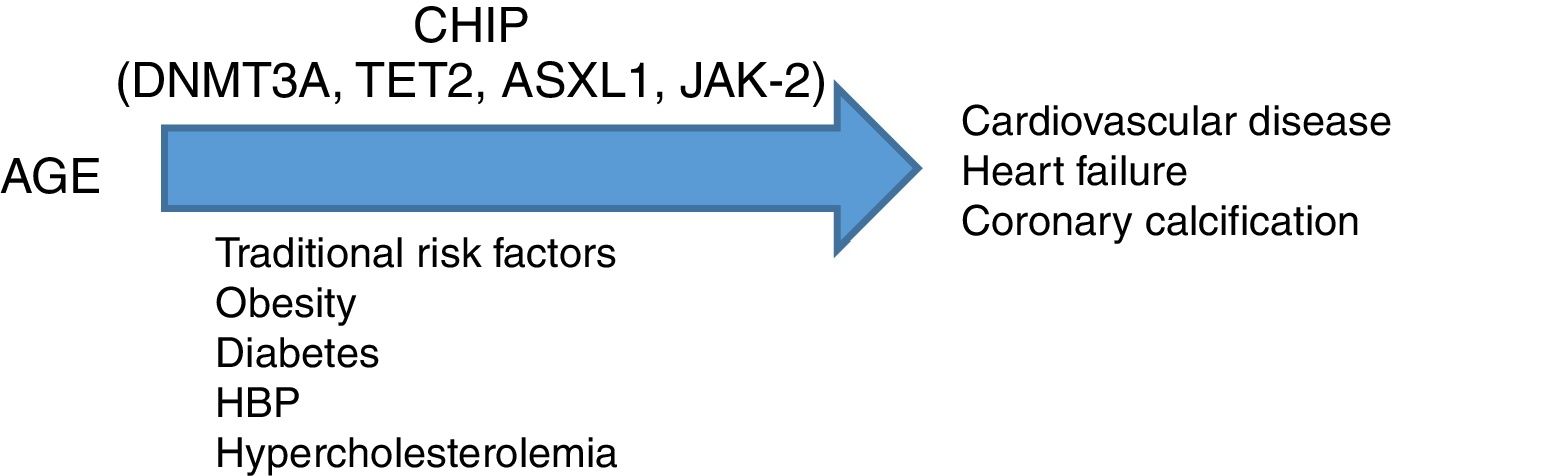
array:24 [ "pii" => "S2387020618303127" "issn" => "23870206" "doi" => "10.1016/j.medcle.2018.07.006" "estado" => "S300" "fechaPublicacion" => "2018-09-14" "aid" => "4507" "copyright" => "Elsevier España, S.L.U.. All rights reserved" "copyrightAnyo" => "2018" "documento" => "article" "crossmark" => 1 "subdocumento" => "sco" "cita" => "Med Clin. 2018;151:207-9" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "Traduccion" => array:1 [ "es" => array:19 [ "pii" => "S0025775318302471" "issn" => "00257753" "doi" => "10.1016/j.medcli.2018.04.007" "estado" => "S300" "fechaPublicacion" => "2018-09-14" "aid" => "4507" "copyright" => "Elsevier España, S.L.U." "documento" => "article" "crossmark" => 1 "subdocumento" => "sco" "cita" => "Med Clin. 2018;151:207-9" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:2 [ "total" => 26 "formatos" => array:2 [ "HTML" => 13 "PDF" => 13 ] ] "es" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Artículo especial</span>" "titulo" => "¿Es la hematopoyesis clonal un nuevo factor de riesgo en enfermedades cardiovasculares?: evidencias clínicas y experimentales" "tienePdf" => "es" "tieneTextoCompleto" => "es" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "207" "paginaFinal" => "209" ] ] "titulosAlternativos" => array:1 [ "en" => array:1 [ "titulo" => "Is clonal hematopoiesis a new risk factor for cardiovascular diseases?: Clinical and experimental evidences" ] ] "contieneTextoCompleto" => array:1 [ "es" => true ] "contienePdf" => array:1 [ "es" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Figura 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 468 "Ancho" => 1558 "Tamanyo" => 63766 ] ] "descripcion" => array:1 [ "es" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">La hematopoyesis clonal de potencial indeterminado ¿nexo entre edad y enfermedades cardiovasculares?</p> <p id="spar0010" class="elsevierStyleSimplePara elsevierViewall">CHIP: hematopoyesis clonal de potencial indeterminado.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Jose A. Páramo Fernandez" "autores" => array:1 [ 0 => array:2 [ "nombre" => "Jose A." "apellidos" => "Páramo Fernandez" ] ] ] ] ] "idiomaDefecto" => "es" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S2387020618303127" "doi" => "10.1016/j.medcle.2018.07.006" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020618303127?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775318302471?idApp=UINPBA00004N" "url" => "/00257753/0000015100000005/v2_201810230632/S0025775318302471/v2_201810230632/es/main.assets" ] ] "itemSiguiente" => array:19 [ "pii" => "S2387020618303139" "issn" => "23870206" "doi" => "10.1016/j.medcle.2018.07.007" "estado" => "S300" "fechaPublicacion" => "2018-09-14" "aid" => "4428" "copyright" => "Elsevier España, S.L.U." "documento" => "article" "crossmark" => 1 "subdocumento" => "pgl" "cita" => "Med Clin. 2018;151:210.e1-210.e13" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:13 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Consensus statement</span>" "titulo" => "Tromboc@t Working Group recommendations for management in patients receiving direct oral anticoagulants" "tienePdf" => "en" "tieneTextoCompleto" => "en" "tieneResumen" => array:2 [ 0 => "en" 1 => "es" ] "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "210.e1" "paginaFinal" => "210.e13" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Recomendaciones del Grupo Catalán de Trombosis (Tromboc@t Working Group) para el tratamiento de los pacientes que reciben anticoagulantes orales directos" ] ] "contieneResumen" => array:2 [ "en" => true "es" => true ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0015" "etiqueta" => "Figure 3" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr3.jpeg" "Alto" => 3099 "Ancho" => 2383 "Tamanyo" => 725352 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0055" class="elsevierStyleSimplePara elsevierViewall">Perioperative approach for patients anticoagulated with DOAC.<span class="elsevierStyleSup">*</span>Assess DOAC withdrawal one more day, depending on the risk of bleeding. **Assess delaying the restart of DOAC one more day, depending on haemostatic safety. Do not administer LMWH or UFH after the discontinuation of DOAC in the preoperative period.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Pável Olivera, Miren Gabilondo, Mireia Constans, Dolors Tàssies, Esther Plensa, Verónica Pons, Germán Las Heras, Carmen Jiménez, Desirée Campoy, Anna Bustins, Artur Oliver, Cristina Marzo, Tania Canals, Anna Varela, Marc Sorigue, Eva Sánchez, Gabriela Ene, Granada Perea, Laura Vicente, Meritxell López, María Cerdá, Erik Johansson, M. Reyes Aguinaco, Nazly Santos, José Mateo, Joan Carles Reverter, Ángel Moya, Amparo Santamaría" "autores" => array:28 [ 0 => array:2 [ "nombre" => "Pável" "apellidos" => "Olivera" ] 1 => array:2 [ "nombre" => "Miren" "apellidos" => "Gabilondo" ] 2 => array:2 [ "nombre" => "Mireia" "apellidos" => "Constans" ] 3 => array:2 [ "nombre" => "Dolors" "apellidos" => "Tàssies" ] 4 => array:2 [ "nombre" => "Esther" "apellidos" => "Plensa" ] 5 => array:2 [ "nombre" => "Verónica" "apellidos" => "Pons" ] 6 => array:2 [ "nombre" => "Germán" "apellidos" => "Las Heras" ] 7 => array:2 [ "nombre" => "Carmen" "apellidos" => "Jiménez" ] 8 => array:2 [ "nombre" => "Desirée" "apellidos" => "Campoy" ] 9 => array:2 [ "nombre" => "Anna" "apellidos" => "Bustins" ] 10 => array:2 [ "nombre" => "Artur" "apellidos" => "Oliver" ] 11 => array:2 [ "nombre" => "Cristina" "apellidos" => "Marzo" ] 12 => array:2 [ "nombre" => "Tania" "apellidos" => "Canals" ] 13 => array:2 [ "nombre" => "Anna" "apellidos" => "Varela" ] 14 => array:2 [ "nombre" => "Marc" "apellidos" => "Sorigue" ] 15 => array:2 [ "nombre" => "Eva" "apellidos" => "Sánchez" ] 16 => array:2 [ "nombre" => "Gabriela" "apellidos" => "Ene" ] 17 => array:2 [ "nombre" => "Granada" "apellidos" => "Perea" ] 18 => array:2 [ "nombre" => "Laura" "apellidos" => "Vicente" ] 19 => array:2 [ "nombre" => "Meritxell" "apellidos" => "López" ] 20 => array:2 [ "nombre" => "María" "apellidos" => "Cerdá" ] 21 => array:2 [ "nombre" => "Erik" "apellidos" => "Johansson" ] 22 => array:2 [ "nombre" => "M. Reyes" "apellidos" => "Aguinaco" ] 23 => array:2 [ "nombre" => "Nazly" "apellidos" => "Santos" ] 24 => array:2 [ "nombre" => "José" "apellidos" => "Mateo" ] 25 => array:2 [ "nombre" => "Joan Carles" "apellidos" => "Reverter" ] 26 => array:2 [ "nombre" => "Ángel" "apellidos" => "Moya" ] 27 => array:2 [ "nombre" => "Amparo" "apellidos" => "Santamaría" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0025775318300721" "doi" => "10.1016/j.medcli.2018.01.022" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775318300721?