. The tax finance systems are not sufficiently funded to manage development. Those companies that contribute to development should get paid. Most would understand and accept some level of commercialization if it was explained to them. | 1) Trust in caregivers decreases. 2) Increased stress for the surgeon. | 1) Patient safety increases. 2) Surgeons’ skills improve. | It was fine. I liked the fact that we had to make an analytical choice. It requires creative thinking. Normally you would choose a single direction. I did get a chance to get annoyed. |
| Worked in the insurance industry | Woman 70 | 2022-09-08 15.00 | I am pro development. Private initiatives and funding are necessary. I used to work at management level in an insurance company and was the chair of PRO for 3 years. I believe skepticism about commercialization is a matter of communication. 15% of the PRO members do not have access to modern communication technology such as the internet. Probably, many of these and other members also are afraid of being used and conned. Most would agree to commercialization if it was explained to them that this way of funding research and development is necessary. | 1) Patient safety decreases. 2) Societal cost increases. | 1) Stress level for the surgeons decreases. 2) Societal cost decreases. | None |
| Librarian | Woman 73 | 2022-09-08 16.00 | I know that I am contradicting myself. I have a coronary stent and the development of this stent would not have been possible without commercial partners, companies, and they need their profit. But in Swedish society with tax-funded welfare we want to believe that development should be directed by scientific goals and not monetary gains. The negative feeling about commercial gains is not rational, but still it is difficult to accept it, probably because of the society that we live in, where the state has taken large responsibility and is the main provider of welfare, including education, healthcare. I used to work as a librarian. | 1) Surgeons stress level increases (it is not good for me as a patient). 2) Societal cost increases. | 1) Surgeon's skills increase (good for me as a patient). 2) Societal cost decreases. | None |
| Medical secretary | Woman 77 | 2022-09-09 10.30 | I think that all profit should go back to the system, the hospital, research institution. Commercial gains should be allowed, but the private companies cannot count on taking all the profit. The share profit should be based on the amount of contributions made by the different parties. I mean, without the doctors and the patients, no videos would be recorded. One cannot claim that the video recording would have been done anyways as a daily routine. Yes, maybe, still there is work effort by the healthcare staff and voluntary contributions by the patients involved. Maybe 70% to the hospitals and 30% to the companies could be a good fair deal. I used to work as a medial secretary (78 y o). | 1) Surgeon's willingness to perform complex surgery decreases. 2) Stress level for surgeon increases. | 1) Stress level for the surgeons decreases. 2) Surgeon's skills improve. | None |
The findings appear to show that the preferred public good is in a dominant position over the benefits of technological gains from commercialization. Recipients of technology benefits consider “non-profitness” a strong criterion in their preferences concerning the use of technology and its potential to improve health outcomes. Although the technology is not a life-saving technology, it is critical in lessening errors and improving surgical outcomes. The profit-seeking motives in a universal healthcare system could generate a negative impression and undermine the organization's image. With growing pressure to improve efficiency and cut costs in such systems, policy makers and innovators in the healthcare ecosystem should consider the potential negative implications from the perspective of demand-side stakeholders.
Much of the theoretical base on which we build is derived from the sustainability and non-profit literature. In the current context, a similar challenge is profit seeking. The profit-seeking theory focuses on the value of the commercialization of goods and services to create value and sustain organizations (Schaltegger & Hörisch, 2017). However, for entities traditionally locked in the institutional iron cage, commercialization comes with its own set of challenges in managing legitimacy and meeting expected social norms and obligations. The melding of commercial and social goals presents commercialization challenges as demand tries to reconcile the non-economic roles with economic roles.
The findings add to the ongoing literature on the commercialization challenges in making even a limited move toward acceptance of a role for profit making. Although medical innovation is a large industry and its innovations have a significant impact on healthcare outcomes, our study, which is based on a type of service, finds limited benefits of such commercialization efforts. The findings can be interpreted through the lens of expectancy violation theory (EVT), which focuses on violations of expectations in a range of contexts including organizational settings (Rhee & Haunschild, 2006). Potential deviations from existing expectations result in stronger negative re-evaluations of that entity (Dequech, 2013). For service providers in the universal healthcare system, this may be an important consideration as they consider re-evaluation of their business models through commercialization. Health service in the universal healthcare system is, to an extent, considered a moral good. Very limited deviation by any of the control variables shows that commercialization represents strong expectation violations that may collectively lead to lower moral reputation through increased commercial engagement.
