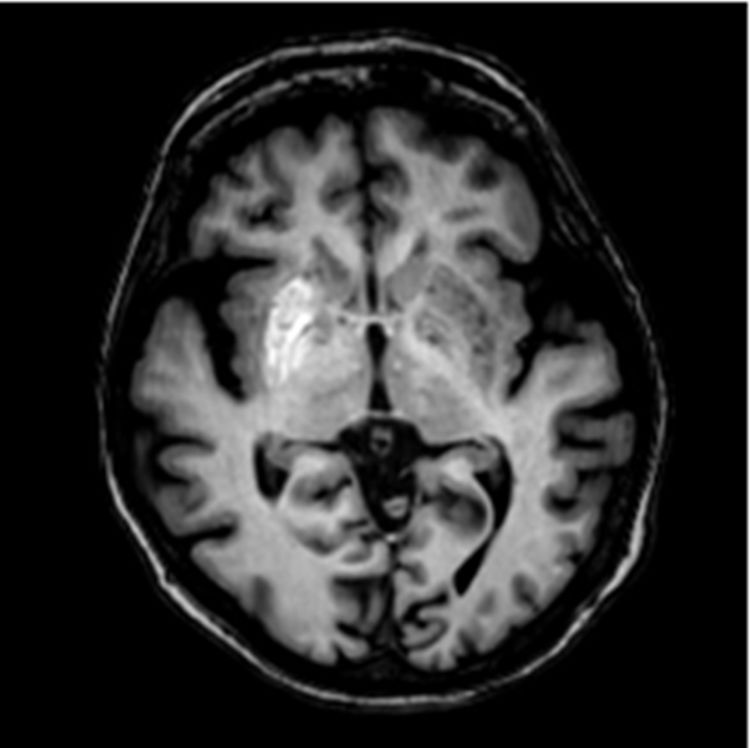
array:24 [ "pii" => "S2387020622002923" "issn" => "23870206" "doi" => "10.1016/j.medcle.2022.01.010" "estado" => "S300" "fechaPublicacion" => "2022-07-08" "aid" => "5917" "copyright" => "Elsevier España, S.L.U.. All rights reserved" "copyrightAnyo" => "2022" "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2022;159:e7-e8" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "Traduccion" => array:1 [ "es" => array:19 [ "pii" => "S0025775322000744" "issn" => "00257753" "doi" => "10.1016/j.medcli.2022.01.015" "estado" => "S300" "fechaPublicacion" => "2022-07-08" "aid" => "5917" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2022;159:e7-e8" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "es" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Carta al Editor</span>" "titulo" => "Hemicorea originada por hiperglucemia" "tienePdf" => "es" "tieneTextoCompleto" => "es" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "e7" "paginaFinal" => "e8" ] ] "titulosAlternativos" => array:1 [ "en" => array:1 [ "titulo" => "Hemichorea caused by hyperglycemia" ] ] "contieneTextoCompleto" => array:1 [ "es" => true ] "contienePdf" => array:1 [ "es" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Figura 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 748 "Ancho" => 750 "Tamanyo" => 36127 ] ] "descripcion" => array:1 [ "es" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">RM craneal con gadolinio: aumento significativo de la señal en el núcleo lenticular derecho en secuencias potenciadas en T1.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Diego Jesús Del Can-Sánchez, Juan Manuel Canelo-Moreno, Raquel Guerrero-Vázquez" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Diego Jesús" "apellidos" => "Del Can-Sánchez" ] 1 => array:2 [ "nombre" => "Juan Manuel" "apellidos" => "Canelo-Moreno" ] 2 => array:2 [ "nombre" => "Raquel" "apellidos" => "Guerrero-Vázquez" ] ] ] ] ] "idiomaDefecto" => "es" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S2387020622002923" "doi" => "10.1016/j.medcle.2022.01.010" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020622002923?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775322000744?idApp=UINPBA00004N" "url" => "/00257753/0000015900000001/v1_202206300527/S0025775322000744/v1_202206300527/es/main.assets" ] ] "itemSiguiente" => array:18 [ "pii" => "S2387020622002960" "issn" => "23870206" "doi" => "10.1016/j.medcle.2022.02.010" "estado" => "S300" "fechaPublicacion" => "2022-07-08" "aid" => "5928" "copyright" => "Elsevier España, S.L.U." "documento" => "article" "crossmark" => 1 "subdocumento" => "sco" "cita" => "Med Clin. 2022;159:56" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Image in medicine</span>" "titulo" => "Orbital filariasis" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:1 [ "paginaInicial" => "56" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Filariasis orbitaria" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:6 [ "identificador" => "fig0005" "etiqueta" => "Figure 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 883 "Ancho" => 1500 "Tamanyo" => 161494 ] ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Laura Sánchez-Vela, Marta Garrido-Marín, Bernardo F. Sánchez-Dalmau" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Laura" "apellidos" => "Sánchez-Vela" ] 1 => array:2 [ "nombre" => "Marta" "apellidos" => "Garrido-Marín" ] 2 => array:2 [ "nombre" => "Bernardo F." "apellidos" => "Sánchez-Dalmau" ] ] ] ] ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020622002960?idApp=UINPBA00004N" "url" => "/23870206/0000015900000001/v2_202301300833/S2387020622002960/v2_202301300833/en/main.assets" ] "itemAnterior" => array:19 [ "pii" => "S238702062200290X" "issn" => "23870206" "doi" => "10.1016/j.medcle.2021.12.008" "estado" => "S300" "fechaPublicacion" => "2022-07-08" "aid" => "5898" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2022;159:e5-e6" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:10 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Vocal fold palsy after vaccination against SARS-CoV-2" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "e5" "paginaFinal" => "e6" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Parálisis de cuerda vocal tras vacunación contra el SARS-CoV-2." ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Eduardo Lehrer, Sara Jubés, Jordi Casanova-Mollà" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Eduardo" "apellidos" => "Lehrer" ] 1 => array:2 [ "nombre" => "Sara" "apellidos" => "Jubés" ] 2 => array:2 [ "nombre" => "Jordi" "apellidos" => "Casanova-Mollà" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0025775322000367" "doi" => "10.1016/j.medcli.2021.12.013" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775322000367?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S238702062200290X?idApp=UINPBA00004N" "url" => "/23870206/0000015900000001/v2_202301300833/S238702062200290X/v2_202301300833/en/main.assets" ] "en" => array:16 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Hemichorea caused by hyperglycemia" "tieneTextoCompleto" => true "saludo" => "Dear Editor:" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "e7" "paginaFinal" => "e8" ] ] "autores" => array:1 [ 0 => array:4 [ "autoresLista" => "Diego Jesús Del Can-Sánchez, Juan Manuel Canelo-Moreno, Raquel Guerrero-Vázquez" "autores" => array:3 [ 0 => array:4 [ "nombre" => "Diego Jesús" "apellidos" => "Del Can-Sánchez" "email" => array:1 [ 0 => "djds22@gmail.com" ] "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">*</span>" "identificador" => "cor0005" ] ] ] 1 => array:3 [ "nombre" => "Juan Manuel" "apellidos" => "Canelo-Moreno" "email" => array:1 [ 0 => "j.m.canelo@hotmail.com" ] ] 2 => array:3 [ "nombre" => "Raquel" "apellidos" => "Guerrero-Vázquez" "email" => array:1 [ 0 => "raquel.guerrero.sspa@juntadeandalucia.es" ] ] ] "afiliaciones" => array:1 [ 0 => array:2 [ "entidad" => "Unidad de Gestión Clínica de Endocrinología y Nutrición, Hospital Universitario Virgen del Rocío, Sevilla, Spain" "identificador" => "aff0005" ] ] "correspondencia" => array:1 [ 0 => array:3 [ "identificador" => "cor0005" "etiqueta" => "⁎" "correspondencia" => "Corresponding author." ] ] ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Hemicorea originada por hiperglucemia" ] ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:8 [ "identificador" => "fig0005" "etiqueta" => "Figure 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 748 "Ancho" => 750 "Tamanyo" => 36127 ] ] "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at0010" "detalle" => "Figure " "rol" => "short" ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Cranial MRI scan performed after administering a gadolinium-based contrast agent: right lentiform nucleus with a significantly intensified signal in the T1-weighted sequences.</p>" ] ] ] "textoCompleto" => "<span class="elsevierStyleSections"><p id="par0005" class="elsevierStylePara elsevierViewall">Hyperglycemic chorea is a clinical, neurological manifestation of decompensated type-2 diabetes mellitus. The toxic effects of hyperglycemia in the basal ganglia of the brain (diabetic striatopathy) cause choreic movements in the contralateral limb, resulting in what is known as the hyperglycemic hemichorea syndrome. The prevalence of this condition if of 1/100,000 inhabitants.<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a> However, these neurological symptoms can mimic those of a cerebrovascular accident, Parkinson’s disease, or epilepsy.<a class="elsevierStyleCrossRef" href="#bib0010"><span class="elsevierStyleSup">2</span></a> Early recognition of hyperglycemic chorea enables its remission following the administration of appropriate treatment.<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a></p><p id="par0010" class="elsevierStylePara elsevierViewall">In this paper we present two cases of hemichorea caused by hyperglycemia, whose early detection and management enabled a complete resolution of this cerebral condition.