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020618303139?idApp=UINPBA00004N" "url" => "/23870206/0000015100000005/v1_201810040625/S2387020618303139/v1_201810040625/en/main.assets" ] "itemAnterior" => array:19 [ "pii" => "S2387020618303061" "issn" => "23870206" "doi" => "10.1016/j.medcle.2018.07.005" "estado" => "S300" "fechaPublicacion" => "2018-09-14" "aid" => "4377" "copyright" => "Elsevier España, S.L.U." "documento" => "article" "crossmark" => 1 "subdocumento" => "rev" "cita" => "Med Clin. 2018;151:198-206" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:13 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Review</span>" "titulo" => "Direct oral anticoagulants: An update" "tienePdf" => "en" "tieneTextoCompleto" => "en" "tieneResumen" => array:2 [ 0 => "en" 1 => "es" ] "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "198" "paginaFinal" => "206" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Anticoagulantes orales directos: puesta al día" ] ] "contieneResumen" => array:2 [ "en" => true "es" => true ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 2183 "Ancho" => 2294 "Tamanyo" => 306869 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0015" class="elsevierStyleSimplePara elsevierViewall">Proposal for the election of direct oral anticoagulants according to subgroups of patients.</p> <p id="spar0020" class="elsevierStyleSimplePara elsevierViewall">DOAC: direct oral anticoagulants; VKA: vitamin K antagonists; AF: atrial fibrillation.</p> <p id="spar0025" class="elsevierStyleSimplePara elsevierViewall"><span class="elsevierStyleSup">a</span>Non-valvular atrial fibrillation is considered atrial fibrillation in the absence of rheumatic mitral stenosis, mechanical or biological valvular prosthesis, or mitral valve repair.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Ana Isabel Franco Moreno, Rosa María Martín Díaz, María José García Navarro" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Ana Isabel" "apellidos" => "Franco Moreno" ] 1 => array:2 [ "nombre" => "Rosa María" "apellidos" => "Martín Díaz" ] 2 => array:2 [ "nombre" => "María José" "apellidos" => "García Navarro" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0025775317309260" "doi" => "10.1016/j.medcli.2017.11.042" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775317309260?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020618303061?idApp=UINPBA00004N" "url" => "/23870206/0000015100000005/v1_201810040625/S2387020618303061/v1_201810040625/en/main.assets" ] "en" => array:17 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Special article</span>" "titulo" => "Is clonal hematopoiesis a new risk factor for cardiovascular diseases?: Clinical and experimental evidences" "tieneTextoCompleto" => true "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "207" "paginaFinal" => "209" ] ] "autores" => array:1 [ 0 => array:3 [ "autoresLista" => "Jose A. Páramo Fernandez" "autores" => array:1 [ 0 => array:3 [ "nombre" => "Jose A." "apellidos" => "Páramo Fernandez" "email" => array:1 [ 0 => "japaramo@unav.es" ] ] ] "afiliaciones" => array:1 [ 0 => array:2 [ "entidad" => "Servicio de Hematología, Clínica Universidad de Navarra, Laboratorio Aterotrombosis, CIMA, Universidad de Navarra, Pamplona, Spain" "identificador" => "aff0005" ] ] ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "¿Es la hematopoyesis clonal un nuevo factor de riesgo en enfermedades cardiovasculares?: evidencias clínicas y experimentales" ] ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 476 "Ancho" => 1558 "Tamanyo" => 57938 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Clonal haematopoiesis of indetermined potential; a link between age and cardiovascular diseases?</p> <p id="spar0010" class="elsevierStyleSimplePara elsevierViewall">CHIP: Clonal haematopoiesis of indetermined potential.</p>" ] ] ] "textoCompleto" => "<span class="elsevierStyleSections"><span id="sec0005" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0005">New concepts in atherogenesis and vulnerability</span><p id="par0005" class="elsevierStylePara elsevierViewall">Cardiovascular disease, the main cause of mortality in the world, is caused by atherothrombotic vascular occlusion, responsible for clinical symptoms as important as unstable angina, myocardial infarction, sudden death and stroke.<a class="elsevierStyleCrossRef" href="#bib0155"><span class="elsevierStyleSup">1</span></a> Atherosclerosis is an inflammatory disease in which various mechanisms are involved, such as endothelial and leukocyte activation and oxidative stress.<a class="elsevierStyleCrossRefs" href="#bib0160"><span class="elsevierStyleSup">2,3</span></a> Classic histopathological studies in patients who died of an acute coronary syndrome (ACS) revealed that the size of the necrotic nucleus, a thin fibrous capsule and abundant inflammatory infiltrate were the characteristics of the plaque that contributed in a decisive way to the occurrence of thrombosis,<a class="elsevierStyleCrossRef" href="#bib0170"><span class="elsevierStyleSup">4</span></a> coining the concept of “vulnerable” plaque to define those with greater propensity to rupture.<a class="elsevierStyleCrossRef" href="#bib0175"><span class="elsevierStyleSup">5</span></a> However, this concept is changing in the light of new findings and, at present, has reduced its clinical relevance.