Managerial implicationsBased on Turco (2012), the challenge in accepting commercialization is based on the perception of encroachment on a deeply personal space of “healthcare as a right” in Sweden. A variety of forms, strategies, and market mechanisms conceived through efforts to commercialize combine in a variety of ways to develop mental frames of interpretation (Yue et al., 2019). In the current study, the results show the proposed commercialization effort as a “deviant case” (Ragin & Becker, 1992) where, despite the feasibility of the innovation, commercialization is not desired. Moreover, the findings may be culture specific. In Sweden, the law of Jante refers to the egalitarian Nordic value system where it is “unworthy and inappropriate any behavior that is not conforming, does things out of the ordinary or is personally ambitious.” Respondents from the older generation may consider commercialization as a violation of Jante norms. Although it may be a plausible explanation, it does not explain the vibrant entrepreneurial ecosystem in Sweden. Future studies could focus on the role of generational effects on how individuals may differ in their valuations of innovations in the healthcare system.
We do not regard the findings of this study as a hurdle to commercialization but rather as a step toward enhanced consideration of important issues in medical commercialization in Sweden. The findings demonstrate that, for elderly patient stakeholders, educational efforts promoting the benefits of commercialization could usefully be provided. Instead of projecting commercialization as a “parasitic” solution to a universal health care system, it could be projected as a “symbiotic” arrangement that can further improve the quality of healthcare. With about 20% of inhabitants over the age of 65 years accounting for an elderly care cost at 109.2 billion SEK in 2014, healthcare commercialization could be the key to cost cutting by leveraging modern technologies and machine learning.
Hospitals are not-for-profit entities attempting to commercialize to increase the effectiveness of technology transfer. It has been suggested that universities should increase the inventor's share of royalty payments to further motivate research patenting and licensing, which would reduce the revenue share to universities from commercialized inventions (Thursby & Thursby, 2011). In addition, the need for more advanced research facilities and equipment has expanded. Thus, the financial pressure to purchase research facilities might be higher for mid-size universities who are often eager to survive in the technology transfer market. Furthermore, the investment costs associated with maintaining a professional TTO are unavoidable and essential for successful academic entrepreneurship, especially the critical role played by these administrative offices designed specifically for patenting and licensing activities (Grimaldi et al., 2011). Finally, the aforementioned burden might become more stressful because failure in meeting these demands might lead to the loss of valuable faculty members who choose to move to other universities with more friendly organizational and institutional environments for academic entrepreneurship.
Limitations and directions for future researchThe findings of this study must be interpreted in the light of its limitations. First, our partial conjoint analysis used in the current study provides greater confidence to the user on the validity of the preferences. However, it comes at the expense of considering all the features in tandem. In a research setting, the confidence in such evaluations will be lower. However, alternative methods demonstrating post-surgery usefulness could yield different results. Second, a focus on healthcare as a public good and a recognition of the implicit right of citizens to receive health care are at the core of Swedish social institutions. The findings may, therefore, not be generalizable and, in the US context – which is based on a more commercialized health care system – the effects may be distinct. Third, we draw on data from the demand side, and the features for the conjoint analysis were identified in concert with surgeons and nurses. However, the study could be extended by basing it on a joint discussion among stakeholders to negotiate a potential solution that ensures the benefits of the technology but also lowers short-term and long-term commercialization concerns.
In conclusion, we hope that our findings provide further insights into the socio-institutional systems that influence technology considerations in a preferred public good setting. Although profit making and scaling are at the core of commercialization efforts, demand-side concerns on profit making may significantly affect commercialization efforts. In contrast to the Schumpeterian notion that commercialization is strongly market driven, the non-economic considerations are based on Nicomachean ethics on the importance of a universal conception of the good life.
