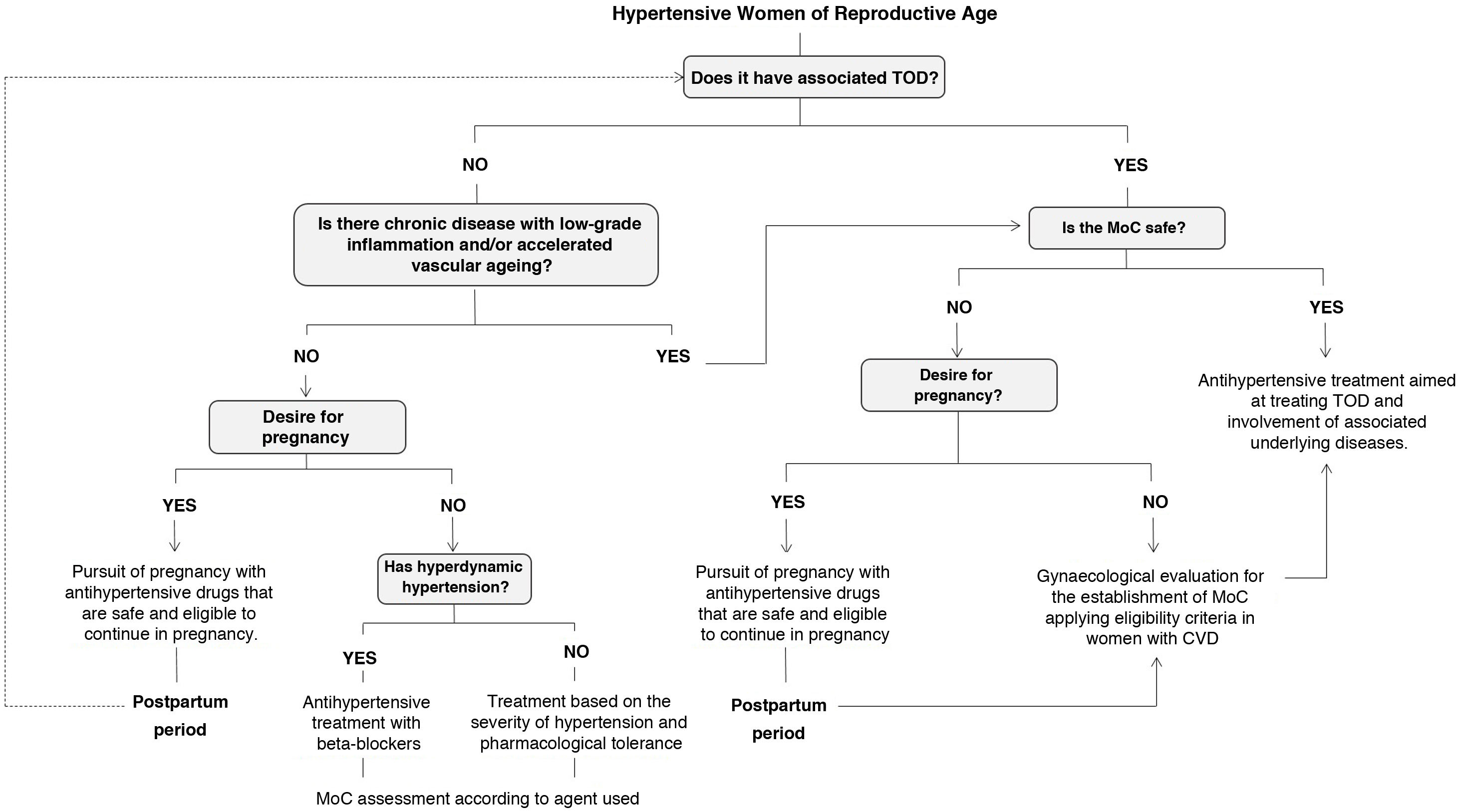
array:24 [ "pii" => "S2387020622003102" "issn" => "23870206" "doi" => "10.1016/j.medcle.2022.02.014" "estado" => "S300" "fechaPublicacion" => "2022-07-22" "aid" => "5939" "copyright" => "Elsevier España, S.L.U.. All rights reserved" "copyrightAnyo" => "2022" "documento" => "article" "crossmark" => 1 "subdocumento" => "sco" "cita" => "Med Clin. 2022;159:101-5" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "Traduccion" => array:1 [ "es" => array:19 [ "pii" => "S0025775322001361" "issn" => "00257753" "doi" => "10.1016/j.medcli.2022.02.009" "estado" => "S300" "fechaPublicacion" => "2022-07-22" "aid" => "5939" "copyright" => "Elsevier España, S.L.U." "documento" => "article" "crossmark" => 1 "subdocumento" => "sco" "cita" => "Med Clin. 2022;159:101-5" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "es" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Artículo especial</span>" "titulo" => "Hipertensión arterial en la mujer en edad fértil no gestante" "tienePdf" => "es" "tieneTextoCompleto" => "es" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "101" "paginaFinal" => "105" ] ] "titulosAlternativos" => array:1 [ "en" => array:1 [ "titulo" => "Hypertension in non-pregnant women of childbearing age" ] ] "contieneTextoCompleto" => array:1 [ "es" => true ] "contienePdf" => array:1 [ "es" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Figura 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1627 "Ancho" => 2925 "Tamanyo" => 341691 ] ] "descripcion" => array:1 [ "es" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Algoritmo de orientación para definir el esquema terapéutico antihipertensivo en mujeres en edad fértil. ECV: enfermedad cardiovascular; HTA: hipertensión arterial; LOD: lesión de órgano diana; MAC: método anticonceptivo.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Albertina M. Ghelfi, Gustavo J. Staffieri" "autores" => array:2 [ 0 => array:2 [ "nombre" => "Albertina M." "apellidos" => "Ghelfi" ] 1 => array:2 [ "nombre" => "Gustavo J." "apellidos" => "Staffieri" ] ] ] ] ] "idiomaDefecto" => "es" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S2387020622003102" "doi" => "10.1016/j.medcle.2022.02.014" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020622003102?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775322001361?idApp=UINPBA00004N" "url" => "/00257753/0000015900000002/v1_202207080542/S0025775322001361/v1_202207080542/es/main.assets" ] ] "itemSiguiente" => array:19 [ "pii" => "S2387020622003084" "issn" => "23870206" "doi" => "10.1016/j.medcle.2021.12.009" "estado" => "S300" "fechaPublicacion" => "2022-07-22" "aid" => "5899" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2022;159:e9" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:10 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Contributions from a multidisciplinary committee for the prevention of infections in patients with targeted immunosuppressive therapy" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:1 [ "paginaInicial" => "e9" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Aportaciones de un comité multidisciplinar para la prevención de infecciones en pacientes tratados con inmunosupresores selectivos" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "José Luis Callejas Rubio, María Carmen Valero Ubierna, Norberto Ortego Centeno" "autores" => array:3 [ 0 => array:2 [ "nombre" => "José Luis" "apellidos" => "Callejas Rubio" ] 1 => array:2 [ "nombre" => "María Carmen" "apellidos" => "Valero Ubierna" ] 2 => array:2 [ "nombre" => "Norberto" "apellidos" => "Ortego Centeno" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0025775322000379" "doi" => "10.1016/j.medcli.2021.12.014" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775322000379?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020622003084?idApp=UINPBA00004N" "url" => "/23870206/0000015900000002/v1_202207200641/S2387020622003084/v1_202207200641/en/main.assets" ] "itemAnterior" => array:19 [ "pii" => "S2387020622003114" "issn" => "23870206" "doi" => "10.1016/j.medcle.2022.07.003" "estado" => "S300" "fechaPublicacion" => "2022-07-22" "aid" => "5942" "copyright" => "Elsevier España, S.L.U." "documento" => "article" "crossmark" => 1 "subdocumento" => "rev" "cita" => "Med Clin. 2022;159:92-100" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:13 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Review</span>" "titulo" => "Barrett’s esophagus, towards improved clinical practice" "tienePdf" => "en" "tieneTextoCompleto" => "en" "tieneResumen" => array:2 [ 0 => "en" 1 => "es" ] "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "92" "paginaFinal" => "100" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Esófago de Barrett, hacia la mejora de la práctica clínica" ] ] "contieneResumen" => array:2 [ "en" => true "es" => true ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:8 [ "identificador" => "fig0010" "etiqueta" => "Fig. 2" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr2.jpeg" "Alto" => 1637 "Ancho" => 2508 "Tamanyo" => 315569 ] ] "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at0010" "detalle" => "Fig. " "rol" => "short" ] ] "descripcion" => array:1 [ "en" => "<p id="spar0020" class="elsevierStyleSimplePara elsevierViewall">Prague classification. The diaphragmatic hiatus can be seen distally, the contraction of which oscillates with respiratory movements. The esophagogastric junction coincides with the proximal margin of the gastric folds. Displacement of the esophagogastric junction proximal to the diaphragmatic hiatus represents a sliding hiatal hernia. The extent of Barrett’s oesophagus is defined by the Prague classification: maximum longitudinal extent in cm (M: distance between the esophagogastric junction and the most proximal extent of the squamocolumnar junction) and maximum circumferential extent in cm (C: distance between the junction esophagogastric and the most proximal circumferential extent of the squamocolumnar junction). Adapted from Peters et al.<a class="elsevierStyleCrossRef" href="#bib0055"><span class="elsevierStyleSup">11</span></a>.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Samuel Jesús Martínez-Domínguez, Ángel Lanas, María José Domper-Arnal" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Samuel Jesús" "apellidos" => "Martínez-Domínguez" ] 1 => array:2 [ "nombre" => "Ángel" "apellidos" => "Lanas" ] 2 => array:2 [ "nombre" => "María José" "apellidos" => "Domper-Arnal" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0025775322001397" "doi" => "10.1016/j.medcli.2022.02.012" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775322001397?