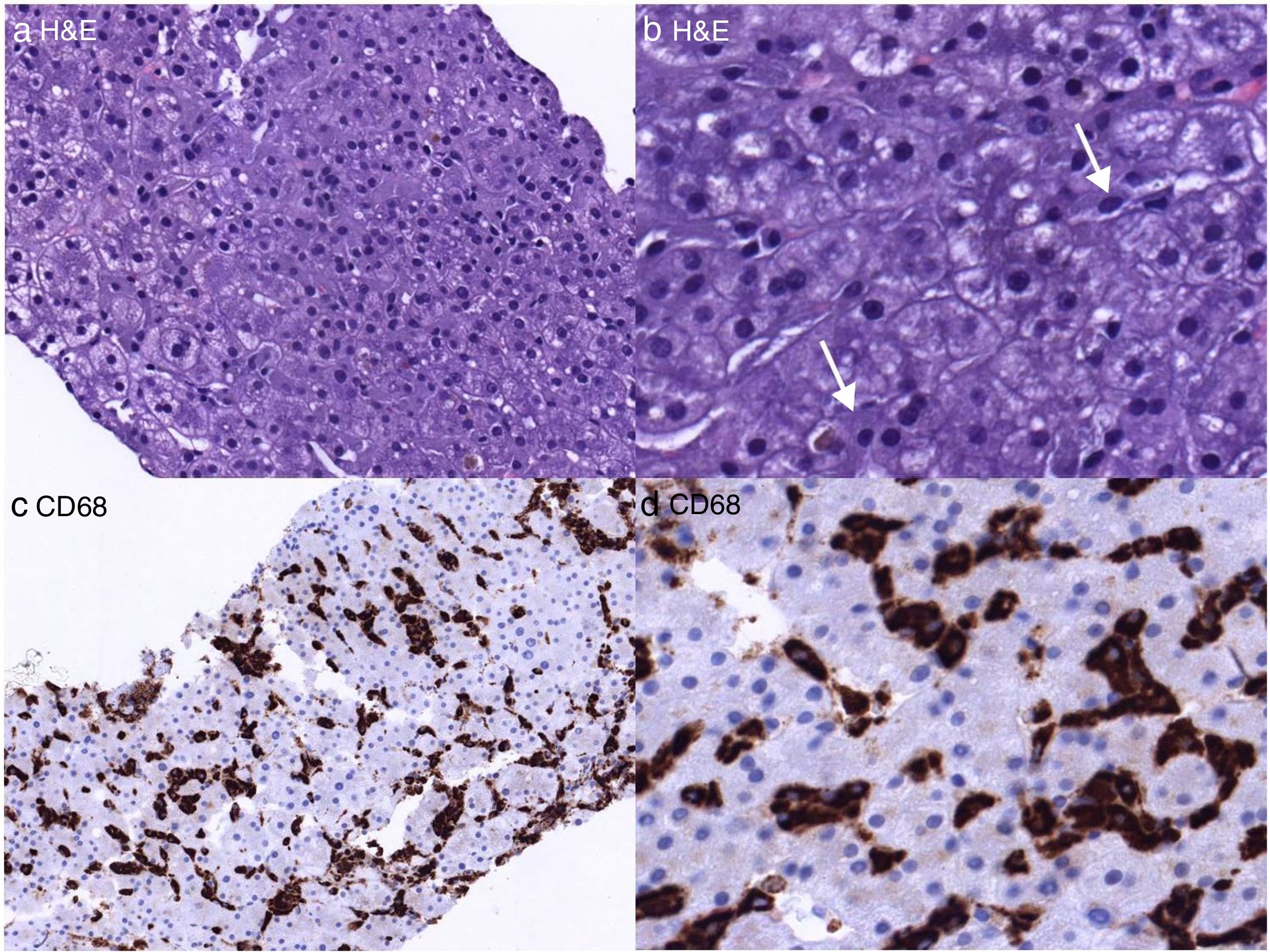
array:24 [ "pii" => "S2387020618302146" "issn" => "23870206" "doi" => "10.1016/j.medcle.2018.05.022" "estado" => "S300" "fechaPublicacion" => "2018-07-23" "aid" => "4352" "copyright" => "Elsevier España, S.L.U.. All rights reserved" "copyrightAnyo" => "2017" "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2018;151:84-5" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "Traduccion" => array:1 [ "es" => array:19 [ "pii" => "S0025775317309016" "issn" => "00257753" "doi" => "10.1016/j.medcli.2017.11.020" "estado" => "S300" "fechaPublicacion" => "2018-07-23" "aid" => "4352" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2018;151:84-5" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:2 [ "total" => 10 "formatos" => array:2 [ "HTML" => 6 "PDF" => 4 ] ] "es" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Carta al Editor</span>" "titulo" => "Síndrome de activación macrofágica inducido por administración prolongada de anfotericina-B liposomal" "tienePdf" => "es" "tieneTextoCompleto" => "es" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "84" "paginaFinal" => "85" ] ] "titulosAlternativos" => array:1 [ "en" => array:1 [ "titulo" => "Macrophage activation syndrome induced by prolonged treatment with liposomal amphotericin B" ] ] "contieneTextoCompleto" => array:1 [ "es" => true ] "contienePdf" => array:1 [ "es" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Figura 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1874 "Ancho" => 2500 "Tamanyo" => 725123 ] ] "descripcion" => array:1 [ "es" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">a y b) Tinción H&E de la biopsia hepática: a) parte del cilindro que, a menor aumento, muestra una arquitectura normal del lóbulo hepático; b) Mayor aumento de «a». Las flechas indican histiocitos con núcleos periféricos y un citoplasma elongado y granular; c y d) menor y mayor aumento de la tinción inmunohistoquímica del CD68 confirmando la presencia de abundantes histiocitos.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Gerhard Jung, Enric Reverter, Javier Fernández" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Gerhard" "apellidos" => "Jung" ] 1 => array:2 [ "nombre" => "Enric" "apellidos" => "Reverter" ] 2 => array:2 [ "nombre" => "Javier" "apellidos" => "Fernández" ] ] ] ] ] "idiomaDefecto" => "es" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S2387020618302146" "doi" => "10.1016/j.medcle.2018.05.022" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020618302146?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775317309016?idApp=UINPBA00004N" "url" => "/00257753/0000015100000002/v1_201807060854/S0025775317309016/v1_201807060854/es/main.assets" ] ] "itemSiguiente" => array:18 [ "pii" => "S2387020618302067" "issn" => "23870206" "doi" => "10.1016/j.medcle.2017.10.051" "estado" => "S300" "fechaPublicacion" => "2018-07-23" "aid" => "4362" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2018;151:85-6" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:10 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Sofosbuvir/ledipasvir as treatment of