<a class="elsevierStyleCrossRef" href="#bib0180"><span class="elsevierStyleSup">6</span></a> Recent evidence indicates that numerous plaques with a thin fibrous capsule and a large lipid content hardly experience rupture; in addition, intravascular imaging studies have shown that thin plaques do not inevitably lead to a thrombotic risk.<a class="elsevierStyleCrossRef" href="#bib0185"><span class="elsevierStyleSup">7</span></a> On the other hand, the Athero-Express study, aimed at determining the characteristics of endarterectomy plaque associated with cardiovascular events in the period of 2002–2014, observed a significant decrease in “vulnerable” plaques and a 15% reduction in lipid content in relation to previous studies.<a class="elsevierStyleCrossRef" href="#bib0190"><span class="elsevierStyleSup">8</span></a></p><p id="par0010" class="elsevierStylePara elsevierViewall">The causes that may have led to the transition from “vulnerable” plaque to “stable” plaque would be<a class="elsevierStyleCrossRefs" href="#bib0180"><span class="elsevierStyleSup">6,9</span></a>:<ul class="elsevierStyleList" id="lis0005"><li class="elsevierStyleListItem" id="lsti0005"><span class="elsevierStyleLabel">-</span><p id="par0015" class="elsevierStylePara elsevierViewall">The increase in the use of statins, as well as a better knowledge and control of cardiovascular risk factors that have modified the natural history of atherosclerotic disease.</p></li><li class="elsevierStyleListItem" id="lsti0010"><span class="elsevierStyleLabel">-</span><p id="par0020" class="elsevierStylePara elsevierViewall">Presence of more fibrotic plaques with less inflammation (“stable” plaques).</p></li><li class="elsevierStyleListItem" id="lsti0015"><span class="elsevierStyleLabel">-</span><p id="par0025" class="elsevierStylePara elsevierViewall">Lower prevalence of plaque rupture in patients with ACS and increased surface erosion, referred to as endothelial dysfunction, without rupture.</p></li><li class="elsevierStyleListItem" id="lsti0020"><span class="elsevierStyleLabel">-</span><p id="par0030" class="elsevierStylePara elsevierViewall">Lower incidence of ACS with ST-segment elevation and greater presence of ACS without elevation, as well as a decrease in stroke.</p></li><li class="elsevierStyleListItem" id="lsti0025"><span class="elsevierStyleLabel">-</span><p id="par0035" class="elsevierStylePara elsevierViewall">Change in the risk profile and demographics of patients, with a greater presence of young subjects, more women, more resistance to insulin/diabetes, more hypertriglyceridemia and less excess of LDL cholesterol.</p></li><li class="elsevierStyleListItem" id="lsti0030"><span class="elsevierStyleLabel">-</span><p id="par0040" class="elsevierStylePara elsevierViewall">It is possible to detect lesions with characteristics of vulnerability in arteries of patients without clinical manifestations. Approximately 75% of coronary or peripheral atherosclerotic plaques in individuals without clinical manifestations show signs of inflammation, with an increase in leukocyte activation markers. A recent study has shown that gene expression of circulating leukocytes is significantly different between coronary arteries and systemic circulation in patients with coronary disease, but not in its absence, suggesting that regional differences in RNA expression may represent a distinctive pattern in patients with atherosclerosis.<a class="elsevierStyleCrossRef" href="#bib0200"><span class="elsevierStyleSup">10</span></a></p></li></ul></p></span><span id="sec0010" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0010">Inflammation in atherosclerosis: a bidirectional relationship</span><p id="par0045" class="elsevierStylePara elsevierViewall">A unified and current vision of the pathophysiology of atherosclerosis suggests that inflammation plays a key role in the different phases of the process.<a class="elsevierStyleCrossRef" href="#bib0160"><span class="elsevierStyleSup">2</span></a> The discovery of T lymphocytes in human atherosclerotic plaques, and the subsequent identification of all cell types involved in innate and acquired immunity, confirm the involvement of the immune system. Thus, T-<span class="elsevierStyleItalic">helper</span> cells produce proinflammatory cytokines such as tumor necrosis factor-α, interleukin (IL)-1β and interferon-γ, with powerful proatherosclerotic action, while anti-inflammatory cytokines, such as IL-10 and transforming growth factor-β, try to balance these actions.<a class="elsevierStyleCrossRef" href="#bib0205"><span class="elsevierStyleSup">11</span></a></p><p id="par0050" class="elsevierStylePara elsevierViewall">The knowledge of the role of inflammation in atherosclerosis offers the possibility of using strategies aimed at the stabilization of the plaque, independently of the degree of stenosis.<a class="elsevierStyleCrossRefs" href="#bib0210"><span class="elsevierStyleSup">12,13</span></a></p></span><span id="sec0015" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0015">The myeloid component of atherosclerosis</span><p id="par0055" class="elsevierStylePara elsevierViewall">Taking into account the role of inflammation in atherosclerosis, the participation of the myeloid component is logical in all stages of this process, from the initial stages to progression and, finally, to the thrombotic consequences of the disease. Recent research involves several monocytic subpopulations, the most abundant myeloid cells in the atherosclerotic plaque, as well as an increase in hematopoietic activity.<a class="elsevierStyleCrossRef" href="#bib0220"><span class="elsevierStyleSup">14</span></a> The myeloid cells will contribute to initiate thrombosis, producing enzymes that degrade the ECM and tissue factor, the main initiator of blood coagulation.