Latent class analysis full estimates by group and control variables.
| Group 1 | Group 2 | ||||||||
| Patient safety: improves | |||||||||
| Coefficient | sd | z | p-value | Coefficient | sd | z | p-value | ||
| Age | 0.0001 | 0.0001 | 0.8700 | 0.3850 | 0.0001 | 0.0002 | 0.3200 | 0.7460 | |
| Sex (0=male; 1=female) | 0.0029 | 0.0017 | 1.7200 | 0.0850 | −0.0039 | 0.0024 | −1.6000 | 0.1100 | |
| Primary school education (1=yes; 0=no) | 0.0037 | 0.0045 | 0.8400 | 0.4030 | −0.0018 | 0.0075 | −0.2500 | 0.8060 | |
| High school education | 0.0040 | 0.0045 | 0.9000 | 0.3690 | −0.0104 | 0.0075 | −1.3900 | 0.1660 | |
| Higher education university | 0.0042 | 0.0046 | 0.9200 | 0.3590 | −0.0091 | 0.0076 | −1.2000 | 0.2290 | |
| Post-graduate education PhD | 0.0113 | 0.0071 | 1.5800 | 0.1150 | −0.0171 | 0.0099 | −1.7400 | 0.0820 | |
| Living situation: With three or more people (ref. I live alone) | 0.0069 | 0.0062 | 1.1100 | 0.2680 | 0.0141 | 0.0083 | 1.7100 | 0.0880 | |
| Living situation: With two people | −0.0007 | 0.0017 | −0.4000 | 0.6860 | −0.0004 | 0.0024 | −0.1500 | 0.8770 | |
| Times visited health care facility in 12 months: 1-2 times (ref. 0 times) | −0.0016 | 0.0031 | −0.5200 | 0.6020 | −0.0021 | 0.0045 | −0.4700 | 0.6360 | |
| Times visited health care facility in 12 months: 3-5 times | −0.0012 | 0.0031 | −0.3800 | 0.7060 | −0.0013 | 0.0046 | −0.2900 | 0.7740 | |
| Times visited health care facility in 12 months: more than 5 times | −0.0017 | 0.0033 | −0.5100 | 0.6100 | −0.0077 | 0.0048 | −1.5900 | 0.1110 | |
| Had operation: Yes, 1-5 years ago (ref. no, never) | 0.0017 | 0.0030 | 0.5600 | 0.5760 | −0.0030 | 0.0045 | −0.6500 | 0.5150 | |
| Had operation: Yes, during the last 12 months | 0.0042 | 0.0033 | 1.2600 | 0.2060 | 0.0010 | 0.0050 | 0.1900 | 0.8480 | |
| Had operation: Yes, more than 5 years ago | 0.0008 | 0.0028 | 0.2900 | 0.7700 | −0.0060 | 0.0043 | −1.4000 | 0.1630 | |
| Cons | 0.0923 | 0.0123 | 7.4900 | 0.0000 | 0.1975 | 0.0196 | 10.0500 | 0.0000 | |
| The use of video for commercial gains: should not be allowed | |||||||||
| Age | −0.0001 | 0.0002 | −0.4300 | 0.6710 | −.0005 | 0.0002 | −2.1700 | 0.0300 | |
| Sex (0=male; 1-female) | 0.0031 | 0.0023 | 1.3800 | 0.1680 | 0.0007 | 0.0027 | 0.2700 | 0.7840 | |
| Primary school education (1=yes; 0=no) | −0.0061 | 0.0077 | −0.7900 | 0.4270 | 0.0065 | 0.0107 | 0.6100 | 0.5420 | |
| High school education | −0.0039 | 0.0078 | −0.5100 | 0.6120 | 0.0150 | 0.0105 | 1.4200 | 0.1550 | |
| Higher education university | −0.0002 | 0.0080 | −0.0200 | 0.9830 | 0.0128 | 0.0105 | 1.2200 | 0.2230 | |
| Post graduate education PhD | −0.0020 | 0.0107 | −0.1900 | 0.8490 | 0.0321 | 0.0127 | 2.5300 | 0.0110 | |