</p><span id="sec0005" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0005">Case 1</span><p id="par0015" class="elsevierStylePara elsevierViewall">The first case corresponded to an 84-yearold woman who presented to the clinic with hyperglycemia of 502<span class="elsevierStyleHsp" style=""></span>mg/dl. She began experiencing involuntary, arrhythmic, non-clonic movements in her left hand and foot, occasionally together with a ballistic component. She had no fever nor an evident infectious focus, and she denied a history of trauma or epilepsy. No other neurological alterations were detected during her examination. Given the above findings, she was referred to the Emergency Care Department to be assessed by a neurologist and have a focality ruled out. A brain computed tomography (CT) scan performed at this department revealed diffuse hyperdensity in her right basal ganglia.</p><p id="par0020" class="elsevierStylePara elsevierViewall">In the Emergency Care Department, she received basal-bolus insulin therapy, achieving optimal glycemic control and almost complete resolution of the choreic movements. A magnetic resonance imaging (MRI) scan performed one month after the onset of this episode revealed a significantly increased signal in the right lentiform nucleus (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>).</p><elsevierMultimedia ident="fig0005"></elsevierMultimedia><p id="par0025" class="elsevierStylePara elsevierViewall">Subsequent follow-up check-ups showed that the patient remained neurologically asymptomatic and continued to maintain an adequate glycemic control.</p></span><span id="sec0010" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0010">Case 2</span><p id="par0030" class="elsevierStylePara elsevierViewall">The second patient was a 49-year-old man who visited the Emergency Care Department with a clinical picture of clonuses affecting his right leg, followed by typical absence seizures. He had been diagnosed with type 2 diabetes mellitus at the age of 25 and had a chronic poor metabolic control due to lack of treatment adherence. His baseline glucose levels were 490<span class="elsevierStyleHsp" style=""></span>mg/dl, without associated acidosis.</p><p id="par0035" class="elsevierStylePara elsevierViewall">A cranial CT scan was performed, initially detecting an established cerebral infarction with petechial hemorrhagic transformation. Because of these findings, the patient was admitted for further testing. A subsequent cranial MRI revealed hyperintensity in the left basal ganglia affecting both the caudate and the lentiform nucleus.</p><p id="par0040" class="elsevierStylePara elsevierViewall">Insulin therapy was intensified to correct his hyperglycemia, with the amplitude of his choreic movements decreasing after achieving an acceptable glycemic control.</p></span><span id="sec0015" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0015">Discussion</span><p id="par0045" class="elsevierStylePara elsevierViewall">The two patients described in this paper had hyperglycemic hemichorea, the most common cause of hemibalismus.<a class="elsevierStyleCrossRef" href="#bib0015"><span class="elsevierStyleSup">3</span></a> This entity is characterized by a triad of unilateral or bilateral involuntary movements, abnormal neuroimaging findings in the basal ganglia (striatal hyperdensity in a CT scan or hyperintensity in a T1-weighted MRI), and hyperglycemia. Its onset is linked to conditions of nonketonic, hyperosmolar hyperglycemia, generally with very high blood glucose levels (>300<span class="elsevierStyleHsp" style=""></span>mg/L or glycated hemoglobin [HbA1c] >14%).<a class="elsevierStyleCrossRef" href="#bib0020"><span class="elsevierStyleSup">4</span></a></p><p id="par0050" class="elsevierStylePara elsevierViewall">The pathogenic mechanism causing hyperglycemic chorea has been linked to cerebral energy metabolism alterations or ischemic damage, with biopsies revealing a loss of neurons, lysis of glial cells, and reactive astrocytosis in areas of the striate body, without associated hemorrhagic foci.<a class="elsevierStyleCrossRef" href="#bib0025"><span class="elsevierStyleSup">5</span></a> Correction of the hyperglycemia usually achieves partial or complete cessation of the movements, as well as resolution of the striatal abnormalities detected in neuroimaging studies. However, additional anti-chorea medications are sometimes required.