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020622003114?idApp=UINPBA00004N" "url" => "/23870206/0000015900000002/v1_202207200641/S2387020622003114/v1_202207200641/en/main.assets" ] "en" => array:17 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Special article</span>" "titulo" => "Hypertension in non-pregnant women of childbearing age" "tieneTextoCompleto" => true "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "101" "paginaFinal" => "105" ] ] "autores" => array:1 [ 0 => array:4 [ "autoresLista" => "Albertina M. Ghelfi, Gustavo J. Staffieri" "autores" => array:2 [ 0 => array:4 [ "nombre" => "Albertina M." "apellidos" => "Ghelfi" "email" => array:1 [ 0 => "albertinaghelfi@hotmail.com" ] "referencia" => array:3 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">a</span>" "identificador" => "aff0005" ] 1 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">b</span>" "identificador" => "aff0010" ] 2 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">*</span>" "identificador" => "cor0005" ] ] ] 1 => array:3 [ "nombre" => "Gustavo J." "apellidos" => "Staffieri" "referencia" => array:2 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">b</span>" "identificador" => "aff0010" ] 1 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">c</span>" "identificador" => "aff0015" ] ] ] ] "afiliaciones" => array:3 [ 0 => array:3 [ "entidad" => "Unidad de Hipertensión Arterial y Riesgo Cardiovascular, Servicio de Clínica Médica, Hospital Escuela Eva Perón, Granadero Baigorria, Argentina" "etiqueta" => "a" "identificador" => "aff0005" ] 1 => array:3 [ "entidad" => "Asociación de Hipertensión Arterial de Rosario, Rosario, Argentina" "etiqueta" => "b" "identificador" => "aff0010" ] 2 => array:3 [ "entidad" => "Unidad de Hipertensión Arterial, Grupo Oroño, Rosario, Argentina" "etiqueta" => "c" "identificador" => "aff0015" ] ] "correspondencia" => array:1 [ 0 => array:3 [ "identificador" => "cor0005" "etiqueta" => "⁎" "correspondencia" => "Corresponding author." ] ] ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Hipertensión arterial en la mujer en edad fértil no gestante" ] ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:8 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1627 "Ancho" => 2925 "Tamanyo" => 295622 ] ] "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at0005" "detalle" => "Fig. " "rol" => "short" ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Guidance algorithm for defining the antihypertensive treatment regimen in women of childbearing age. CVD: cardiovascular disease; HTN: arterial hypertension; TOD: target organ injury; MoC: method of contraception.</p>" ] ] ] "textoCompleto" => "<span class="elsevierStyleSections"><span id="sec0005" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0005">Introduction</span><p id="par0005" class="elsevierStylePara elsevierViewall">Cardiovascular diseases (CVD) are the leading cause of death in women in the Western world. Although hypertension (HTN) is less common and usually better controlled in women, the presence of this factor can match the cardiovascular risk (CVR) of men and even triple the chance of an ischaemic event.<a class="elsevierStyleCrossRefs" href="#bib0005"><span class="elsevierStyleSup">1,2</span></a> In Spain, more than 50% of deaths in women are due to diseases of the circulatory system<a class="elsevierStyleCrossRef" href="#bib0015"><span class="elsevierStyleSup">3</span></a>; in the USA, CVD in women is responsible for more deaths than all cancers affecting women combined,<a class="elsevierStyleCrossRef" href="#bib0020"><span class="elsevierStyleSup">4</span></a> while in Argentina one in three women dies of CVD.<a class="elsevierStyleCrossRef" href="#bib0025"><span class="elsevierStyleSup">5</span></a> The perception of the real dimensions of this problem remains low, not only among the population, but also among health teams.<a class="elsevierStyleCrossRefs" href="#bib0015"><span class="elsevierStyleSup">3–7</span></a> Women themselves, especially younger women, perceive gynaecological cancer as the main cause of death associated with their gender, while they point to CVD as a problem more often linked to men. Surveys report that only 20–40% of patients ever discuss their risk of heart disease with their doctor.<a class="elsevierStyleCrossRefs" href="#bib0015"><span class="elsevierStyleSup">3–6</span></a> The likelihood of CVD in women is often underestimated among health professionals. Given the same clinical scenarios, women tend to be assigned a lower CVR category and receive fewer preventive recommendations. When faced with an ischemic event, a woman is more likely to be misdiagnosed, receive fewer medications, have less aggressive treatments, and be discharged sooner than a man.<a class="elsevierStyleCrossRefs" href="#bib0030"><span class="elsevierStyleSup">6,8</span></a></p><p id="par0010" class="elsevierStylePara elsevierViewall">This bias is probably related to the protective role conferred by oestrogens during the fertile years of these patients.<a class="elsevierStyleCrossRefs" href="#bib0015"><span class="elsevierStyleSup">3,5</span></a> However, this hormonal protection cannot be extrapolated to other stages and is far from infallible, especially in adverse metabolic circumstances. Among young women, a decreased promotion of healthy habits and an increased prevalence of diabetes mellitus (DM), obesity (OB), dyslipidaemia (DLP) and smoking status (SS) at younger ages have been observed.<a class="elsevierStyleCrossRefs" href="#bib0020"><span class="elsevierStyleSup">4,5,9</span></a> This would lead to persistently poorer cardiovascular profiles later in life, which, together with the disappearance of oestrogen protection at menopause, would facilitate the development of CVD.<a class="elsevierStyleCrossRefs" href="#bib0015"><span class="elsevierStyleSup">3,5,6</span></a></p><p id="par0015" class="elsevierStylePara elsevierViewall">In this scenario, HTN is frequently involved, occurring in more than 25% of women worldwide and representing the most important CVR factor in this group.<a class="elsevierStyleCrossRef" href="#bib0050"><span class="elsevierStyleSup">10</span></a> In addition to essential HTN, women have gender-specific hypertensive scenarios, such as those associated with oral contraceptive use, assisted reproduction, menopause, hormone replacement therapy, and pregnancy and/or postpartum.<a class="elsevierStyleCrossRefs" href="#bib0050"><span class="elsevierStyleSup">10,11</span></a></p><p id="par0020" class="elsevierStylePara elsevierViewall">We consider it necessary to reflect on the real implications of HTN and its impact on CVR in this population, paying attention to specific scenarios, where even in the middle of the reproductive stage women leave unquestionable cardiovascular signs.</p><p id="par0025" class="elsevierStylePara elsevierViewall">The range of situations in this regard is wide. A significant event could be the development of pre-eclampsia (PE), in which autoimmune abnormalities will be triggered leading to inflammation and damage to the vascular endothelium. Endothelial dysfunction will persist over time even after pregnancy has ended, conferring an increased risk of developing CVD later in life.<a class="elsevierStyleCrossRefs" href="#bib0060"><span class="elsevierStyleSup">12–14</span></a></p><p id="par0030" class="elsevierStylePara elsevierViewall">Similarly, we found scenarios where young adults present with early or subclinical target organ damage (TOD)-associated HTN. Rheumatic and autoimmune diseases have a low prevalence but affect women more often in all age and ethnic groups, with manifestations often beginning in youth and frequently including renal involvement. These entities have as a common denominator an underlying chronic inflammatory state, with rapid development of stiffness and subclinical atherosclerosis with an increased likelihood of plaque rupture and are associated in a multifactorial manner with other clinical conditions such as HTN.<a class="elsevierStyleCrossRef" href="#bib0075"><span class="elsevierStyleSup">15</span></a></p><p id="par0035" class="elsevierStylePara elsevierViewall">Also, to be considered are entities of increasing prevalence where the risk of premature vascular ageing with the possibility of renal involvement at an early age is very likely, especially considering that its presence is no longer uncommon in adolescents and young adults. Age-stratified analyses estimate that a diagnosis of DM at around 15 years of age results in an average loss of 12 years of life.<a class="elsevierStyleCrossRefs" href="#bib0015"><span class="elsevierStyleSup">3,16</span></a> In this regard it is worth recalling the existing and aforementioned disparities in the drug therapy offered, as a woman with DM is also less likely to receive aspirin, statins or certain antihypertensive drugs compared to a male patient with a similar medical history.