Few studies have investigated the impacts of metabolic syndrome (MS) on coronavirus disease 2019 (COVID-19). We described the clinical features and prognosis of confirmed COVID-19 patients with MS during hospitalization and after discharge.
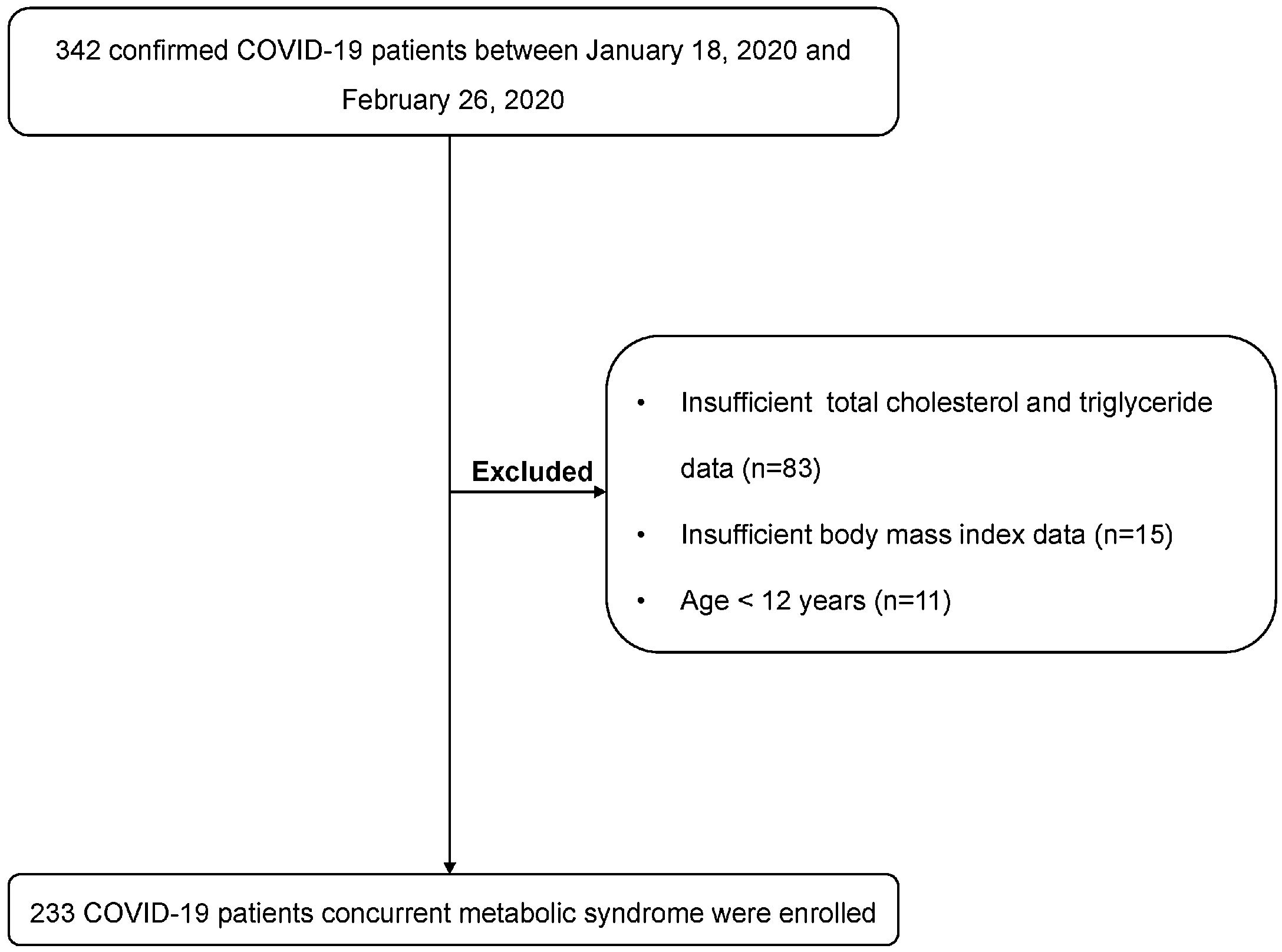
MethodsTwo hundred and thirty-three COVID-19 patients from the hospitals in 8 cities of Jiangsu, China were retrospectively included. Clinical characteristics of COVID-19 patients were described and risk factors of severe illness were analyzed by logistic regression analysis.
