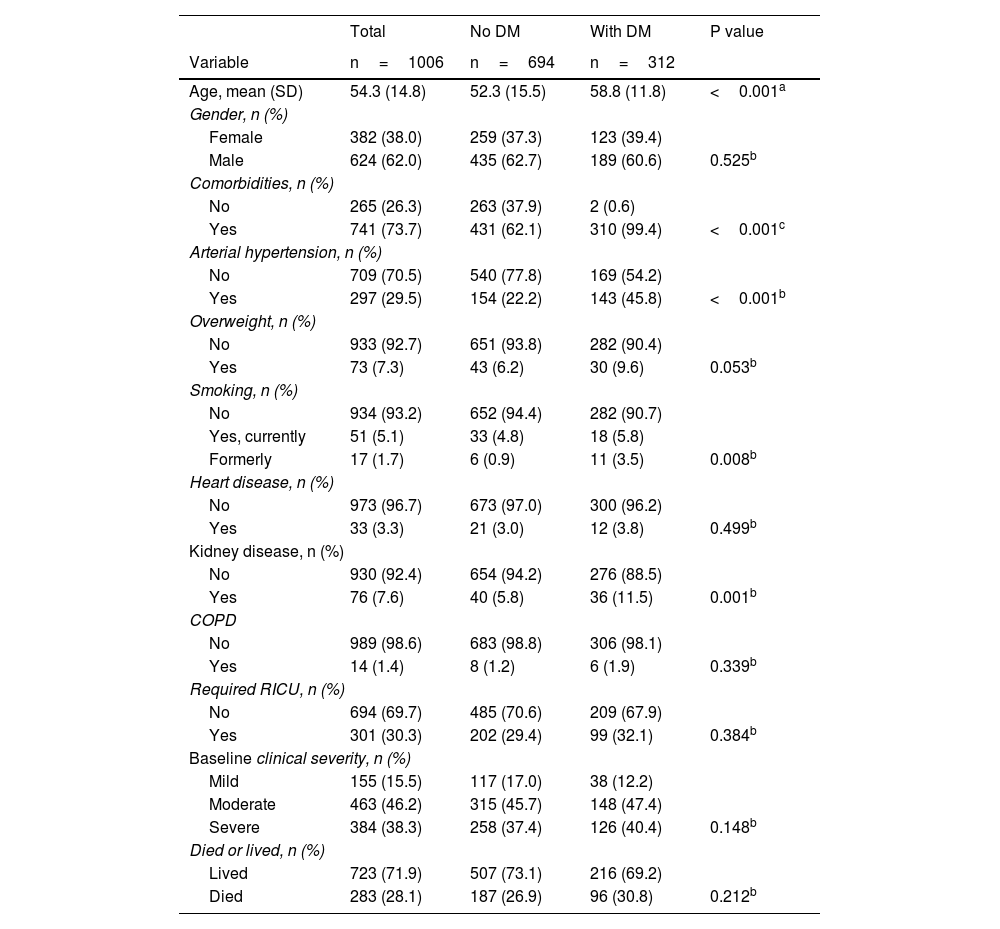
Diabetes mellitus (DM) is a public health problem in Mexico, considered an epidemiological emergency and the second leading cause of death, with an estimated cost of care of 7.7 billion dollars per year.1 Diabetes is one of the most common comorbidities in people with COVID-19, with a prevalence of 7–30%; in addition, compared to non-diabetic patients, the rate of hospital admission, severe pneumonia and mortality is higher.2 The aim of this study was to understand the impact of DM during the pandemic analysing prevalence, clinical severity and mortality. A cross-sectional study was conducted on patients>18 years old, with SARSCoV-2 infection confirmed by RT-PCR testing during the first waves of the disease, from February to June 2020, in the conventional respiratory care unit of the "Dr. Eduardo Liceaga" General Hospital of Mexico, a community health centre, following the protocols on the publication of patient data. A total of 1006 patients were included. The Mann–Whitney U test, Chi-square and Fisher's exact test were used for statistical analysis. In our series, 62% were male, mean age 52.3 and 58.8 years for the groups with absence and presence of DM, respectively; patients with DM (310) had more comorbidities (99.4%) such as systemic hypertension 143 (45.8%), chronic kidney disease 36 (11.5%) and smoking 18 (5.8%), compared to the group of people without DM (Table 1). A logistic regression model was performed, finding that patients>60 years had an OR of 2.8 (95% confidence interval [95%CI] 2.05–3.70; p<0.001) of dying from COVID-19 compared to the younger age group. The male gender presented an OR of 1.46 (95%CI 1.08–1.99; p=0.015) of dying compared to the female gender, patients with CKD presented an OR of 2.02 (95%CI 1.21–3.39; p= 0.007) of dying compared to those who did not report such disease.