<a class="elsevierStyleCrossRefs" href="#bib0015"><span class="elsevierStyleSup">3,9,17</span></a></p><p id="par0040" class="elsevierStylePara elsevierViewall">Effective blood pressure (BP) controls improve overall long-term cardiovascular outcomes in all cases.<a class="elsevierStyleCrossRefs" href="#bib0050"><span class="elsevierStyleSup">10,11</span></a> While it would appear that there are no antihypertensive regimens that are more effective in women than in men,<a class="elsevierStyleCrossRefs" href="#bib0040"><span class="elsevierStyleSup">8,10</span></a> there are some facts that are particular to the female population and should be taken into account when prescribing. Two in particular stand out: a higher frequency of adverse effects when taking antihypertensives (oedema with the use of calcium channel blockers, cough with angiotensin-converting enzyme inhibitors, and hyponatremia and hypokalaemia with diuretics) and the possibility of pregnancy during the reproductive age. In this regard, it is often observed that a significant number of professionals will directly avoid the use of RAAS inhibitors in childbearing age in view of their potential toxic-teratogenic effect in case of pregnancy.<a class="elsevierStyleCrossRefs" href="#bib0010"><span class="elsevierStyleSup">2,10,11,18–20</span></a></p><p id="par0045" class="elsevierStylePara elsevierViewall">That said, it is clear that preferences for use of one or the other antihypertensive, regardless of therapeutic effectiveness, will vary greatly depending on whether the treatment is for a man or a woman. It is worth considering whether this predilection for use – or disuse – of RAAS inhibitors is equally applicable to all conditions of HTN in women of childbearing age, especially when intervention could prevent, halt or even reverse the damage.</p><p id="par0050" class="elsevierStylePara elsevierViewall">In the light of the above, the following questions arise: Can we continue to generalise under the label “women of childbearing age” patients who do not share the same baseline scenarios? If we recognise these differences, why do antihypertensive treatment recommendations tend to be standardised for young adult women? In view of the increased prevalence of conditions associated with TOD, can we generalise a relative contraindication to RAAS inhibitors or a delayed introduction of drugs that would delay the progression of these lesions considering a probable pregnancy? If pregnancy is a concern, is it not more appropriate to strengthen the method of contraception (MoC) than to avoid drugs with proven benefits?</p><p id="par0055" class="elsevierStylePara elsevierViewall">The intention of this article is to review the safety of our certainties and to discuss with a critical eye the controversies that influence therapeutic behaviour in these women.</p></span><span id="sec0010" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0010">Hypertension in non-pregnant women of childbearing<span class="elsevierStyleHsp" style=""></span><span class="elsevierStyleHsp" style=""></span>age</span><p id="par0060" class="elsevierStylePara elsevierViewall">Before we dive into the potential implications of each drug regimen, we should point out what does not yet seem to be so obvious: <span class="elsevierStyleItalic">not all women wish to become mothers</span>. It is not the intention of this article to reflect on the necessary change of paradigm that has emerged in our society in relation to the vindication of the role of women, nor do we feel able to analyse the social movements that accompany their social-cultural hierarchisation. But we must point out that <span class="elsevierStyleItalic">reproductive capacity</span> and <span class="elsevierStyleItalic">desire to conceive</span> are not the same thing.</p><p id="par0065" class="elsevierStylePara elsevierViewall">Many clinical practice guidelines recommend avoiding the use of RAAS inhibitors in this period of life if not necessary.<a class="elsevierStyleCrossRefs" href="#bib0090"><span class="elsevierStyleSup">18–20</span></a> But in daily practice, and especially in our country, it is generally observed that most professionals always avoid them, as if they were banned for these women.</p><p id="par0070" class="elsevierStylePara elsevierViewall">We owe it to ourselves to reflect deeply on the counterpoints of this position. We should discuss whether it is not reductionist to believe that avoiding prescription solves the problem, instead of discussing how to proceed in the face of the growing need for the use of these drugs in this period, how to improve counselling on the subject, how to strengthen educational spaces on sexual health, and how to make a better selection of the MoC that adapts to the desires and cultural, educational, economic, social, psychological and biological possibilities of each woman.</p><p id="par0075" class="elsevierStylePara elsevierViewall">There are multiple situations where the introduction of an angiotensin-converting enzyme inhibitor (ACEI) or an angiotensin II receptor blocker (ARB) represents a significant additional benefit for these women. Among these stand out:<ul class="elsevierStyleList" id="lis0005"><li class="elsevierStyleListItem" id="lsti0005"><span class="elsevierStyleLabel">1)</span><p id="par0080" class="elsevierStylePara elsevierViewall">The ability to regress left ventricular hypertrophy and nephroprotective behaviour by reducing protein excretion. This, together with the fact that they do not alter the lipid profile and improve insulin resistance, makes them first-line treatment for HTN associated with DM.<a class="elsevierStyleCrossRefs" href="#bib0095"><span class="elsevierStyleSup">19,20</span></a></p></li><li class="elsevierStyleListItem" id="lsti0010"><span class="elsevierStyleLabel">2)</span><p id="par0085" class="elsevierStylePara elsevierViewall">An important role in the treatment of autoimmune diseases, especially in rheumatoid arthritis due to its potential anti-inflammatory effect and in systemic lupus erythematosus due to its antiproteinuric effects.<a class="elsevierStyleCrossRef" href="#bib0075"><span class="elsevierStyleSup">15</span></a></p></li><li class="elsevierStyleListItem" id="lsti0015"><span class="elsevierStyleLabel">3)</span><p id="par0090" class="elsevierStylePara elsevierViewall">A very useful option in patients infected with human immunodeficiency virus because of its beneficial metabolic effects and reduced likelihood of dangerous interactions with antiretroviral therapy.<a class="elsevierStyleCrossRef" href="#bib0075"><span class="elsevierStyleSup">15</span></a></p></li><li class="elsevierStyleListItem" id="lsti0020"><span class="elsevierStyleLabel">4)</span><p id="par0095" class="elsevierStylePara elsevierViewall">In any other setting with chronic low-grade inflammation and/or accelerated vascular ageing, ACE inhibitors influence arterial stiffness by reducing vasoconstriction and improving endothelial function, which can be assessed by observing improvements in parameters such as pulse wave velocity (PWV).<a class="elsevierStyleCrossRef" href="#bib0105"><span class="elsevierStyleSup">21</span></a></p></li></ul></p><p id="par0100" class="elsevierStylePara elsevierViewall">Are these scenarios really so rare in everyday clinical practice? How certain can we be that in these women we should avoid ACEIs or ARBs, just to protect against a potential pregnancy? Does a pregnancy that has not yet occurred really weigh more in the equation than the actual documented organ damage? We believe it is important to stress the need to explore the woman’s desire for pregnancy and to properly plan antihypertensive treatment at this stage based on her wishes.