hepatitis C virus genotype 5 infection: Two case reports" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "85" "paginaFinal" => "86" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Sofosbuvir/ledipasvir para el tratamiento de la infección por genotipo 5 del virus de hepatitis C: descripción de dos casos" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Esther Chamorro-de-Vega, Alvaro Gimenez-Manzorro, Maria Sanjurjo" "autores" => array:4 [ 0 => array:2 [ "nombre" => "Esther" "apellidos" => "Chamorro-de-Vega" ] 1 => array:2 [ "nombre" => "Alvaro" "apellidos" => "Gimenez-Manzorro" ] 2 => array:2 [ "nombre" => "Maria" "apellidos" => "Sanjurjo" ] 3 => array:1 [ "colaborador" => "on behalf of the GRUVIC Study Group" ] ] ] ] ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020618302067?idApp=UINPBA00004N" "url" => "/23870206/0000015100000002/v1_201807220502/S2387020618302067/v1_201807220502/en/main.assets" ] "itemAnterior" => array:19 [ "pii" => "S2387020618302134" "issn" => "23870206" "doi" => "10.1016/j.medcle.2018.05.021" "estado" => "S300" "fechaPublicacion" => "2018-07-23" "aid" => "4317" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "crp" "cita" => "Med Clin. 2018;151:82-3" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:10 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Scientific letter</span>" "titulo" => "Analysis of severe cases of epidemic influenza and its lethality in the last 5 flu seasons" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "82" "paginaFinal" => "83" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Análisis de los casos graves de gripe epidémica y su letalidad en las últimas 5 temporadas gripales" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Jordi Reina, Carmen López de Bilbao, Melchor Riera" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Jordi" "apellidos" => "Reina" ] 1 => array:2 [ "nombre" => "Carmen" "apellidos" => "López de Bilbao" ] 2 => array:2 [ "nombre" => "Melchor" "apellidos" => "Riera" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0025775317308266" "doi" => "10.1016/j.medcli.2017.10.025" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775317308266?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020618302134?idApp=UINPBA00004N" "url" => "/23870206/0000015100000002/v1_201807220502/S2387020618302134/v1_201807220502/en/main.assets" ] "en" => array:15 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Macrophage activation syndrome induced by prolonged treatment with liposomal amphotericin B" "tieneTextoCompleto" => true "saludo" => "Dear Editor:" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "84" "paginaFinal" => "85" ] ] "autores" => array:1 [ 0 => array:4 [ "autoresLista" => "Gerhard Jung, Enric Reverter, Javier Fernández" "autores" => array:3 [ 0 => array:4 [ "nombre" => "Gerhard" "apellidos" => "Jung" "email" => array:1 [ 0 => "gerhard.jung@gmail.com" ] "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">*</span>" "identificador" => "cor0005" ] ] ] 1 => array:2 [ "nombre" => "Enric" "apellidos" => "Reverter" ] 2 => array:2 [ "nombre" => "Javier" "apellidos" => "Fernández" ] ] "afiliaciones" => array:1 [ 0 => array:2 [ "entidad" => "Unidad de Cuidados Intensivos Hepática, Hospital Clínic de Barcelona, Instituto de Enfermedades Digestivas y Metabólicas (IMDM), Barcelona, Spain" "identificador" => "aff0005" ] ] "correspondencia" => array:1 [ 0 => array:3 [ "identificador" => "cor0005" "etiqueta" => "⁎" "correspondencia" => "Corresponding author." ] ] ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Síndrome de activación macrofágica inducido por administración prolongada de anfotericina-B liposomal" ] ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1874 "Ancho" => 2500 "Tamanyo" => 725123 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">(a and b) H&E staining of liver biopsy: (a) part of the cylinder that, at lower magnification, shows a normal architecture of the hepatic lobe; (b) higher magnification of “a”. The arrows indicate histiocytes with peripheral nuclei and an elongated and granular cytoplasm; (c and d) lower and higher increase in immunohistochemical staining of CD68, confirming the presence of abundant histiocytes.</p>" ] ] ] "textoCompleto" => "<span class="elsevierStyleSections"><p id="par0005" class="elsevierStylePara elsevierViewall">The macrophage activation syndrome (MAS) is a rare entity characterized by the uncontrolled proliferation and activation of macrophages that invade other tissues such as bone marrow, liver or spleen, and can cause a variety of non-specific symptoms such as fever, cytopenia and abnormal liver function tests.<a class="elsevierStyleCrossRef" href="#bib0030"><span class="elsevierStyleSup">1</span></a> Due to the non-specificity of these symptoms, the lack of well-defined diagnostic criteria and its low prevalence, it is probably an underdiagnosed entity, although potentially severe. More and more cases are recognized in the adult population secondary to a great variety of triggers. Nevertheless, drug-induced cases are rare.</p><p id="par0010" class="elsevierStylePara elsevierViewall">We report the case of a 53-year-old male patient, admitted to the ICU and recently recovered from a multiorgan failure, who developed atypical ulcers in both lower limbs 10 days after his admission to the ICU. Skin biopsies revealed an invasive fungal infection by <span class="elsevierStyleItalic">Mucor</span>. Treatment was started with liposomal amphotericin-B (LAmB), posaconazole and anidulafungin. Surgical debridement was performed 3 times, with negative control biopsies from the second intervention. Triple antifungal therapy was maintained for a total of 61 days. After confirming the resolution of the infection, an autologous skin graft was performed, with good progression.