| Living situation: With three or more people (ref. I live alone) | −0.0014 | 0.0084 | −0.1700 | 0.8690 | 0.0261 | 0.0091 | 2.8500 | 0.0040 | |
| Living situation: With two people | −0.0004 | 0.0022 | −0.1700 | 0.8630 | 0.0003 | 0.0028 | 0.1000 | 0.9200 | |
| Times visited health care facility in 12 months: 1-2 times (ref. 0 times) | −0.0022 | 0.0041 | −0.5300 | 0.5950 | −0.0017 | 0.0048 | −0.3600 | 0.7200 | |
| Times visited health care facility in 12 months: 3-5 times | −0.0020 | 0.0040 | −0.4800 | 0.6280 | 0.0061 | 0.0048 | 1.2800 | 0.2010 | |
| Times visited health care facility in 12 months: more than 5 times | −0.0038 | 0.0043 | −0.8700 | 0.3840 | −0.0033 | 0.0050 | −0.6600 | 0.5090 | |
| Had operation: Yes, 1-5 years ago (ref. no, never) | −0.0058 | 0.0041 | −1.4200 | 0.1550 | −0.0102 | 0.0047 | −2.1500 | 0.0320 | |
| Had operation: Yes, during the last 12 months | −0.0021 | 0.0046 | −0.4600 | 0.6450 | −0.0073 | 0.0052 | −1.4100 | 0.1590 | |
| Had operation: Yes, more than 5 years ago | −0.0020 | 0.0038 | −0.5200 | 0.6060 | −0.0018 | 0.0043 | −0.4100 | 0.6790 | |
| Cons | 0.2198 | 0.0175 | 12.6000 | 0.0000 | 0.1027 | 0.0208 | 4.9300 | 0.0000 | |
| Trust in caregivers: increases | |||||||||
| Age | 0.0006 | 0.0003 | 1.9000 | 0.0580 | 0.0004 | 0.0004 | 0.9700 | 0.3300 | |
| Sex (0=male; 1=female) | −0.0012 | 0.0035 | −0.3300 | 0.7390 | −0.0047 | 0.0041 | −1.1300 | 0.2570 | |
| Primary school education (1=yes; 0=no) | −0.0048 | 0.0132 | −0.3700 | 0.7140 | 0.0213 | 0.0164 | 1.3000 | 0.1940 | |
| High school education | −0.0047 | 0.0134 | −0.3500 | 0.7270 | 0.0220 | 0.0162 | 1.3600 | 0.1740 | |
| Higher education university | 0.0043 | 0.0138 | 0.3100 | 0.7550 | 0.0261 | 0.0162 | 1.6100 | 0.1070 | |
| Post-graduate education PhD | 0.0204 | 0.0184 | 1.1100 | 0.2670 | 0.0239 | 0.0202 | 1.1900 | 0.2360 | |
| Living situation: With three or more people (ref. I live alone) | 0.0157 | 0.0141 | 1.1100 | 0.2670 | −0.0376 | 0.0152 | −2.4600 | 0.0140 | |
| Living situation: With two people | 0.0026 | 0.0035 | 0.7500 | 0.4540 | −0.0048 | 0.0042 | −1.1500 | 0.2520 | |
| Times visited health care facility in 12 months: 1-2 times (ref. 0 times) | 0.0133 | 0.0066 | 2.0300 | 0.0430 | 0.0214 | 0.0076 | 2.8200 | 0.0050 | |
| Times visited health care facility in 12 months: 3-5 times | 0.0159 | 0.0066 | 2.4100 | 0.0160 | 0.0138 | 0.0077 | 1.7900 | 0.0730 | |
| Times visited health care facility in 12 months: more than 5 times | 0.0125 | 0.0070 | 1.7900 | 0.0730 | 0.0197 | 0.0080 | 2.4700 | 0.0140 | |
| Had operation: Yes, 1-5 years ago (ref. no, never) | −0.0064 | 0.0065 | −0.9900 | 0.3220 | -0.0105 | 0.0073 | −1.4400 | 0.1490 | |