</p><p id="par0105" class="elsevierStylePara elsevierViewall">We have stated that the therapeutic efficacy of antihypertensive drugs is similar in females and males, so the choice of therapy is weighed against these other factors to be considered.<a class="elsevierStyleCrossRefs" href="#bib0010"><span class="elsevierStyleSup">2,8,10</span></a> So let’s talk about the management of hypertension in young individuals. The approximate prevalence of hypertension in individuals aged 16–35 is 12%. In these groups, confirmation of the diagnosis by ambulatory BP monitoring is necessary as white coat hypertension, an entity more often seen in women than in men, is common. When the diagnosis is confirmed, although most cases are usually due to essential hypertension, there is a need to rule out causes of secondary hypertension, since the entities that determine it are more common in youth.<a class="elsevierStyleCrossRefs" href="#bib0010"><span class="elsevierStyleSup">2,20</span></a> These entities are more common in women and are usually underdiagnosed in this group.<a class="elsevierStyleCrossRefs" href="#bib0010"><span class="elsevierStyleSup">2,10</span></a> An age-based approach is recommended, considering especially in the female population: renal parenchymal diseases, renovascular hypertension due to fibromuscular dysplasia, hyperaldosteronism, hypothyroidism, hypertension induced by hormonal contraceptives, street drugs and herbal health products.<a class="elsevierStyleCrossRefs" href="#bib0010"><span class="elsevierStyleSup">2,10,20</span></a> Likewise, the metabolic profile and the eventual presence of associated TOD must be assessed, remembering that OB can be a determinant of hypertension even in childhood, and predisposes to states of insulin resistance and earlier DM onset.<a class="elsevierStyleCrossRefs" href="#bib0005"><span class="elsevierStyleSup">1,2,10,16</span></a><span class="elsevierStyleSup">,</span><a class="elsevierStyleCrossRef" href="#bib0100"><span class="elsevierStyleSup">20</span></a> The Argentine Consensus on HTN indicates starting drugs when diastolic BP is ≥ 90 mmHg, or, in those cases where the systolic BP is ≥ 140 mmHg with parallel TOD evidence.<a class="elsevierStyleCrossRef" href="#bib0100"><span class="elsevierStyleSup">20</span></a> The general recommendation for this group is to use the doses and antihypertensive drugs commonly prescribed to adults, i.e., according to the latest published guidelines, treatment should preferably be based on combinations of ACEIs or ARBs with calcium channel blockers or thiazide/thiazide-like, as these drugs are complementary in their mechanism of action, limiting the potentially associated adverse reactions.<a class="elsevierStyleCrossRefs" href="#bib0050"><span class="elsevierStyleSup">10,19,20</span></a> However, this and other texts will indicate that ACEIs and ARBs are relatively contraindicated in young women of childbearing age,<a class="elsevierStyleCrossRefs" href="#bib0050"><span class="elsevierStyleSup">10,19,20</span></a> although some will mention that this preference for avoidance will only apply to settings where there is no safe MoC.<a class="elsevierStyleCrossRef" href="#bib0095"><span class="elsevierStyleSup">19</span></a> The possibility of using a beta-blocker (BB) at this stage is considered by both the European Society of Cardiology (ESC) and the Argentine Consensus, especially in young subjects between 16 and 35 years of age with hyperdynamic hypertension<a class="elsevierStyleCrossRef" href="#bib0100"><span class="elsevierStyleSup">20</span></a> and/or in the event that a young woman plans a pregnancy.<a class="elsevierStyleCrossRef" href="#bib0095"><span class="elsevierStyleSup">19</span></a></p><p id="par0110" class="elsevierStylePara elsevierViewall">Here one might wonder why the risk posed by ACEIs and ARBs in the face of a potential pregnancy is a sufficient argument to avoid them in the childbearing age, but this same premise does not exert similar pressure for BBs. For the time being, the only BB with a good safety profile during pregnancy is labetalol, and the use of other drugs in the same family for the management of HTN in pregnant women is discouraged.<a class="elsevierStyleCrossRef" href="#bib0110"><span class="elsevierStyleSup">22</span></a></p><p id="par0115" class="elsevierStylePara elsevierViewall">In recent years, there is growing evidence that all agents in this pharmacological group should be avoided in the first trimester of pregnancy.<a class="elsevierStyleCrossRefs" href="#bib0110"><span class="elsevierStyleSup">22,23</span></a> The contraindication of administering atenolol during the 3 trimesters is strong in view of the fact that it is a drug with proven harmful effects on the foetus, placed in risk category D in the <span class="elsevierStyleItalic">Food and Drug Administration’s classification</span>.<a class="elsevierStyleCrossRefs" href="#bib0110"><span class="elsevierStyleSup">22,23</span></a> We believe that if a BB is used at this stage and if there is a possibility of pregnancy, labetalol should be preferred, although it should be remembered that in case of pregnancy any BB should ideally be started after the 20th week of pregnancy because of its effects on the foetus.<a class="elsevierStyleCrossRefs" href="#bib0010"><span class="elsevierStyleSup">2,24</span></a> As can be seen, the choice of this group of antihypertensives during childbearing years is not entirely safe either.</p><p id="par0120" class="elsevierStylePara elsevierViewall">Calcium channel blockers are designated as second- or third-line drugs by the ESC.<a class="elsevierStyleCrossRef" href="#bib0095"><span class="elsevierStyleSup">19</span></a> These drugs have proven useful in BP reduction and have demonstrated reductions in ventricular mass in hypertrophy, antiatherogenic, antiproliferative and natriuretic effects by increasing renal plasma flow through afferent vasodilation. Their indication in women often meets with some reservations, in view of an increased reported occurrence of oedema with the use of these drugs, although this adverse reaction is not consistent.<a class="elsevierStyleCrossRefs" href="#bib0010"><span class="elsevierStyleSup">2,10</span></a> If the practitioner is concerned about the possibility of an unwanted pregnancy, dihydropyridine calcium channel blockers are an option. Both nifedipine and amlodipine appear to be safe in pregnancy, although these drugs are also preferred after 20 weeks’ gestational age and require special considerations regarding antihypertensive potency, available formulations and evidence with the use of the different presentations.<a class="elsevierStyleCrossRefs" href="#bib0010"><span class="elsevierStyleSup">2,24</span></a></p><p id="par0125" class="elsevierStylePara elsevierViewall">The use of diuretics is also currently considered as second or third line by ESC.<a class="elsevierStyleCrossRef" href="#bib0095"><span class="elsevierStyleSup">19</span></a> Thiazide diuretics such as hydrochlorothiazide (HCTZ) used to be commonly prescribed for young women. This trend has diminished in recent years, mainly in view of their questionable usefulness as first-line antihypertensives and their proven advantages when used in combinations. They are relatively contraindicated in pregnancy, as there are proven detrimental metabolic effects on the foetus, especially during the first trimester, as well as the possibility of triggering complications such as the development of PE.<a class="elsevierStyleCrossRefs" href="#bib0095"><span class="elsevierStyleSup">19,22,25</span></a> HCTZ is considered useful for preventing osteoporosis and reducing CVR in elderly patients, which implies a benefit for administration in menopausal women, but these data do not justify its choice during childbearing age.