In-hospital cardiac arrest (IHCA) has a low survival rate, so it is essential to recognize the cases with the highest probability of developing it. The aim of this study is to identify factors associated with the occurrence of IHCA.
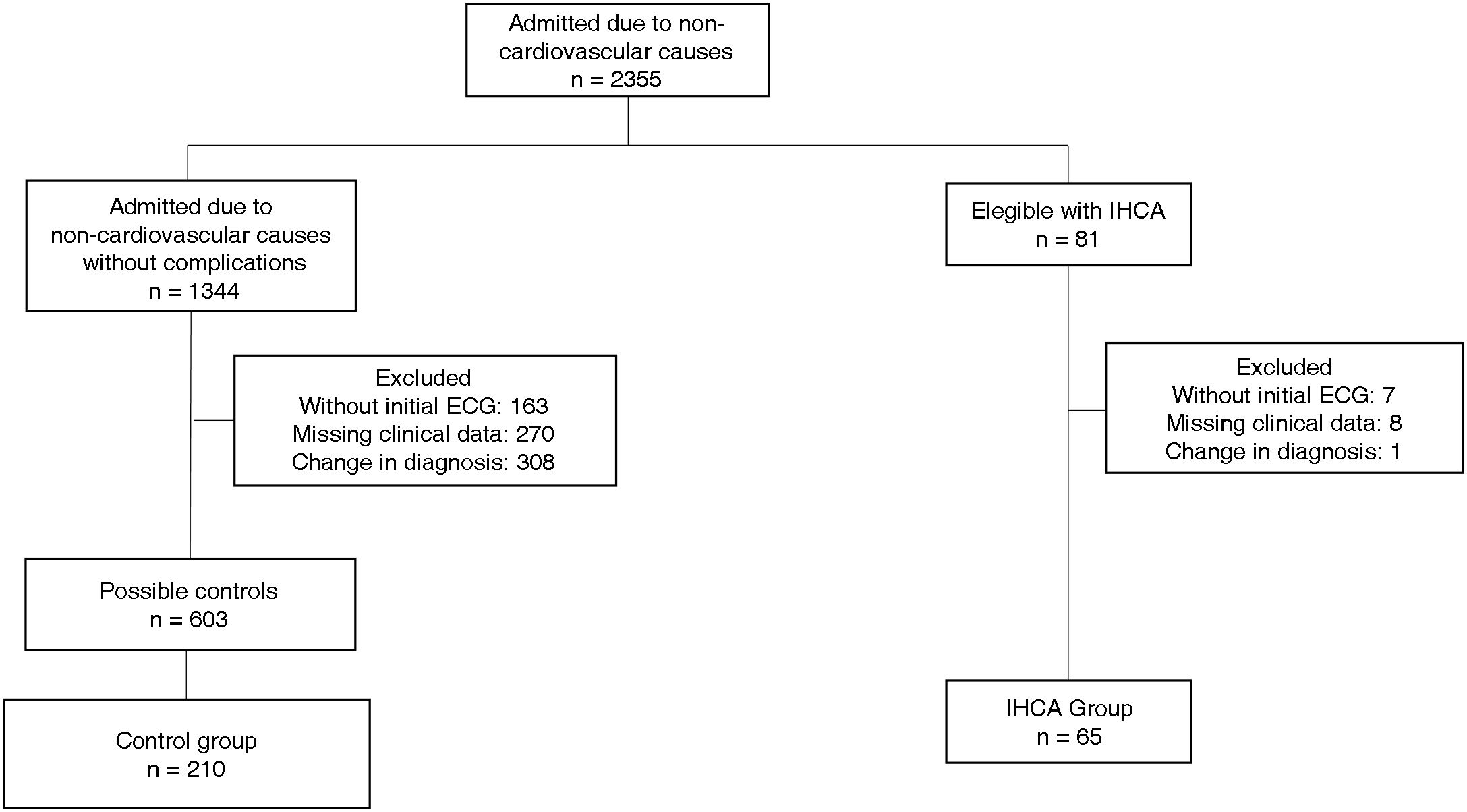
Material and methodsA single-center case-control study was conducted including 65 patients admitted to internal medicine wards for non-cardiovascular causes who experienced IHCA, matched with 210 admitted controls who did not present with IHCA.
ResultsThe main reason for admission was pneumonia. The most prevalent comorbidity was arterial hypertension. Four characteristics were strongly and independently associated with IHCA presentation, these are electrical left ventricular hypertrophy (LVH) (OR = 13.8 95% IC: 4.7–40.7), atrial fibrillation (OR = 9.4 95% CI: 4.3–20.6), the use of drugs with known risk of Torsades de pointes (OR = 2.7 95% CI: 1.3–5.5) and the combination of the categories known risk plus conditional risk (OR = 17.1 95% CI: 6.7–50.1). The first two detected in the electrocardiogram taken at the time of admission.
ConclusionIn admitted patients for non-cardiovascular causes, the use of drugs with a known risk of Torsades de Pointes, as well as the detection of electrical LVH and atrial fibrillation in the initial electrocardiogram, is independently associated with a higher probability of suffering a IHCA.
El paro cardiaco intrahospitalario (PCIH) presenta una baja tasa de supervivencia por lo que es imprescindible reconocer los casos con más alta probabilidad de desarrollarlo. El objetivo de este estudio es identificar factores asociados a la ocurrencia de PCIH.
Materiales y métodosSe realizó un estudio de casos y controles unicéntrico que incluyó 65 pacientes ingresados en salas de medicina interna por causas no cardiovasculares que sufrieron un PCIH, emparejados con 210 controles ingresados que no presentaron PCIH.
ResultadosEl principal motivo de ingreso fue la neumonía. La comorbilidad más prevalente fue la hipertensión arterial. Cuatro características se asociaron de forma independiente con la manifestación de un PCIH, estas son, hipertrofia ventricular izquierda eléctrica (OR = 13,8 95% IC: 4,7–40,7), fibrilación auricular (OR = 9,4 95% IC: 4,3–20,6), el uso de fármacos con riesgo conocido Torsades de Pointes (OR = 2,7 95% IC: 1,3–5,5) y la combinación riesgo conocido más riesgo condicional (OR = 17,1 95% IC: 6,7–50,1). Las dos primeras detectadas en el electrocardiograma tomado al momento del ingreso.
ConclusionesEn pacientes ingresados por causas no cardiovasculares el uso de fármacos con potencial para producir Torsades de Pointes así como la detección de hipertrofia ventricular izquierda y de fibrilación auricular en el electrocardiograma inicial se asocia de forma independiente a una mayor probabilidad de sufrir un PCIH.