| Had operation: Yes, during the last 12 months | −0.0125 | 0.0072 | −1.7300 | 0.0840 | −0.0035 | 0.0081 | −0.4300 | 0.6650 | |
| Had operation: Yes, more than 5 years ago | −0.0094 | 0.0060 | −1.5600 | 0.1180 | −0.0138 | 0.0068 | −2.0300 | 0.0420 | |
| Cons | 0.0851 | 0.0284 | 3.0000 | 0.0030 | 0.1037 | 0.0332 | 3.1300 | 0.0020 | |
| The surgeon's willingness to perform difficult operations: increases | |||||||||
| Age | 0.0000 | 0.0004 | 0.0200 | 0.9820 | −0.0002 | 0.0004 | −0.3800 | 0.7050 | |
| Sex (0=male; 1=female) | −0.0083 | 0.0039 | −2.1300 | 0.0330 | 0.0093 | 0.0046 | 2.0200 | 0.0440 | |
| Primary school education (1=yes; 0=no) | −0.0004 | 0.0144 | −0.0300 | 0.9780 | -0.0359 | 0.0182 | −1.9700 | 0.0490 | |
| High school education | 0.0012 | 0.0146 | 0.0800 | 0.9370 | −0.0452 | 0.0179 | −2.5300 | 0.0120 | |
| Higher education university | −0.0012 | 0.0150 | −0.0800 | 0.9360 | −0.0378 | 0.0180 | −2.1000 | 0.0360 | |
| Post-graduate education PhD | 0.0245 | 0.0200 | 1.2300 | 0.2200 | −0.0471 | 0.0222 | −2.1200 | 0.0340 | |
| Living situation: With three or more people (ref. I live alone) | −0.0022 | 0.0156 | −0.1400 | 0.8870 | 0.0159 | 0.0170 | 0.9400 | 0.3490 | |
| Living situation: With two people | 0.0009 | 0.0038 | 0.2400 | 0.8080 | −0.0033 | 0.0047 | −0.7000 | 0.4830 | |
| Times visited health care facility in 12 months: 1-2 times (ref. 0 times) | −0.0057 | 0.0073 | −0.7700 | 0.4410 | −0.0019 | 0.0084 | −0.2300 | 0.8180 | |
| Times visited health care facility in 12 months: 3-5 times | −0.0107 | 0.0074 | −1.4500 | 0.1470 | 0.0011 | 0.0085 | 0.1300 | 0.8940 | |
| Times visited health care facility in 12 months: more than 5 times | −0.0048 | 0.0078 | −0.6100 | 0.5410 | −0.0095 | 0.0088 | −1.0700 | 0.2830 | |
| Had operation: Yes, 1-5 years ago (ref. no, never) | 0.0064 | 0.0072 | 0.8900 | 0.3740 | 0.0136 | 0.0082 | 1.6600 | 0.0960 | |
| Had operation: Yes, during the last 12 months | 0.0176 | 0.0081 | 2.1800 | 0.0300 | 0.0048 | 0.0091 | 0.5300 | 0.5940 | |
| Had operation: Yes, more than 5 years ago | 0.0079 | 0.0067 | 1.1800 | 0.2380 | 0.0056 | 0.0077 | 0.7300 | 0.4620 | |
| Cons | 0.1331 | 0.0316 | 4.2200 | 0.0000 | 0.2045 | 0.0370 | 5.5300 | 0.0000 | |
| The stress level of the surgeon during surgery: decreases | |||||||||
| Age | −0.0003 | 0.0004 | −0.8400 | 0.4030 | 0.0004 | 0.0004 | 0.9800 | 0.3300 | |
| Sex (0=male; 1=female) | 0.0022 | 0.0040 | 0.5600 | 0.5740 | 0.0058 | 0.0047 | 1.2500 | 0.2120 | |
| Primary school education (1=yes; 0=no) | 0.0095 | 0.0150 | 0.6300 | 0.5280 | −0.0406 | 0.0184 | −2.2100 | 0.0270 | |
| High school education | 0.0207 | 0.0152 | 1.3600 | 0.1730 | −0.0391 | 0.0181 | −2.1600 | 0.0310 | |