<a class="elsevierStyleCrossRef" href="#bib0010"><span class="elsevierStyleSup">2</span></a></p><p id="par0130" class="elsevierStylePara elsevierViewall">Regarding ACEIs and ARBs, their category tends to be generalized. They are toxic during the first trimester of pregnancy and teratogenic during the second and third. In large-scale studies by Walfisch et al.<a class="elsevierStyleCrossRef" href="#bib0130"><span class="elsevierStyleSup">26</span></a> and Li et al.,<a class="elsevierStyleCrossRef" href="#bib0135"><span class="elsevierStyleSup">27</span></a> no evidence was found to show that first-trimester ACEI exposure was associated with an increased risk of major malformations compared with other antihypertensives. Both conclude that this risk could be related to the use of either of these drugs or to the underlying hypertensive condition even if the woman is not on medication.<a class="elsevierStyleCrossRefs" href="#bib0120"><span class="elsevierStyleSup">24,26,27</span></a><span class="elsevierStyleItalic">The National Institute for Health and Care Excellence 2019 guidelines</span> consider the possibility of preconception prescription of ACEIs or ARBs in women with associated conditions, advising in these cases to alert patients to the need for early notification of their pregnancy for immediate discontinuation of these pharmacological agents.<a class="elsevierStyleCrossRef" href="#bib0125"><span class="elsevierStyleSup">25</span></a> If an early withdrawal, meaning before the end of the first trimester, is carried out, it is very likely that there will be no major consequences.</p><p id="par0135" class="elsevierStylePara elsevierViewall">It is not our intention to state that these antihypertensives should be used liberally and indiscriminately, nor that they should be maintained throughout the first trimester of pregnancy. We believe that women should receive medication based on the general guidelines issued for the adult population, taking into account the particularities of each case and the existence of associated TOD. Any drugs with teratogenic potential, especially ACEIs and ARBs, but also those that cause foetal toxicity, such as BB and HCTZ, should be avoided in young women of childbearing age if they do not provide a real benefit over other drugs with similar BP-lowering utility. However, in cases where the introduction of these drugs would be of clear benefit to the patient, they should be indicated, taking contraceptive precautions.<a class="elsevierStyleCrossRef" href="#bib0120"><span class="elsevierStyleSup">24</span></a></p><p id="par0140" class="elsevierStylePara elsevierViewall">In the latter situation we must remember the need to discuss the risks, benefits and therapeutic alternatives with the patient. If the woman wishes to become a mother now and is planning a pregnancy: she should be referred to an obstetric consultation in order to draw up an interdisciplinary plan of action. We should discuss the need to use drugs that do not pose a risk, highlighting that during this stage these therapies will not slow down or improve the lesions associated with her hypertension, and that once the pregnancy is over, she should be re-evaluated for any progression of these lesions. If the woman wishes to face this risk in favour of her desire for motherhood, she should be reassured that the drugs selected are those with the best available evidence in terms of safety, and that if there are no other complications, this therapeutic change will allow her to carry her pregnancy to term. It must be taken into account that this action plan must also include the postpartum period and that the pharmacological behaviours of this stage must also be agreed with the patient.</p><p id="par0145" class="elsevierStylePara elsevierViewall">If the woman has no current desire for conception, or motherhood is not in her life plans: she should be referred for gynaecological counselling so that she receives a safe MoC, which does not increase her CVR in the face of her underlying process. There are eligibility criteria for the use of safe, effective and acceptable contraceptives for women with cardiovascular conditions, which are especially worth considering when faced with the combination of different comorbidities or associated pathologies. Beyond the introduction of the MoC, we should warn about the possibilities of failure associated with each method, as well as advise that in the event of pregnancy, prompt medical advice should be sought. <a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a> proposes an algorithm for action on the basis of what has been reviewed in these paragraphs.</p><elsevierMultimedia ident="fig0005"></elsevierMultimedia></span><span id="sec0015" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0015">Hypertension in childbearing age after pregnancy</span><p id="par0150" class="elsevierStylePara elsevierViewall">Although this article does not intend to review in detail the pharmacological indications for hypertensive disorders in pregnancy (HDP), we do consider it important to prioritise the recommendations for the adequacy of the antihypertensive regimen in the postpartum period, opting for drugs that address vascular damage.</p><p id="par0155" class="elsevierStylePara elsevierViewall">Management should be aimed at addressing the vascular damage observed. It may be related to acute pregnancy-related TOD in the context of PE: development of peripartum dilated cardiomyopathy, development of heart failure or presence of nephrotic syndrome, among others; or it may correspond to subclinical or clinical TOD known prior to pregnancy: microalbuminuria, vascular stiffness, ventricular hypertrophy, atheromatosis, autoimmune diseases or DM, among others.</p><p id="par0160" class="elsevierStylePara elsevierViewall">In these scenarios, the prescription of an ACEI can have numerous benefits: from decreased afterload to improved proteinuria. Although enalapril and captopril have shown safety for use during breastfeeding, the former is preferred in view of its negligible excretion in breast milk.<a class="elsevierStyleCrossRefs" href="#bib0125"><span class="elsevierStyleSup">25,28</span></a> Although ARBs could exhibit the same potential benefits as an ACEI in terms of TOD management, due to the lack of data in the lactation period, they are classified as a yellow category. That said, given the need for use and if the woman is breastfeeding, the introduction of an ACEI<a class="elsevierStyleCrossRef" href="#bib0120"><span class="elsevierStyleSup">24</span></a> is preferable.</p><p id="par0165" class="elsevierStylePara elsevierViewall">In postpartum women with chronic HTN without evidence of TOD and in gestational HTN, other safe drugs can be used at this stage – such as nifedipine, amlodipine or labetalol – based on individual patient characteristics.</p><p id="par0170" class="elsevierStylePara elsevierViewall">It is highly recommended that all professionals involved in the care of postpartum women, especially those who have experienced HDP, be aware of the risk of the “fourth trimester”. This stage refers to the remainder of a woman’s life after childbirth, a period of great vulnerability for the development of short- and long-term cardiovascular and metabolic complications.