Population socio-demographic and clinical characteristics according to diabetes mellitus status.
| Total | No DM | With DM | P value | |
|---|---|---|---|---|
| Variable | n=1006 | n=694 | n=312 | |
| Age, mean (SD) | 54.3 (14.8) | 52.3 (15.5) | 58.8 (11.8) | <0.001a |
| Gender, n (%) | ||||
| Female | 382 (38.0) | 259 (37.3) | 123 (39.4) | |
| Male | 624 (62.0) | 435 (62.7) | 189 (60.6) | 0.525b |
| Comorbidities, n (%) | ||||
| No | 265 (26.3) | 263 (37.9) | 2 (0.6) | |
| Yes | 741 (73.7) | 431 (62.1) | 310 (99.4) | <0.001c |
| Arterial hypertension, n (%) | ||||
| No | 709 (70.5) | 540 (77.8) | 169 (54.2) | |
| Yes | 297 (29.5) | 154 (22.2) | 143 (45.8) | <0.001b |
| Overweight, n (%) | ||||
| No | 933 (92.7) | 651 (93.8) | 282 (90.4) | |
| Yes | 73 (7.3) | 43 (6.2) | 30 (9.6) | 0.053b |
| Smoking, n (%) | ||||
| No | 934 (93.2) | 652 (94.4) | 282 (90.7) | |
| Yes, currently | 51 (5.1) | 33 (4.8) | 18 (5.8) | |
| Formerly | 17 (1.7) | 6 (0.9) | 11 (3.5) | 0.008b |
| Heart disease, n (%) | ||||
| No | 973 (96.7) | 673 (97.0) | 300 (96.2) | |
| Yes | 33 (3.3) | 21 (3.0) | 12 (3.8) | 0.499b |
| Kidney disease, n (%) | ||||
| No | 930 (92.4) | 654 (94.2) | 276 (88.5) | |
| Yes | 76 (7.6) | 40 (5.8) | 36 (11.5) | 0.001b |
| COPD | ||||
| No | 989 (98.6) | 683 (98.8) | 306 (98.1) | |
| Yes | 14 (1.4) | 8 (1.2) | 6 (1.9) | 0.339b |
| Required RICU, n (%) | ||||
| No | 694 (69.7) | 485 (70.6) | 209 (67.9) | |
| Yes | 301 (30.3) | 202 (29.4) | 99 (32.1) | 0.384b |
| Baseline clinical severity, n (%) | ||||
| Mild | 155 (15.5) | 117 (17.0) | 38 (12.2) | |
| Moderate | 463 (46.2) | 315 (45.7) | 148 (47.4) | |
| Severe | 384 (38.3) | 258 (37.4) | 126 (40.4) | 0.148b |
| Died or lived, n (%) | ||||
| Lived | 723 (71.9) | 507 (73.1) | 216 (69.2) | |
| Died | 283 (28.1) | 187 (26.9) | 96 (30.8) | 0.212b |
SD: standard deviation; COPD: chronic obstructive pulmonary disease; RICU: respiratory intensive care unit.
In our series, 143 (45.8%) patients with systemic arterial hypertension/DM accounted for 80% of comorbidities in hospitalised patients with COVID-19, with a higher risk of admission to the intensive care unit and higher mortality.
The presence of DM in COVID-19 infection is common, as we observed in 312 patients (31%) of our study; in Spain DM was found in 16.2–19.4 % of cases, in the UK in 19%, in the US in 38% and in a meta-analysis in China, the US, France and Israel in 14.34%. Uncontrolled glycaemia is a significant predictor of severity and death in patients with SARS-CoV-2, in our series 80% had glycaemia>300mg/dl and mean Hba1c>15%; in addition, diabetes was associated with increased hospitalisations (31%) and mechanical ventilation, with 148 patients having moderate (47.4%) and 126 critical (40.4%) disease, with a total of 96 deaths (30.8%).3
Overweight was found in 30 patients (9.6%), obesity has been associated with severe forms of the disease in patients with a body mass index>5, having a higher risk of hospitalisation, ICU admission and death.4 CKD due to diabetic nephropathy was associated with increased hospitalisation in 36 (11.5%) patients.
DM, systemic arterial hypertension, cardiovascular and respiratory diseases have demonstrated a correlation with higher mortality and are the main cause of disability in Mexico; DM is the leading cause of non-traumatic amputation and blindness; in our study, 30% of diabetic patients had pulmonary sequelae, thus decreasing their lung capacity. To date, it has not been possible to ensure adequate glycaemic control in patients living with DM, resulting in an increase in the years of life potentially lost attributable to premature death, despite the fact that in recent years there has been an increase in policies to adopt a balanced diet and healthy lifestyles that include daily physical activity, as well as programmes that promote the importance of self-care and raise awareness of the risks of obesity and poor diet.5
The mortality rate is high in people with chronic diseases and SARSCoV-2 (COVID-19) infection, so it is essential to have an adequate diagnosis and medical control, as well as continuing to implement prevention measures in a timely manner.
FundingThere was no participation from any funding source.
Conflict of interestNone.