| Higher education university | 0.0108 | 0.0156 | 0.6900 | 0.4890 | −0.0519 | 0.0182 | −2.8500 | 0.0040 | |
| Post-graduate education PhD | 0.0023 | 0.0206 | 0.1100 | 0.9110 | −0.0564 | 0.0224 | −2.5200 | 0.0120 | |
| Living situation: With three or more people (ref. I live alone) | −0.0303 | 0.0160 | −1.9000 | 0.0580 | 0.0291 | 0.0172 | 1.6900 | 0.0910 | |
| Living situation: With two people | −0.0019 | 0.0039 | −0.5000 | 0.6190 | −0.0024 | 0.0047 | −0.5000 | 0.6190 | |
| Times visited health care facility in 12 months: 1-2 times (ref. 0 times) | −0.0091 | 0.0074 | −1.2200 | 0.2210 | 0.0185 | 0.0085 | 2.1800 | 0.0300 | |
| Times visited health care facility in 12 months: 3-5 times | −0.0126 | 0.0074 | −1.6900 | 0.0910 | 0.0203 | 0.0086 | 2.3500 | 0.0190 | |
| Times visited health care facility in 12 months: more than 5 times | −0.0093 | 0.0079 | −1.1800 | 0.2370 | 0.0173 | 0.0090 | 1.9400 | 0.0530 | |
| Had operation: Yes, 1-5 years ago (ref. no, never) | 0.0120 | 0.0074 | 1.6100 | 0.1070 | 0.0079 | 0.0083 | 0.9500 | 0.3430 | |
| Had operation: Yes, during the last 12 months | 0.0020 | 0.0083 | 0.2500 | 0.8060 | −0.0017 | 0.0092 | −0.1800 | 0.8560 | |
| Had operation: Yes, more than 5 years ago | −0.0001 | 0.0069 | −0.0200 | 0.9840 | 0.0052 | 0.0078 | 0.6600 | 0.5070 | |
| Cons | 0.1276 | 0.0321 | 3.9800 | 0.0000 | 0.1374 | 0.0374 | 3.6700 | 0.0000 | |
| Societal cost for surgical complications: decreases | |||||||||
| Age | −0.0002 | 0.0004 | −0.6900 | 0.4930 | 0.0004 | 0.0004 | 1.0100 | 0.3140 | |
| Sex (0=male; 1=female) | 0.0023 | 0.0039 | 0.5900 | 0.5580 | −0.0072 | 0.0047 | −1.5400 | 0.1230 | |
| Primary school education (1=yes; 0=no) | −0.0021 | 0.0144 | −0.1400 | 0.8850 | 0.0285 | 0.0184 | 1.5500 | 0.1220 | |
| High school education | −0.0018 | 0.0146 | −0.1200 | 0.9010 | 0.0284 | 0.0181 | 1.5700 | 0.1170 | |
| Higher education university | −0.0075 | 0.0150 | −0.5000 | 0.6160 | 0.0347 | 0.0182 | 1.9100 | 0.0560 | |
| Post-graduate education PhD | −0.0029 | 0.0199 | −0.1500 | 0.8830 | 0.0066 | 0.0224 | 0.3000 | 0.7670 | |
| Living situation: With three or more people (ref. I live alone) | −0.0044 | 0.0158 | −0.2800 | 0.7810 | −0.0075 | 0.0170 | −0.4400 | 0.6600 | |
| Living situation: With two people | −0.0047 | 0.0039 | −1.2100 | 0.2270 | 0.0022 | 0.0048 | 0.4600 | 0.6490 | |
| Times visited health care facility in 12 months: 1-2 times (ref. 0 times) | 0.0100 | 0.0074 | 1.3400 | 0.1790 | −0.0055 | 0.0085 | −0.6400 | 0.5190 | |
| Times visited health care facility in 12 months: 3-5 times | 0.0177 | 0.0074 | 2.3900 | 0.0170 | -0.0048 | 0.0086 | -0.5500 | 0.5800 | |
| Times visited health care facility in 12 months: more than 5 times | 0.0185 | 0.0079 | 2.3600 | 0.0180 | −0.0105 | 0.0089 | −1.1800 | 0.2370 | |