<a class="elsevierStyleCrossRef" href="#bib0225"><span class="elsevierStyleSup">15</span></a> In addition to monocytes, neutrophils can aggravate thrombosis locally by creating <span class="elsevierStyleItalic">neutrophil extracellular traps</span> that, in addition to being present in atherosclerotic lesions, will promote the growth and persistence of the thrombus by inducing procoagulant factors and amplifying inflammation, activating inflammasome and generating IL-1β.<a class="elsevierStyleCrossRefs" href="#bib0230"><span class="elsevierStyleSup">16,17</span></a> Therefore, the myeloid component, resulting from an increased hematopoietic activity, will be relevant in the inflammatory and thrombotic processes characteristic of atherothrombosis. It is interesting to note that recent studies are analysing the role of anti-inflammatory strategies which could prevent the development of atherosclerosis by modulating innate immunity (for example, canakinumab, an IL-1 antagonistβ, CANTOS study).<a class="elsevierStyleCrossRef" href="#bib0240"><span class="elsevierStyleSup">18</span></a></p></span><span id="sec0020" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0020">Significance of clonal haematopoiesis of indetermined potential in cardiovascular diseases</span><p id="par0060" class="elsevierStylePara elsevierViewall">Research carried out in recent years using various genomic techniques has shown that clonal haematopoiesis of indetermined potential (CHIP), the result of somatic mutations, is not only a frequent process related to age and a premalignant state, but a condition that predisposes to the development of cardiovascular diseases.<a class="elsevierStyleCrossRef" href="#bib0245"><span class="elsevierStyleSup">19</span></a> This is a finding of great importance, due to the possibility of identifying new targets of interest in the prevention and/or treatment of these diseases.</p><p id="par0065" class="elsevierStylePara elsevierViewall">Somatic mutations are uncommon before the age of 40 but are present in 10–20% of the subjects over 70 years of age; most consist of a single mutation, with DNMT3A being the most common, followed by TET2 and ASLX1. Other less frequent mutations are TP53, JAK-2, SF3B1 and BCOR.<a class="elsevierStyleCrossRefs" href="#bib0250"><span class="elsevierStyleSup">20,21</span></a> Somatic mutations in clonal haematopoiesis persist over time and are considered a premalignant state, with similarities with other clonal hematopoietic disorders, such as monoclonal gammopathy of undetermined significance, monoclonal B lymphocytosis, myelodysplastic syndromes or paroxysmal nocturnal hemoglobinuria.<a class="elsevierStyleCrossRef" href="#bib0260"><span class="elsevierStyleSup">22</span></a> The great majority of mutations in clonal haematopoiesis affect genes involved in epigenetic regulation; for example, DNMT3A and TET2 regulate DNA methylation and inflammatory processes.<a class="elsevierStyleCrossRefs" href="#bib0265"><span class="elsevierStyleSup">23–25</span></a></p><p id="par0070" class="elsevierStylePara elsevierViewall">CHIP is characterized, therefore, by the expansion of hematopoietic clones carrying somatic mutations, which confer a selective advantage with clonal expansion of granulocytic, lymphocytic and monocytic cells. It has been previously associated with advanced age and with an increased risk of hematological malignancies.<a class="elsevierStyleCrossRefs" href="#bib0250"><span class="elsevierStyleSup">20,22</span></a> Recent studies also indicate that the presence of CHIP is associated with accelerated atherosclerosis in mice and with a high risk of coronary heart disease in humans.<a class="elsevierStyleCrossRefs" href="#bib0280"><span class="elsevierStyleSup">26,27</span></a> The connection between CHIP and cardiovascular disease was recently demonstrated by Jaiswall et al.,<a class="elsevierStyleCrossRef" href="#bib0280"><span class="elsevierStyleSup">26</span></a> in large series of patients from prospective (BioImage and MDC) and retrospective (ATVB and PROMIS) studies in 4726 patients with coronary artery disease and 3529 healthy controls. Mutations were observed in ASXL1, TET2, DNMT3A and JAK-2 associated with an elevated risk of ischemic heart disease (HR 2.0), ischemic stroke (HR 2.6) and coronary calcification. It is interesting to note that the cardiovascular risk attributable to CHIP was comparable or superior in magnitude to that of traditional cardiovascular risk factors, such as hypertension, hypercholesterolemia and smoking. The association between CHIP and cardiovascular diseases may be due to variables not yet identified or share physiopathological aspects with the senescence process, such as vascular inflammation. In this sense, the fact that TET2 negatively regulates IL-6 suggests that somatic mutations in TET2 may favor inflammatory processes.<a class="elsevierStyleCrossRefs" href="#bib0265"><span class="elsevierStyleSup">23,25</span></a></p><p id="par0075" class="elsevierStylePara elsevierViewall">To study causality, experimental studies were carried out in LDLr-/- mice (developing spontaneous or diet-induced atherosclerosis), which were transplanted with bone marrow from mice (TET2-/-). The animals were subjected to a high-fat diet for 10 weeks and both the expression of genes and proteins expressed in macrophages and the histological and immunohistochemical study of the atherosclerotic lesion were analyzed. The results showed a higher degree of atherosclerosis at the aortic arch level, as well as the production of cytokines (IL1β, inflammasome) in TET2-/- mice, establishing a mechanism by which mutations or deletion of TET2 can contribute to increased cardiovascular risk.<a class="elsevierStyleCrossRefs" href="#bib0280"><span class="elsevierStyleSup">26,27</span></a> Experimental studies have also shown that TET2-mediated clonal haematopoiesis accelerates the onset of heart failure, by inflammatory mechanisms linked to inflammasome.