<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a></p><p id="par0055" class="elsevierStylePara elsevierViewall">The most frequently affected structure in diabetic striatopathy is the contralateral putamen and, occasionally, the caudate nucleus and the globus pallidus. The radiological lesion specifically delineating the affected basal ganglia does not follow a vascular distribution. Hence, the typical CT image of this entity is that of hyperdensity in the contralateral striate body. An MRI scan reveals hyperintensity in the T1-weighted sequence and hypointensity in the T2-weighted sequence of the same location. Normal MRI findings have been reported within the first consecutive year following resolution of the chorea. Therefore, a generally favorable prognosis can be estimated, as these symptoms disappear in most patients after achieving glycemic correction.<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a></p><p id="par0060" class="elsevierStylePara elsevierViewall">To conclude, hemiballismus/hemichorea secondary to hyperglycemia is a neurological complication that can be seen in patients with diabetes and in which case the following aspects are considered essential for its therapeutic management: early detection, diagnosis, and treatment of the clinical picture.</p></span><span id="sec0020" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0020">Ethical considerations</span><p id="par0065" class="elsevierStylePara elsevierViewall">The work described in this paper was carried out in accordance with the code of ethics of the World Medical Association (Helsinki Declaration) concerning experiments performed on human subjects and the uniform requirements for manuscripts submitted to biomedical journals. All subjects under study provided their informed consent and all ethical procedures were implemented. The privacy rights of the subjects were respected at all times. The study was approved by the clinical research ethics committee (CREC) of University Hospital Virgen del Rocío of Seville (Spain).</p></span><span id="sec0025" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0025">Funding</span><p id="par0070" class="elsevierStylePara elsevierViewall">No financial participation was available to fund this study.</p></span></span>" "textoCompletoSecciones" => array:1 [ "secciones" => array:6 [ 0 => array:2 [ "identificador" => "sec0005" "titulo" => "Case 1" ] 1 => array:2 [ "identificador" => "sec0010" "titulo" => "Case 2" ] 2 => array:2 [ "identificador" => "sec0015" "titulo" => "Discussion" ] 3 => array:2 [ "identificador" => "sec0020" "titulo" => "Ethical considerations" ] 4 => array:2 [ "identificador" => "sec0025" "titulo" => "Funding" ] 5 => array:1 [ "titulo" => "References" ] ] ] "pdfFichero" => "main.pdf" "tienePdf" => true "NotaPie" => array:1 [ 0 => array:2 [ "etiqueta" => "☆" "nota" => "<p class="elsevierStyleNotepara" id="npar0005">Please cite this article as: Del Can-Sánchez DJ, Canelo-Moreno JM, Guerrero-Vázquez R, Hemicorea originada por hiperglucemia, Med Clin (Barc). 2022;159:e7–e8.</p>" ] ] "multimedia" => array:1 [ 0 => array:8 [ "identificador" => "fig0005" "etiqueta" => "Figure 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 748 "Ancho" => 750 "Tamanyo" => 36127 ] ] "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at0010" "detalle" => "Figure " "rol" => "short" ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Cranial MRI scan performed after administering a gadolinium-based contrast agent: right lentiform nucleus with a significantly intensified signal in the T1-weighted sequences.</p>" ] ] ] "bibliografia" => array:2 [ "titulo" => "References" "seccion" => array:1 [ 0 => array:2 [ "identificador" => "bibs0005" "bibliografiaReferencia" => array:5 [ 0 => array:3 [ "identificador" => "bib0005" "etiqueta" => "1" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "“Diabetic striatopathy”: clinical presentations, controversy, pathogenesis, treatments, and outcomes" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:6 [ 0 => "C.B. Chua" 1 => "C.K. Sun" 2 => "C.W. Hsu" 3 => "Y.C. Tai" 4 => "C.Y. Liang" 5 => "I.T. Tsai" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1038/s41598-019-56847-4" "Revista" => array:6 [ "tituloSerie" => "Sci Rep." "fecha" => "2020" "volumen" => "10" "paginaInicial" => "1" "paginaFinal" => "11" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/31913322" "web" => "Medline" ] ] ] ] ] ] ] ] 1 => array:3 [ "identificador" => "bib0010" "etiqueta" => "2" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Presentation of striatal hyperintensity on T1- weighted MRI in patients with hemiballism-hemichorea caused by non-ketotic hyperglycemia: report of seven new cases and a review of literature" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "J.