<a class="elsevierStyleCrossRef" href="#bib0145"><span class="elsevierStyleSup">29</span></a></p><p id="par0175" class="elsevierStylePara elsevierViewall">Having HDP, and especially PE, increases the risk of developing CVD in later life. Due to the long-term persistence of established endothelial dysfunction, a woman’s risk of CVD death may be almost equal to that of a man. According to the <span class="elsevierStyleItalic">American Heart Association</span> 2021 guidelines, a history of pregnancy complications, such as HDP, gestational diabetes or abruptio placentae, should be taken as an indicator of a strong need for primary CVD prevention, as they have been linked to an increased risk of coronary heart disease, heart failure, cerebrovascular disease and peripheral vascular disease.<a class="elsevierStyleCrossRef" href="#bib0150"><span class="elsevierStyleSup">30</span></a></p></span><span id="sec0020" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0020">Conclusions</span><p id="par0180" class="elsevierStylePara elsevierViewall">We believe it is necessary to break with old axioms and reconsider these ideas in the light of current evidence: CVD is the leading cause of death in women in the Western world; most women will have HTN as a major associated risk factor; the unfavourable cardiometabolic profiles of youth are carried over into later life with a significant impact when oestrogen deprivation occurs; women who develop HDP will have a higher CVR throughout their lives; in many settings these issues are poorly recognised by health care teams. In all cases, it is highly recommended to discuss with the woman the benefits and risks of the available treatments, and the implications of introducing or withdrawing them, aiming at a critical and unbiased professional exercise that assists in making personalised decisions in the context of the particular scenario.</p></span><span id="sec0025" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0025">Funding</span><p id="par0185" class="elsevierStylePara elsevierViewall">This paper has not received any type of funding.</p></span><span id="sec0030" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0030">Conflict of interests</span><p id="par0190" class="elsevierStylePara elsevierViewall">The authors declare no conflicts of interest.</p></span></span>" "textoCompletoSecciones" => array:1 [ "secciones" => array:7 [ 0 => array:2 [ "identificador" => "sec0005" "titulo" => "Introduction" ] 1 => array:2 [ "identificador" => "sec0010" "titulo" => "Hypertension in non-pregnant women of childbearing age" ] 2 => array:2 [ "identificador" => "sec0015" "titulo" => "Hypertension in childbearing age after pregnancy" ] 3 => array:2 [ "identificador" => "sec0020" "titulo" => "Conclusions" ] 4 => array:2 [ "identificador" => "sec0025" "titulo" => "Funding" ] 5 => array:2 [ "identificador" => "sec0030" "titulo" => "Conflict of interests" ] 6 => array:1 [ "titulo" => "References" ] ] ] "pdfFichero" => "main.pdf" "tienePdf" => true "fechaRecibido" => "2021-12-10" "fechaAceptado" => "2022-02-01" "NotaPie" => array:1 [ 0 => array:2 [ "etiqueta" => "☆" "nota" => "<p class="elsevierStyleNotepara" id="npar0005">Please cite this article as: Ghelfi AM, Staffieri GJ. Hipertensión arterial en la mujer en edad fértil no gestante. Med Clin (Barc). 2022;159:101–105.</p>" ] ] "multimedia" => array:1 [ 0 => array:8 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1627 "Ancho" => 2925 "Tamanyo" => 295622 ] ] "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at0005" "detalle" => "Fig. " "rol" => "short" ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Guidance algorithm for defining the antihypertensive treatment regimen in women of childbearing age. CVD: cardiovascular disease; HTN: arterial hypertension; TOD: target organ injury; MoC: method of contraception.</p>" ] ] ] "bibliografia" => array:2 [ "titulo" => "References" "seccion" => array:1 [ 0 => array:2 [ "identificador" => "bibs0005" "bibliografiaReferencia" => array:30 [ 0 => array:3 [ "identificador" => "bib0005" "etiqueta" => "[1]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Características epidemiológicas de la hipertensión arterial en la Argentina. Estudio RENATA 2" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:6 [ 0 => "A.M. Delucchi" 1 => "C.R. Majul" 2 => "A. Vicario" 3 => "G.H. Cerezo" 4 => "G. Fábregues" 5 => "Registro Nacional de Hipertensión Arterial" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "Rev Argent Cardiol" "fecha" => "2017" "volumen" => "85" "paginaInicial" => "354" "paginaFinal" => "360" "itemHostRev" => array:3 [ "pii" => "S0168827814008563" "estado" => "S300" "issn" => "01688278" ] ] ] ] ] ] ] 1 => array:3 [ "identificador" => "bib0010" "etiqueta" => "[2]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Toma de posición. Hipertensión en la Mujer" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:1 [ 0 => "Sociedad Argentina de Hipertensión Arterial" ] ] ] ] ] "host" => array:2 [ 0 => array:1 [ "Libro" => array:1 [ "fecha" => "2018" ] ] 1 => array:1 [ "WWW" => array:1 [ "link" => "http://www.saha.org.ar/files/documents/HTA-en-la-mujer.pdf" ] ] ] ] ] ] 2 => array:3 [ "identificador" => "bib0015" "etiqueta" => "[3]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "La enfermedad cardiovascular en función del género: mitos y evidencias" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:1 [ 0 => "A. Coca" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.rce.2011.10.011" "Revista" => array:7 [ "tituloSerie" => "Rev Clín Esp" "fecha" => "2012" "volumen" => "212" "paginaInicial" => "81" "paginaFinal" => "83" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/22153585" "web" => "Medline" ] ] "itemHostRev" => array:3 [ "pii" => "S0168827814004085" "estado" => "S300" "issn" => "01688278" ] ] ] ] ] ] ] 3 => array:3 [ "identificador" => "bib0020" "etiqueta" => "[4]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Knowledge, attitudes, and beliefs regarding cardiovascular disease in women. The Women’s Heart Alliance" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "C.N.B. Merz" 1 => "H. Andersen" 2 => "E. Sprague" 3 => "A. Burns" 4 => "M. Keida" 5 => "M.N. Walsh" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.jacc.2017.05.024" "Revista" => array:6 [ "tituloSerie" => "J Am Coll Cardiol" "fecha" => "2017" "volumen" => "70" "paginaInicial" => "123" "paginaFinal" => "132" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/28648386" "web" => "Medline" ] ] ] ] ] ] ] ] 4 => array:3 [ "identificador" => "bib0025" "etiqueta" => "[5]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Causas de muerte en la mujer y su tendencia en los últimos 23 años en la Argentina" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "M.I. Sosa Liprandi" 1 => "P.S. Harwicz" 2 => "A. Sosa Liprandi" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "Rev Argent Cardiol" "fecha" => "2006" "volumen" => "74" "paginaInicial" => "297" "paginaFinal" => "303" "itemHostRev" => array:3 [ "pii" => "S0016508518300167" "estado" => "S300" "issn" => "00165085" ] ] ] ] ] ] ] 5 => array:3 [ "identificador" => "bib0030" "etiqueta" => "[6]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Enfermedad cardiovascular en la mujer. Cómo la perciben, qué conocen y qué conductas de prevención adoptan las mujeres" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "C. Artucio" 1 => "M. Giambruno" 2 => "I. Duro" 3 => "V. Michelis" 4 => "D. Korytnicki" 5 => "D. Barranco" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Rev Urug de Cardiol" "fecha" => "2017" "volumen" => "32" "paginaInicial" => "13" "paginaFinal" => "22" ] ] ] ] ] ] 6 => array:3 [ "identificador" => "bib0035" "etiqueta" => "[7]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Symptom recognition and healthcare experiences of young women with acute myocardial infarction" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "J.H. Lichtman" 1 => "E.C. Leifheit-Limson" 2 => "E. Watanabe" 3 => "N.B. Allen" 4 => "B. Garavalia" 5 => "L.S. Garavalia" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1161/CIRCOUTCOMES.114.001612" "Revista" => array:7 [ "tituloSerie" => "Circ Cardiovasc Qual Outcomes" "fecha" => "2015" "volumen" => "8" "paginaInicial" => "S31" "paginaFinal" => "S38" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/25714826" "web" => "Medline" ] ] "itemHostRev" => array:3 [ "pii" => "S0168827810008251" "estado" => "S300" "issn" => "01688278" ] ] ] ] ] ] ] 7 => array:3 [ "identificador" => "bib0040" "etiqueta" => "[8]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Do men and women respond differently to blood pressure-lowering treatment? Results of prospectively designed overviews of randomized trials" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "F. Turnbull" 1 => "M. Woodward" 2 => "B. Neal" 3 => "F. Barzi" 4 => "T. Ninomiya" 5 => "J. Chalmers" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1093/eurheartj/ehn427" "Revista" => array:6 [ "tituloSerie" => "Eur Heart J" "fecha" => "2008" "volumen" => "29" "paginaInicial" => "2669" "paginaFinal" => "2680" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/18852183" "web" => "Medline" ] ] ] ] ] ] ] ] 8 => array:3 [ "identificador" => "bib0045" "etiqueta" => "[9]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta-analysis of 37 prospective cohort studies" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "R. Huxley" 1 => "F. Barzi" 2 => "M. Woodward" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "BMJ" "fecha" => "2006" "volumen" => "14" "paginaInicial" => "73" "paginaFinal" => "78" ] ] ] ] ] ] 9 => array:3 [ "identificador" => "bib0050" "etiqueta" => "[10]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Hypertension across a woman’s life cycle" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:6 [ 0 => "N.K. Wenger" 1 => "A. Arnold" 2 => "C.N. Bairey Merz" 3 => "R.M. Cooper-DeHoff" 4 => "K.C. Ferdinand" 5 => "J.L. Fleg" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/0735-1097(94)90189-9" "Revista" => array:6 [ "tituloSerie" => "J Am Coll Cardiol" "fecha" => "2018" "volumen" => "24" "paginaInicial" => "1797" "paginaFinal" => "1813" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/7963130" "web" => "Medline" ] ] ] ] ] ] ] ] 10 => array:3 [ "identificador" => "bib0055" "etiqueta" => "[11]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Hipertensión arterial en la mujer" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:1 [ 0 => "J.K. Urrea" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "Rev Colomb Cardiol" "fecha" => "2018" "volumen" => "25" "numero" => "S1" "paginaInicial" => "13" "paginaFinal" => "20" ] ] ] ] ] ] 11 => array:3 [ "identificador" => "bib0060" "etiqueta" => "[12]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Long-term cardiovascular risks associated with adverse pregnancy outcomes" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:5 [ 0 => "A.D. Lane-Cordova" 1 => "S.S. Khan" 2 => "W.A. Grobman" 3 => "P. Greenland" 4 => "S.J. Shah" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.jacc.2018.12.092" "Revista" => array:6 [ "tituloSerie" => "J Am Coll Cardiol" "fecha" => "2019" "volumen" => "73" "paginaInicial" => "2106" "paginaFinal" => "2116" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/31023435" "web" => "Medline" ] ] ] ] ] ] ] ] 12 => array:3 [ "identificador" => "bib0065" "etiqueta" => "[13]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Cardiovascular risk, lipids and pregnancy: preeclampsia and the risk of later life cardiovascular disease" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "F. Charlton" 1 => "J. Tooher" 2 => "K.A. Rye" 3 => "A. Hennessy" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Hear Lung Circ" "fecha" => "2014" "volumen" => "23" "paginaInicial" => "203" "paginaFinal" => "212" ] ] ] ] ] ] 13 => array:3 [ "identificador" => "bib0070" "etiqueta" => "[14]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Post partum hypertension: “It Ain’t Over’ til It’s Over”" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "P. August" 1 => "L. Malha" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1161/CIRCULATIONAHA.115.019510" "Revista" => array:6 [ "tituloSerie" => "Circulation" "fecha" => "2015" "volumen" => "132" "paginaInicial" => "1690" "paginaFinal" => "1692" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/26416811" "web" => "Medline" ] ] ] ] ] ] ] ] 14 => array:3 [ "identificador" => "bib0075" "etiqueta" => "[15]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Riesgo Cardiovascular en las Enfermedades Inflamatorias Crónicas" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:1 [ 0 => "Sociedad Argentina de Cardiología" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "Rev Argent Cardiol" "fecha" => "2019" "volumen" => "87" "paginaInicial" => "1" "paginaFinal" => "45" "itemHostRev" => array:3 [ "pii" => "S0168827819301291" "estado" => "S300" "issn" => "01688278" ] ] ] ] ] ] ] 15 => array:3 [ "identificador" => "bib0080" "etiqueta" => "[16]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Age at diagnosis of type 2 diabetesmellitus and associations with cardiovascular and mortality risks" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:1 [ 0 => "Swedish National Diabetes Registry" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1161/CIRCULATIONAHA.118.037885" "Revista" => array:7 [ "tituloSerie" => "Circulation" "fecha" => "2019" "volumen" => "139" "paginaInicial" => "2228" "paginaFinal" => "2237" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/30955347" "web" => "Medline" ] ] "itemHostRev" => array:3 [ "pii" => "S0168827820303846" "estado" => "S300" "issn" => "01688278" ] ] ] ] ] ] ] 16 => array:3 [ "identificador" => "bib0085" "etiqueta" => "[17]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "S. Yusuf" 1 => "S. Hawken" 2 => "S. Ôunpuu" 3 => "T. Dans" 4 => "A. Avezum" 5 => "F. Lanas" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/S0140-6736(04)17018-9" "Revista" => array:7 [ "tituloSerie" => "Lancet" "fecha" => "2004" "volumen" => "364" "paginaInicial" => "937" "paginaFinal" => "952" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/15364185" "web" => "Medline" ] ] "itemHostRev" => array:3 [ "pii" => "S0168827818302149" "estado" => "S300" "issn" => "01688278" ] ] ] ] ] ] ] 17 => array:3 [ "identificador" => "bib0090" "etiqueta" => "[18]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Prescripción de enalapril a la mujer fértil como factor de riesgo de malformaciones congénitas en el primer nivel de atención pública de la Argentina" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "R.G. Bernztein" 1 => "I. Drake" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Rev Argent Cardiol" "fecha" => "2011" "volumen" => "79" "paginaInicial" => "111" "paginaFinal" => "116" ] ] ] ] ] ] 18 => array:3 [ "identificador" => "bib0095" "etiqueta" => "[19]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Guía ESC/ESH 2018 sobre el diagnóstico y tratamiento de la hipertensión arterial" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:1 [ 0 => "Grupo de Trabajo de la Sociedad Europea de Cardiología (ESC) y la European Society of Hypertension (ESH)" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.rec.2018.12.004" "Revista" => array:7 [ "tituloSerie" => "Rev Esp Cardiol" "fecha" => "2019" "volumen" => "72" "paginaInicial" => "160.e1" "paginaFinal" => "160.e78" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/30704723" "web" => "Medline" ] ] "itemHostRev" => array:3 [ "pii" => "S0168827815002597" "estado" => "S300" "issn" => "01688278" ] ] ] ] ] ] ] 19 => array:3 [ "identificador" => "bib0100" "etiqueta" => "[20]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Consenso Argentino de Hipertensión Arterial" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:1 [ 0 => "Sociedad Argentina de