<a class="elsevierStyleCrossRef" href="#bib0290"><span class="elsevierStyleSup">28</span></a></p></span><span id="sec0025" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0025">Clonal haematopoiesis of indetermined potential: a new therapeutic target in atherosclerosis?</span><p id="par0080" class="elsevierStylePara elsevierViewall">Atherosclerosis, far from being considered an irreversible process associated with aging, is postulated as a condition that can be stopped or even reversed.<a class="elsevierStyleCrossRefs" href="#bib0210"><span class="elsevierStyleSup">12,13</span></a> In this sense, statins exert a beneficial effect on the composition of the plaque, rather than on the degree of stenosis. In addition, the protective action that a strict control over cardiovascular risk factors and heart-healthy lifestyles exerts on the atherosclerotic process could be mediated by its action on hematopoiesis.<a class="elsevierStyleCrossRef" href="#bib0295"><span class="elsevierStyleSup">29</span></a> Finally, it has been shown that vitamin <span class="elsevierStyleSmallCaps">C</span> restores TET2 activity in some types of leukemias and downregulates the expression of apolipoprotein (a) via TET2, which could explain some of its antiatherogenic actions.<a class="elsevierStyleCrossRef" href="#bib0300"><span class="elsevierStyleSup">30</span></a></p></span><span id="sec0030" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0030">Conclusion</span><p id="par0085" class="elsevierStylePara elsevierViewall">Somatic mutations in genes that are described in patients with hematologic malignancies can be frequently detected in the blood of healthy elderly subjects. CHIP is associated with coronary artery disease and the degree of atherosclerosis (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>). CHIP emerges as a new risk factor for atherosclerotic disease, ischemic heart disease and heart failure, so its detection in clinical practice can have important therapeutic implications, since it will allow the identification of new targets aimed at personalized medicine.</p><elsevierMultimedia ident="fig0005"></elsevierMultimedia></span><span id="sec0035" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0035">Conflict of interests</span><p id="par0090" class="elsevierStylePara elsevierViewall">The author declares no conflict of interest.</p></span></span>" "textoCompletoSecciones" => array:1 [ "secciones" => array:8 [ 0 => array:2 [ "identificador" => "sec0005" "titulo" => "New concepts in atherogenesis and vulnerability" ] 1 => array:2 [ "identificador" => "sec0010" "titulo" => "Inflammation in atherosclerosis: a bidirectional relationship" ] 2 => array:2 [ "identificador" => "sec0015" "titulo" => "The myeloid component of atherosclerosis" ] 3 => array:2 [ "identificador" => "sec0020" "titulo" => "Significance of clonal haematopoiesis of indetermined potential in cardiovascular diseases" ] 4 => array:2 [ "identificador" => "sec0025" "titulo" => "Clonal haematopoiesis of indetermined potential: a new therapeutic target in atherosclerosis?" ] 5 => array:2 [ "identificador" => "sec0030" "titulo" => "Conclusion" ] 6 => array:2 [ "identificador" => "sec0035" "titulo" => "Conflict of interests" ] 7 => array:1 [ "titulo" => "References" ] ] ] "pdfFichero" => "main.pdf" "tienePdf" => true "fechaRecibido" => "2018-02-19" "fechaAceptado" => "2018-04-10" "NotaPie" => array:1 [ 0 => array:2 [ "etiqueta" => "☆" "nota" => "<p class="elsevierStyleNotepara" id="npar0005">Please cite this article as: Páramo Fernandez JA. ¿Es la hematopoyesis clonal un nuevo factor de riesgo en enfermedades cardiovasculares?: evidencias clínicas y experimentales. Med Clin (Barc). 2018;151:207–209.</p>" ] ] "multimedia" => array:1 [ 0 => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 476 "Ancho" => 1558 "Tamanyo" => 57938 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Clonal haematopoiesis of indetermined potential; a link between age and cardiovascular diseases?</p> <p id="spar0010" class="elsevierStyleSimplePara elsevierViewall">CHIP: Clonal haematopoiesis of indetermined potential.</p>" ] ] ] "bibliografia" => array:2 [ "titulo" => "References" "seccion" => array:1 [ 0 => array:2 [ "identificador" => "bibs0015" "bibliografiaReferencia" => array:30 [ 0 => array:3 [ "identificador" => "bib0155" "etiqueta" => "1" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Causes of Death Collaborators Global, regional, and national life expectancy, all-cause mortality and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:1 [ 0 => "2015 Mortality G.B.D." ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/S0140-6736(16)31012-1" "Revista" => array:6 [ "tituloSerie" => "Lancet" "fecha" => "2016" "volumen" => "388" "paginaInicial" => "1459" "paginaFinal" => "1544" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/27733281" "web" => "Medline" ] ] ] ] ] ] ] ] 1 => array:3 [ "identificador" => "bib0160" "etiqueta" => "2" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Inflammation in atherosclerosis" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:1 [ 0 => "P. Libby" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1161/ATVBAHA.108.179705" "Revista" => array:6 [ "tituloSerie" => "Arterioscler Thromb Vasc Biol" "fecha" => "2012" "volumen" => "32" "paginaInicial" => "2045" "paginaFinal" => "2051" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/22895665" "web" => "Medline" ] ] ] ] ] ] ] ] 2 => array:3 [ "identificador" => "bib0165" "etiqueta" => "3" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Aterosclerosis en enfermedades inflamatorias" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "J.A. Páramo" 1 => "J.A. Rodríguez" 2 => "J. Orbe" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Med Clin (Barc)" "fecha" => "2007" "volumen" => "128" "paginaInicial" => "749" "paginaFinal" => "756" ] ] ] ] ] ] 3 => array:3 [ "identificador" => "bib0170" "etiqueta" => "4" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Mechanisms of acute coronary syndromes and implications to