| Had operation: Yes, 1-5 years ago (ref. no, never) | −0.0097 | 0.0073 | −1.3400 | 0.1820 | 0.0118 | 0.0082 | 1.4400 | 0.1500 | |
| Had operation: Yes, during the last 12 months | −0.0122 | 0.0082 | −1.5000 | 0.1330 | 0.0177 | 0.0092 | 1.9300 | 0.0540 | |
| Had operation: Yes, more than 5 years ago | −0.0053 | 0.0068 | −0.7800 | 0.4380 | 0.0066 | 0.0077 | 0.8600 | 0.3900 | |
| Cons | 0.1347 | 0.0318 | 4.2400 | 0.0000 | 0.0661 | 0.0372 | 1.7800 | 0.0750 | |
| The protection of patient integrity: improves | |||||||||
| Age | −0.0003 | 0.0003 | −1.0200 | 0.3070 | −0.0002 | 0.0004 | −0.5800 | 0.5630 | |
| Sex (0=male; 1=female) | 0.0006 | 0.0035 | 0.1600 | 0.8710 | −0.0054 | 0.0042 | −1.2900 | 0.1960 | |
| Primary school education (1=yes; 0=no) | 0.0031 | 0.0132 | 0.2300 | 0.8160 | 0.0017 | 0.0169 | 0.1000 | 0.9200 | |
| High school education | −0.0093 | 0.0134 | −0.7000 | 0.4870 | −0.0106 | 0.0166 | −0.6400 | 0.5210 | |
| Higher education university | −0.0117 | 0.0137 | −0.8500 | 0.3940 | −0.0086 | 0.0166 | −0.5200 | 0.6040 | |
| Post-graduate education PhD | −0.0214 | 0.0182 | −1.1800 | 0.2390 | −0.0064 | 0.0204 | −0.3100 | 0.7540 | |
| Living situation: With three or more people (ref. I live alone) | −0.0080 | 0.0142 | −0.5600 | 0.5760 | −0.0220 | 0.0153 | −1.4300 | 0.1520 | |
| Living situation: With two people | 0.0035 | 0.0035 | 0.9900 | 0.3210 | 0.0025 | 0.0043 | 0.5800 | 0.5630 | |
| Times visited health care facility in 12 months: 1-2 times (ref. 0 times) | −0.0101 | 0.0067 | −1.5200 | 0.1300 | −0.0127 | 0.0077 | −1.6500 | 0.0980 | |
| Times visited health care facility in 12 months: 3-5 times | −0.0119 | 0.0067 | −1.7900 | 0.0740 | −0.0146 | 0.0078 | −1.8700 | 0.0620 | |
| Times visited health care facility in 12 months: more than 5 times | −0.0150 | 0.0071 | −2.1100 | 0.0350 | −0.0045 | 0.0081 | −0.5600 | 0.5770 | |
| Had operation: Yes, 1-5 years ago (ref. no, never) | 0.0040 | 0.0066 | 0.6000 | 0.5460 | −0.0012 | 0.0074 | −0.1600 | 0.8750 | |
| Had operation: Yes, during the last 12 months | 0.0067 | 0.0074 | 0.9100 | 0.3610 | −0.0024 | 0.0082 | −0.3000 | 0.7680 | |
| Had operation: Yes, more than 5 years ago | 0.0035 | 0.0061 | 0.5700 | 0.5700 | 0.0026 | 0.0069 | 0.3700 | 0.7090 | |
| Cons | 0.1313 | 0.0289 | 4.5500 | 0.0000 | 0.1493 | 0.0337 | 4.4300 | 0.0000 | |
| The skill of the surgeon: decreases | |||||||||
| Age | 0.0000 | 0.0003 | 0.0500 | 0.9620 | −0.0001 | 0.0003 | −0.2700 | 0.7880 | |
| Sex (0=male; 1=female) | 0.0007 | 0.0030 | 0.2300 | 0.8190 | 0.0003 | 0.0035 | 0.0800 | 0.9360 | |
| Primary school education (1=yes; 0=no) | 0.0014 | 0.0109 | 0.1300 | 0.8940 | 0.0248 | 0.0142 | 1.7500 | 0.0800 | |