Cardiología, Federación Argentina de Cardiología y Sociedad Argentina de Hipertensión Arterial" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "Rev Argent Cardiol" "fecha" => "2018" "volumen" => "86" "paginaInicial" => "1" "paginaFinal" => "53" "itemHostRev" => array:3 [ "pii" => "S0168827820303810" "estado" => "S300" "issn" => "01688278" ] ] ] ] ] ] ] 20 => array:3 [ "identificador" => "bib0105" "etiqueta" => "[21]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Cuantificación de la rigidez arterial: de lo básico a lo clínico" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "P. Forcada" 1 => "E. Melgarejo" 2 => "D. Echeverri" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "Rev Colomb Cardiol" "fecha" => "2015" "volumen" => "22" "paginaInicial" => "69" "paginaFinal" => "71" "itemHostRev" => array:3 [ "pii" => "S0168827818319664" "estado" => "S300" "issn" => "01688278" ] ] ] ] ] ] ] 21 => array:3 [ "identificador" => "bib0110" "etiqueta" => "[22]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Use of medication for cardiovascular disease during pregnancy" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:6 [ 0 => "D.G. Halpern" 1 => "C.R. Weinberg" 2 => "R. Pinnelas" 3 => "S. Mehta-Lee" 4 => "K.E. Economy" 5 => "A.M. Valente" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.jacc.2018.10.075" "Revista" => array:6 [ "tituloSerie" => "J Am Coll Cardiol" "fecha" => "2019" "volumen" => "73" "paginaInicial" => "457" "paginaFinal" => "476" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/30704579" "web" => "Medline" ] ] ] ] ] ] ] ] 22 => array:3 [ "identificador" => "bib0115" "etiqueta" => "[23]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "ESC Guidelines for the management of cardiovascular diseases during pregnancy" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:1 [ 0 => "European Society of Cardiology (ESC)" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1093/eurheartj/ehy340" "Revista" => array:6 [ "tituloSerie" => "Eur Heart J" "fecha" => "2018" "volumen" => "39" "paginaInicial" => "3165" "paginaFinal" => "3241" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/30165544" "web" => "Medline" ] ] ] ] ] ] ] ] 23 => array:3 [ "identificador" => "bib0120" "etiqueta" => "[24]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Tratamiento farmacológico de la hipertensión arterial no severa durante el embarazo, el posparto y la lactancia" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "A.M. Ghelfi" 1 => "M.V. Ferretti" 2 => "G.J. Staffieri" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.hipert.2021.01.002" "Revista" => array:6 [ "tituloSerie" => "Hipertens Riesgo Vasc" "fecha" => "2021" "volumen" => "38" "paginaInicial" => "133" "paginaFinal" => "147" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/33632659" "web" => "Medline" ] ] ] ] ] ] ] ] 24 => array:3 [ "identificador" => "bib0125" "etiqueta" => "[25]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Hypertension in pregnancy: diagnosis and management NICE guideline" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:1 [ 0 => "National Institute for Health and Care Excellence (NICE)" ] ] ] ] ] "host" => array:2 [ 0 => array:1 [ "Libro" => array:1 [ "fecha" => "2019" ] ] 1 => array:1 [ "WWW" => array:1 [ "link" => "https://www.nice.org.uk/guidance/ng133" ] ] ] ] ] ] 25 => array:3 [ "identificador" => "bib0130" "etiqueta" => "[26]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Teratogenicity of angiotensin converting enzyme inhibitors or receptor blockers" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:5 [ 0 => "A. Walfisch" 1 => "A. Al-maawali" 2 => "M.E. Moretti" 3 => "C. Nickel" 4 => "G. Koren" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.3109/01443615.2011.579197" "Revista" => array:6 [ "tituloSerie" => "J Obstet Gynaecol" "fecha" => "2011" "volumen" => "31" "paginaInicial" => "465" "paginaFinal" => "472" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/21823839" "web" => "Medline" ] ] ] ] ] ] ] ] 26 => array:3 [ "identificador" => "bib0135" "etiqueta" => "[27]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Maternal exposure to angiotensin converting enzyme inhibitors in the first trimester and risk of malformations in offspring: a retrospective cohort study" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:5 [ 0 => "D.K. Li" 1 => "C. Yang" 2 => "S. Andrade" 3 => "V. Tavares" 4 => "J.R. Ferber" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:3 [ "tituloSerie" => "BMJ" "fecha" => "2011" "volumen" => "343" ] ] ] ] ] ] 27 => array:3 [ "identificador" => "bib0140" "etiqueta" => "[28]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Postpartum hypertension" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "K. Powles" 1 => "S. Gandhi" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1503/cmaj.171389" "Revista" => array:4 [ "tituloSerie" => "CMAJ" "fecha" => "2017" "volumen" => "189" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/29229709" "web" => "Medline" ] ] ] ] ] ] ] ] 28 => array:3 [ "identificador" => "bib0145" "etiqueta" => "[29]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Recomendaciones de seguimiento a partir del “cuarto trimestre” de mujeres con complicaciones vasculares y metabólicas durante el embarazo. Documento de consenso de la SEC, SEMERGEN, semFYC y SEGO" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "A. Castro Conde" 1 => "M. Goya" 2 => "J.L. Delgado Marín" 3 => "N. Martínez Sánchez" 4 => "V. Pallarés Carratalá" 5 => "J.C. Obaya" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Rec Cardioclinics" "fecha" => "2019" "volumen" => "55" "paginaInicial" => "38" "paginaFinal" => "46" ] ] ] ] ] ] 29 => array:3 [ "identificador" => "bib0150" "etiqueta" => "[30]" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Adverse pregnancy outcomes and cardiovascular disease risk: unique opportunities for cardiovascular disease prevention in women: a scientific statement from the American Heart Association" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "N.I. Parikh" 1 => "J.M. Gonzalez" 2 => "C.A.M. Anderson" 3 => "S.E. Judd" 4 => "K.M. Rexrode" 5 => "M.A. Hlatky" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1161/CIR.0000000000000961" "Revista" => array:6 [ "tituloSerie" => "Circulation" "fecha" => "2021" "volumen" => "143" "paginaInicial" => "e902" "paginaFinal" => "e916" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/33779213" "web" => "Medline" ] ] ] ] ] ] ] ] ] ] ] ] ] "idiomaDefecto" => "en" "url" => "/23870206/0000015900000002/v1_202207200641/S2387020622003102/v1_202207200641/en/main.assets" "Apartado" => array:4 [ "identificador" => "44145" "tipo" => "SECCION" "en" => array:2 [ "titulo" => "Special article" "idiomaDefecto" => true ] "idiomaDefecto" => "en" ] "PDF" => "https://static.elsevier.es/multimedia/23870206/0000015900000002/v1_202207200641/S2387020622003102/v1_202207200641/en/main.pdf?idApp=UINPBA00004N&text.app=https://www.elsevier.es/" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020622003102?idApp=UINPBA00004N" ]
Journal Information
Vol. 159. Issue 2.
Pages 101-105 (July 2022)
Share
Download PDF
More article options
Vol. 159. Issue 2.
Pages 101-105 (July 2022)
Special article
Hypertension in non-pregnant women of childbearing age
Hipertensión arterial en la mujer en edad fértil no gestante
Visits
1
This item has received
Article information
These are the options to access the full texts of the publication Medicina Clínica (English Edition)
Subscriber
Subscribe
Purchase
Contact
Phone for subscriptions and reporting of errors
From Monday to Friday from 9 a.m. to 6 p.m. (GMT + 1) except for the months of July and August which will be from 9 a.m. to 3 p.m.
Calls from Spain
932 415 960
Calls from outside Spain
+34 932 415 960
E-mail