therapy" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:1 [ 0 => "P. Libby" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1056/NEJMra1216063" "Revista" => array:6 [ "tituloSerie" => "N Engl J Med" "fecha" => "2013" "volumen" => "368" "paginaInicial" => "2004" "paginaFinal" => "2013" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/23697515" "web" => "Medline" ] ] ] ] ] ] ] ] 4 => array:3 [ "identificador" => "bib0175" "etiqueta" => "5" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Mechanisms of plaque formation and rupture" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "J.F. Bentzon" 1 => "F. Otsuka" 2 => "R. Virmani" 3 => "E. Falk" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1161/CIRCRESAHA.114.302721" "Revista" => array:6 [ "tituloSerie" => "Circ Res" "fecha" => "2014" "volumen" => "114" "paginaInicial" => "1852" "paginaFinal" => "1866" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/24902970" "web" => "Medline" ] ] ] ] ] ] ] ] 5 => array:3 [ "identificador" => "bib0180" "etiqueta" => "6" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Requiem for the vulnerable plaque" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "P. Libby" 1 => "G. Pasterkamp" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1093/eurheartj/ehv349" "Revista" => array:6 [ "tituloSerie" => "Eur Heart J" "fecha" => "2015" "volumen" => "36" "paginaInicial" => "2984" "paginaFinal" => "2987" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/26206212" "web" => "Medline" ] ] ] ] ] ] ] ] 6 => array:3 [ "identificador" => "bib0185" "etiqueta" => "7" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Visualization of coronary atherosclerotic plaques in patients using optical coherence tomography: comparison with intravascular ultrasound" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "I.K. Jang" 1 => "B.E. Bouma" 2 => "D.H. Kang" 3 => "S.J. Park" 4 => "S.W. Park" 5 => "K.B. Seung" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "J Am Coll Cardiol" "fecha" => "2002" "volumen" => "39" "paginaInicial" => "604" "paginaFinal" => "609" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/11849858" "web" => "Medline" ] ] ] ] ] ] ] ] 7 => array:3 [ "identificador" => "bib0190" "etiqueta" => "8" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Time-dependent changes in atherosclerotic plaque composition in patients undergoing carotid surgery" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "G.W. Van Lammeren" 1 => "H.M. den Ruijter" 2 => "J.E. Vrijenhoek" 3 => "S.W. van der Laan" 4 => "E. Velema" 5 => "J.P. de Vries" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1161/CIRCULATIONAHA.113.007603" "Revista" => array:6 [ "tituloSerie" => "Circulation" "fecha" => "2014" "volumen" => "129" "paginaInicial" => "2269" "paginaFinal" => "2276" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/24637558" "web" => "Medline" ] ] ] ] ] ] ] ] 8 => array:3 [ "identificador" => "bib0195" "etiqueta" => "9" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Temporal shifts in clinical presentation and underlying mechanisms of atherosclerotic disease" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "G. Pasterkamp" 1 => "H.M. den Ruijter" 2 => "P. Libby" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1038/nrcardio.2016.166" "Revista" => array:6 [ "tituloSerie" => "Nat Rev Cardiol" "fecha" => "2017" "volumen" => "14" "paginaInicial" => "21" "paginaFinal" => "29" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/27762311" "web" => "Medline" ] ] ] ] ] ] ] ] 9 => array:3 [ "identificador" => "bib0200" "etiqueta" => "10" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Differential leukocyte RNA expression in the coronary arteries compared to systemic circulation discriminate betwen patients with and those without coronary artery disease" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "J. Ribalta" 1 => "A. Alipour" 2 => "F. Sánchez-Cabo" 3 => "J.C. Vallvé" 4 => "T. Njo" 5 => "R. Alvaez" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Clin Invest Arterioscler" "fecha" => "2017" "volumen" => "29" "paginaInicial" => "60" "paginaFinal" => "66" ] ] ] ] ] ] 10 => array:3 [ "identificador" => "bib0205" "etiqueta" => "11" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Adaptive response of T and B cells in atherosclerosis" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "D.F. Ketelhuth" 1 => "G.K. Hansson" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1161/CIRCRESAHA.115.306427" "Revista" => array:6 [ "tituloSerie" => "Circ Res" "fecha" => "2016" "volumen" => "118" "paginaInicial" => "668" "paginaFinal" => "678" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/26892965" "web" => "Medline" ] ] ] ] ] ] ] ] 11 => array:3 [ "identificador" => "bib0210" "etiqueta" => "12" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Estabilización de la placa de ateroma: un nuevo concepto basado en la biología dinámica de la aterosclerosis" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "J.A. Páramo" 1 => "J. Orbe" 2 => "J.A. Rodríguez" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Med Clin (Barc)" "fecha" => "2003" "volumen" => "121" "paginaInicial" => "583" "paginaFinal" => "587" ] ] ] ] ] ] 12 => array:3 [ "identificador" => "bib0215" "etiqueta" => "13" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "¿Es posible la regresión de la placa aterosclerótica?" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "J.A. Páramo" 1 => "F. Civeira" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Clin Invest Arterioscler" "fecha" => "2017" "volumen" => "29" "paginaInicial" => "46" "paginaFinal" => "50" ] ] ] ] ] ] 13 => array:3 [ "identificador" => "bib0220" "etiqueta" => "14" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Monocytes in atherosclerosis: subsets and functions" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "K.J. Woolard" 1 => "F. Geissman" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1038/nrcardio.2009.228" "Revista" => array:6 [ "tituloSerie" => "Nat Rev Cardiol" "fecha" => "2010" "volumen" => "7" "paginaInicial" => "77" "paginaFinal" => "86" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/20065951" "web" => "Medline" ] ] ] ] ] ] ] ] 14 => array:3 [ "identificador" => "bib0225" "etiqueta" => "15" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Tissue factor: an essential mediator of hemostasis and trigger of thrombosis" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "S.P. Grover" 1 => "N. Mackman" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1161/ATVBAHA.117.309846" "Revista" => array:6 [ "tituloSerie" => "Arterioscler Thromb Vasc Biol" "fecha" => "2018" "volumen" => "38" "paginaInicial" => "709" "paginaFinal" => "725" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/29437578" "web" => "Medline" ] ] ] ] ] ] ] ] 15 => array:3 [ "identificador" => "bib0230" "etiqueta" => "16" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Presence of luminal neutrophil extracelular traps in atherosclerosis" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "R.T. Megens" 1 => "S. Viyajan" 2 => "D. Lievens" 3 => "Y. Döring" 4 => "M.A. van Zandvoort" 5 => "J. Grommes" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1160/TH11-09-0650" "Revista" => array:6 [ "tituloSerie" => "Thromb Haemost" "fecha" => "2012" "volumen" => "107" "paginaInicial" => "597" "paginaFinal" => "598" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/22318427" "web" => "Medline" ] ] ] ] ] ] ] ] 16 => array:3 [ "identificador" => "bib0235" "etiqueta" => "17" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Neutrophil extracellular traps in atherosclerosis and atherothrombosis" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "Y. Döring" 1 => "O. Soehnlein" 2 => "C. Weber" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1161/CIRCRESAHA.116.309692" "Revista" => array:6 [ "tituloSerie" => "Circ Res" "fecha" => "2017" "volumen" => "120" "paginaInicial" => "736" "paginaFinal" => "743" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/28209798" "web" => "Medline" ] ] ] ] ] ] ] ] 17 => array:3 [ "identificador" => "bib0240" "etiqueta" => "18" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "CANTOS Trial Group. Antiinflammatory therapy with canakinumab for atherosclerotic disease" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "P.M. Ridker" 1 => "B.M. Everett" 2 => "T. Thuren" 3 => "J.G. MacFadyen" 4 => "W.H. Chang" 5 => "C. Ballantyne" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1056/NEJMoa1707914" "Revista" => array:6 [ "tituloSerie" => "N Engl J Med" "fecha" => "2017" "volumen" => "377" "paginaInicial" => "1119" "paginaFinal" => "1131" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/28845751" "web" => "Medline" ] ] ] ] ] ] ] ] 18 => array:3 [ "identificador" => "bib0245" "etiqueta" => "19" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Somatic mutations and clonal hematopoiesis. Unexpected potential new drivers and age-related cardiovascular disease" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "J.J. Fuster" 1 => "K. Walsh" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Arterioscler Thromb Vasc Biol" "fecha" => "2018" "volumen" => "122" "paginaInicial" => "523" "paginaFinal" => "532" ] ] ] ] ] ] 19 => array:3 [ "identificador" => "bib0250" "etiqueta" => "20" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Age-related clonal hematopoiesis associated with adverse outcomes" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "S. Jaiswal" 1 => "P. Fontanillas" 2 => "J. Flannick" 3 => "A. Manning" 4 => "P.V. Grauman" 5 => "B.G. Mar" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1056/NEJMoa1408617" "Revista" => array:6 [ "tituloSerie" => "N Engl J Med" "fecha" => "2014" "volumen" => "371" "paginaInicial" => "2488" "paginaFinal" => "2498" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/25426837" "web" => "Medline" ] ] ] ] ] ] ] ] 20 => array:3 [ "identificador" => "bib0255" "etiqueta" => "21" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Clonal hematopoiesis, with and without candidate driver mutations, is common in the elderly" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "F. Zink" 1 => "S.N. Stacey" 2 => "G.L. Norddahl" 3 => "M.L. Frigge" 4 => "O.T. Magnusson" 5 => "I. Jonsdottir" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1182/blood-2017-02-769869" "Revista" => array:6 [ "tituloSerie" => "Blood" "fecha" => "2017" "volumen" => "130" "paginaInicial" => "742" "paginaFinal" => "752" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/28483762" "web" => "Medline" ] ] ] ] ] ] ] ] 21 => array:3 [ "identificador" => "bib0260" "etiqueta" => "22" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Clonal hematopoiesis of indeterminate potential and its distinction from myelodysplastic syndromes" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "D.P. Steensma" 1 => "R. Bejar" 2 => "S. Jaiswal" 3 => "R.C. Lindsley" 4 => "M.A. Sekeres" 5 => "R.P. Hasserjian" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1182/blood-2015-03-631747" "Revista" => array:6 [ "tituloSerie" => "Blood" "fecha" => "2015" "volumen" => "126" "paginaInicial" => "9" "paginaFinal" => "16" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/25931582" "web" => "Medline" ] ] ] ] ] ] ] ] 22 => array:3 [ "identificador" => "bib0265" "etiqueta" => "23" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "TET2 restrains inflammatory gene expression in macrophages" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:5 [ 0 => "A.H. Cull" 1 => "B. Snetsinger" 2 => "R. Buckstein" 3 => "R.A. Wells" 4 => "M.J. Raug" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Exp Hematol" "fecha" => "2017" "volumen" => "55" "paginaInicial" => "e13" "paginaFinal" => "e70" ] ] ] ] ] ] 23 => array:3 [ "identificador" => "bib0270" "etiqueta" => "24" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "DNMT3A and TET2 dominate clonal hematopoiesis and demonstrate benign phenotypes and different genetic