ResultsForty-five (19.3%) of 233 COVID-19 patients had MS. The median age of COVID-19 patients with MS was significantly higher than non-MS patients (53.0 years vs. 46.0 years, P=0.004). There were no significant differences of clinical symptoms, abnormal chest CT images, and treatment drugs between two groups. More patients with MS had severe illness (33.3% vs. 6.4%, P<0.001) and critical illness (4.4% vs. 0.5%, P=0.037) than non-MS patients. The proportions of respiratory failure and acute respiratory distress syndrome in MS patients were also higher than non-MS patients during hospitalization. Multivariate analysis showed that concurrent MS (odds ratio [OR] 7.668, 95% confidence interval [CI] 3.062–19.201, P<0.001) and lymphopenia (OR 3.315, 95% CI 1.306–8.411, P=0.012) were independent risk factors of severe illness of COVID-19. At a median follow-up of 28 days after discharge, bilateral pneumonia was found in 95.2% of MS patients, while only 54.7% of non-MS patients presented bilateral pneumonia.
Conclusions19.3% of COVID-19 patients had MS in our study. COVID-19 patients with MS are more likely to develop severe complications and have worse prognosis. More attention should be paid to COVID-19 patients with MS.
Pocos estudios han investigado el impacto del síndrome metabólico (SM) en la enfermedad por coronavirus 2019 (COVID-19). Describimos las características clínicas y el pronóstico de los pacientes con COVID-19 confirmados con SM durante la hospitalización y después del alta.
MétodosSe incluyó de forma retrospectiva a 233 pacientes con COVID-19 de los hospitales de 8 ciudades de Jiangsu (China). Se describieron sus características clínicas y se analizaron los factores de riesgo de enfermedad grave mediante un análisis de regresión logística.
ResultadosDe los 233 pacientes, 45 (19,3%) tenían EM. La mediana de edad de estos pacientes con EM fue significativamente mayor que la de los pacientes sin él (53,0 años frente a 46,0 años; p = 0,004). No hubo diferencias significativas en cuanto a los síntomas clínicos, las imágenes de TC torácica anormales y los fármacos de tratamiento entre los 2 grupos. Hubo más pacientes con EM que tuvieron enfermedades graves (33,3% frente a 6,4%; p < 0,001) y críticas (4,4% frente a 0,5%; p = 0,037) que los pacientes sin EM. Las proporciones de insuficiencia respiratoria y síndrome de dificultad respiratoria aguda en los pacientes con EM también fueron mayores que en los pacientes sin EM durante la hospitalización. El análisis multivariante mostró que la EM concurrente (odds ratio [OR] 7,668; intervalo de confianza [IC] del 95%: 3,062-19,201; p < 0,001) y la linfopenia (OR 3,315; IC del 95%: 1,306-8,411; p = 0,012) eran factores de riesgo independientes de COVID-19 grave. En una mediana de seguimiento de 28 días tras el alta, se encontró neumonía bilateral en el 95,2% de los pacientes con EM, mientras que solo la presentaron el 54,7% de los pacientes sin EM.
ConclusionesEl 19,3% de los pacientes con COVID-19 tenían EM en nuestro estudio. Los pacientes con COVID-19 y EM son más propensos a desarrollar complicaciones graves y tienen peor pronóstico. Se debe prestar más atención a los pacientes con COVID-19 y EM.