| High school education | 0.0000 | 0.0111 | 0.0000 | 0.9990 | 0.0248 | 0.0139 | 1.7800 | 0.0750 | |
| Higher education university | −0.0002 | 0.0114 | −0.0200 | 0.9860 | 0.0226 | 0.0140 | 1.6200 | 0.1050 | |
| Post-graduate education PhD | −0.0048 | 0.0154 | −0.3100 | 0.7530 | 0.0443 | 0.0173 | 2.5600 | 0.0100 | |
| Living situation: With three or more people (ref. I live alone) | 0.0120 | 0.0120 | 1.0000 | 0.3200 | -0.0066 | 0.0129 | −0.5100 | 0.6090 | |
| Living situation: With two people | −0.0014 | 0.0029 | −0.4700 | 0.6390 | 0.0022 | 0.0036 | 0.6100 | 0.5450 | |
| Times visited health care facility in 12 months: 1-2 times (ref. 0 times) | −0.0036 | 0.0056 | −0.6500 | 0.5160 | −0.0088 | 0.0064 | −1.3700 | 0.1710 | |
| Times visited health care facility in 12 months: 3-5 times | −0.0053 | 0.0056 | −0.9400 | 0.3460 | −0.0108 | 0.0065 | −1.6600 | 0.0970 | |
| Times visited health care facility in 12 months: more than 5 times | −0.0087 | 0.0060 | −1.4600 | 0.1440 | −0.0054 | 0.0068 | −0.8000 | 0.4220 | |
| Had operation: Yes, 1-5 years ago (ref. no, never) | −0.0139 | 0.0055 | -2.5300 | 0.0120 | −0.0055 | 0.0062 | −0.8800 | 0.3770 | |
| Had operation: Yes, during the last 12 months | −0.0081 | 0.0062 | −1.3200 | 0.1860 | −0.0028 | 0.0069 | −0.4100 | 0.6830 | |
| Had operation: Yes, more than 5 years ago | −0.0100 | 0.0051 | −1.9500 | 0.0510 | −0.0008 | 0.0058 | −0.1400 | 0.8900 | |
| Cons | 0.0640 | 0.0241 | 2.6500 | 0.0080 | 0.0313 | 0.0281 | 1.1100 | 0.2650 | |
| Variance | |||||||||
| Patient safety: improves | 0.0021 | 0.0001 | 0.0021 | 0.0001 | |||||
| The use of video for commercial gains: should not be allowed | 0.0007 | 0.0000 | 0.0007 | 0.0000 | |||||
| Trust in caregivers: increases | 0.0022 | 0.0001 | 0.0022 | 0.0001 | |||||
| The surgeon's willingness to perform difficult operations: increases | 0.0026 | 0.0001 | 0.0026 | 0.0001 | |||||
| The stress level of the surgeon during surgery: decreases | 0.0027 | 0.0001 | 0.0027 | 0.0001 | |||||
| Societal cost for surgical complications: decreases | 0.0027 | 0.0001 | 0.0027 | 0.0001 | |||||
| The protection of patient integrity: improves | 0.0022 | 0.0001 | 0.0022 | 0.0001 | |||||
| The skill of the surgeon: decreases | 0.0016 | 0.0001 | 0.0016 | 0.0001 | |||||
| AIC: -36647.157; BIC: -35334.849 | |||||||||
We would like to express our deepest appreciation to the nurses at Children's Heart Center, Linda Hansson and Ann-Christine Lusagnet, for their valuable feedback during the pilot study. The researchers acknowledge financial support from Kamprad Family Foundation under the project developing an open-source platform for 3D surgical data videos (Reference number 20190194).