predisposition" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "M. Buscarlet" 1 => "S. Provost" 2 => "Y.F. Zada" 3 => "A. Barhadi" 4 => "V. Bourgoin" 5 => "G. Lépine" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1182/blood-2017-04-777029" "Revista" => array:6 [ "tituloSerie" => "Blood" "fecha" => "2017" "volumen" => "130" "paginaInicial" => "753" "paginaFinal" => "762" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/28655780" "web" => "Medline" ] ] ] ] ] ] ] ] 24 => array:3 [ "identificador" => "bib0275" "etiqueta" => "25" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "TET2 is required to resolve inflammation by recruiting Hdac2 to specifically repress IL-6" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "Q. Zhang" 1 => "K. Zhao" 2 => "Q. Shen" 3 => "Y. Han" 4 => "Y. Gu" 5 => "X. Li" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1038/nature15252" "Revista" => array:6 [ "tituloSerie" => "Nature" "fecha" => "2015" "volumen" => "525" "paginaInicial" => "389" "paginaFinal" => "393" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/26287468" "web" => "Medline" ] ] ] ] ] ] ] ] 25 => array:3 [ "identificador" => "bib0280" "etiqueta" => "26" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Clonal hematopoiesis and risk of atherosclerotic cardiovascular disease" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "S. Jaiswal" 1 => "P. Natarajan" 2 => "A.J. Silver" 3 => "C.J. Gibson" 4 => "A.G. Bick" 5 => "E. Shvartz" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1056/NEJMoa1701719" "Revista" => array:6 [ "tituloSerie" => "N Engl J Med" "fecha" => "2017" "volumen" => "377" "paginaInicial" => "111" "paginaFinal" => "121" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/28636844" "web" => "Medline" ] ] ] ] ] ] ] ] 26 => array:3 [ "identificador" => "bib0285" "etiqueta" => "27" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Clonal hematopoiesis associated with TET2 deficiency accelerates atherosclerosis development in mice" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "J.J. Fuster" 1 => "S. MacLauchlan" 2 => "M.A. Zuriaga" 3 => "M.N. Polackal" 4 => "A.C. Ostriker" 5 => "R. Chakraborty" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1126/science.aag1381" "Revista" => array:6 [ "tituloSerie" => "Science" "fecha" => "2017" "volumen" => "355" "paginaInicial" => "842" "paginaFinal" => "847" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/28104796" "web" => "Medline" ] ] ] ] ] ] ] ] 27 => array:3 [ "identificador" => "bib0290" "etiqueta" => "28" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Tet2-mediated clonal hematopoiesis accelerates experimental heart failure through and IL-1β/NLRP3 inflammasome mechanism" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "S. Sano" 1 => "K. Ashima" 2 => "Y. Wang" 3 => "S. MacLauchlan" 4 => "Y. Katanasaka" 5 => "M. Sano" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.jacc.2017.12.037" "Revista" => array:6 [ "tituloSerie" => "J Am Coll Cardiol" "fecha" => "2018" "volumen" => "71" "paginaInicial" => "875" "paginaFinal" => "886" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/29471939" "web" => "Medline" ] ] ] ] ] ] ] ] 28 => array:3 [ "identificador" => "bib0295" "etiqueta" => "29" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Lifestyle effects on hematopoiesis and atherosclerosis" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "M. Nahrendorf" 1 => "F.K. Swirski" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1161/CIRCRESAHA.116.303550" "Revista" => array:6 [ "tituloSerie" => "Circ Res" "fecha" => "2015" "volumen" => "116" "paginaInicial" => "884" "paginaFinal" => "894" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/25722442" "web" => "Medline" ] ] ] ] ] ] ] ] 29 => array:3 [ "identificador" => "bib0300" "etiqueta" => "30" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Vitamin C down-regulate apo(a) expression via Tet2-dependent DNA demethylation in HepG2 cells" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "K. Qu" 1 => "X.F. Ma" 2 => "G.H. Li" 3 => "H. Zhang" 4 => "Y.M. Liu" 5 => "K. Zhang" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.ijbiomac.2017.02.025" "Revista" => array:6 [ "tituloSerie" => "Int J Biol Macromol" "fecha" => "2017" "volumen" => "98" "paginaInicial" => "637" "paginaFinal" => "645" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/28192139" "web" => "Medline" ] ] ] ] ] ] ] ] ] ] ] ] ] "idiomaDefecto" => "en" "url" => "/23870206/0000015100000005/v1_201810040625/S2387020618303127/v1_201810040625/en/main.assets" "Apartado" => array:4 [ "identificador" => "44145" "tipo" => "SECCION" "en" => array:2 [ "titulo" => "Special article" "idiomaDefecto" => true ] "idiomaDefecto" => "en" ] "PDF" => "https://static.elsevier.es/multimedia/23870206/0000015100000005/v1_201810040625/S2387020618303127/v1_201810040625/en/main.pdf?idApp=UINPBA00004N&text.app=https://www.elsevier.es/" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020618303127?idApp=UINPBA00004N" ]
Journal Information
Vol. 151. Issue 5.
Pages 207-209 (September 2018)
Share
Download PDF
More article options
Vol. 151. Issue 5.
Pages 207-209 (September 2018)
Special article
Is clonal hematopoiesis a new risk factor for cardiovascular diseases?: Clinical and experimental evidences
¿Es la hematopoyesis clonal un nuevo factor de riesgo en enfermedades cardiovasculares?: evidencias clínicas y experimentales
Visits
87
Jose A. Páramo Fernandez
Servicio de Hematología, Clínica Universidad de Navarra, Laboratorio Aterotrombosis, CIMA, Universidad de Navarra, Pamplona, Spain
This item has received
Article information
These are the options to access the full texts of the publication Medicina Clínica (English Edition)
Subscriber
Subscribe
Purchase
Contact
Phone for subscriptions and reporting of errors
From Monday to Friday from 9 a.m. to 6 p.m. (GMT + 1) except for the months of July and August which will be from 9 a.m. to 3 p.m.
Calls from Spain
932 415 960
Calls from outside Spain
+34 932 415 960
E-mail