-J. Lin" 1 => "G.-Y. Lin" 2 => "C. Shih" 3 => "W.-C. Shen" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1007/s004150170089" "Revista" => array:7 [ "tituloSerie" => "J Neurol." "fecha" => "2001" "volumen" => "248" "numero" => "9" "paginaInicial" => "750" "paginaFinal" => "755" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/11596778" "web" => "Medline" ] ] ] ] ] ] ] ] 2 => array:3 [ "identificador" => "bib0015" "etiqueta" => "3" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Hemiballism: revisiting a classic disorder" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "R.B. Postuma" 1 => "A.E. Lang" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/s1474-4422(03)00554-4" "Revista" => array:6 [ "tituloSerie" => "Lancet Neurol." "fecha" => "2003" "volumen" => "2" "paginaInicial" => "661" "paginaFinal" => "668" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/14572734" "web" => "Medline" ] ] ] ] ] ] ] ] 3 => array:3 [ "identificador" => "bib0020" "etiqueta" => "4" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Chorea induced by non- ketotic hyperglycaemia: a case report" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:5 [ 0 => "D. Branca" 1 => "O. Gervasio" 2 => "E. Le Piane" 3 => "C. Russo" 4 => "U. Aguglia" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1007/s10072-005-0471-0" "Revista" => array:7 [ "tituloSerie" => "Neurol Sci." "fecha" => "2005" "volumen" => "26" "numero" => "4" "paginaInicial" => "275" "paginaFinal" => "277" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/16193255" "web" => "Medline" ] ] ] ] ] ] ] ] 4 => array:3 [ "identificador" => "bib0025" "etiqueta" => "5" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Methylglyoxal, the dark side of glycolysis" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "I. Allaman" 1 => "M. Bélanger" 2 => "P.J. Magistretti" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.3389/fnins.2015.00001" "Revista" => array:6 [ "tituloSerie" => "Front Neurosci." "fecha" => "2015" "volumen" => "9" "paginaInicial" => "1" "paginaFinal" => "12" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/25653585" "web" => "Medline" ] ] ] ] ] ] ] ] ] ] ] ] ] "idiomaDefecto" => "en" "url" => "/23870206/0000015900000001/v2_202301300833/S2387020622002923/v2_202301300833/en/main.assets" "Apartado" => array:4 [ "identificador" => "43309" "tipo" => "SECCION" "en" => array:2 [ "titulo" => "Letters to the Editor" "idiomaDefecto" => true ] "idiomaDefecto" => "en" ] "PDF" => "https://static.elsevier.es/multimedia/23870206/0000015900000001/v2_202301300833/S2387020622002923/v2_202301300833/en/main.pdf?idApp=UINPBA00004N&text.app=https://www.elsevier.es/" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020622002923?idApp=UINPBA00004N" ]
Journal Information
Vol. 159. Issue 1.
Pages e7-e8 (July 2022)
Share
Download PDF
More article options
Vol. 159. Issue 1.
Pages e7-e8 (July 2022)
Letter to the Editor
Hemichorea caused by hyperglycemia
Hemicorea originada por hiperglucemia
Visits
5
Diego Jesús Del Can-Sánchez
, Juan Manuel Canelo-Moreno, Raquel Guerrero-Vázquez
Corresponding author
Unidad de Gestión Clínica de Endocrinología y Nutrición, Hospital Universitario Virgen del Rocío, Sevilla, Spain
This item has received
Article information
These are the options to access the full texts of the publication Medicina Clínica (English Edition)
Subscriber
Subscribe
Purchase
Contact
Phone for subscriptions and reporting of errors
From Monday to Friday from 9 a.m. to 6 p.m. (GMT + 1) except for the months of July and August which will be from 9 a.m. to 3 p.m.
Calls from Spain
932 415 960
Calls from outside Spain
+34 932 415 960
E-mail