</p><p id="par0015" class="elsevierStylePara elsevierViewall">Thirty-five days after initiating triple antifungal therapy, the patient presented with high fever refractory to antipyretics. Laboratory tests showed a normal leukocyte blood count, eosinophilia (11.5%, 600/mcl) and an abnormal liver function test (AlkP: 654<span class="elsevierStyleHsp" style=""></span>IU/l; GGT: 287<span class="elsevierStyleHsp" style=""></span>IU/l; bilirubin 2.0<span class="elsevierStyleHsp" style=""></span>mg/dl, with normal transaminases). Microbiological cultures (blood cultures, urine cultures, stool cultures, bronchoalveolar aspirates and catheters) were persistently negative. A chest-abdomen-pelvis CT scan showed moderate ascites and hepatosplenomegaly, which did not exist at the time of admission. Tumor and autoimmunity markers were also negative. Macrophages were detected in the ascitic fluid (84%/1400<span class="elsevierStyleHsp" style=""></span>cel/ml), and a massive infiltration by macrophages was observed in the pathological anatomy of the liver biopsy (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>). PET-CT showed an intense increase in bone marrow metabolism. After considering all the above, MAS was suspected. Serum ferritin and triglyceride levels were high (2184<span class="elsevierStyleHsp" style=""></span>ng/ml and 629<span class="elsevierStyleHsp" style=""></span>mg/dl, respectively), as well as the ESR (140<span class="elsevierStyleHsp" style=""></span>mm/h). Plasma fibrinogen levels were normal. With the clinical suspicion of MAS induced by the prolonged administration of LAmB (63 cumulative days of treatment) said drug was discontinued. Fever disappeared in 4 days and the ascites in 2 weeks, the liver enzymes normalized within a month and ferritin levels decreased significantly (996<span class="elsevierStyleHsp" style=""></span>mg/ml). PET performed 7 weeks after LAmB was discontinued showed a normal bone marrow metabolism.</p><elsevierMultimedia ident="fig0005"></elsevierMultimedia><p id="par0020" class="elsevierStylePara elsevierViewall">In conclusion, our patient fulfilled 4 of the 9 diagnostic criteria of the MAS, established by the “MAS study group”: fever, hyperferritinaemia, hypertriglyceridemia, abnormal liver function tests.<a class="elsevierStyleCrossRef" href="#bib0035"><span class="elsevierStyleSup">2</span></a> The presence of abundant macrophages in the liver biopsy was highly suggestive of this diagnosis. All possible secondary causes described in the literature were ruled out, these included viral infections (Epstein–Barr virus, cytomegalovirus, human herpesvirus 6, HIV-1, H1N1, hepatitis A, B virus and <span class="elsevierStyleSmallCaps">C</span>), bacterial infections (<span class="elsevierStyleItalic">Staphylococcus</span>, <span class="elsevierStyleItalic">Salmonella</span>, <span class="elsevierStyleItalic">Legionella</span>, <span class="elsevierStyleItalic">Mycoplasma</span>), neoplasms and autoimmune diseases.<a class="elsevierStyleCrossRef" href="#bib0035"><span class="elsevierStyleSup">2</span></a> The <a id="intr0010" class="elsevierStyleInterRef" href="http://www.pubmed.com/">www.pubmed.com</a> database was used for the search of cases secondary to drugs from the first description of the syndrome in 1985 to the present. Although no case of MAS induced by LAmB has been reported, it is well known that this antifungal has immunostimulant effects and is capable of increasing macrophage activity.<a class="elsevierStyleCrossRefs" href="#bib0040"><span class="elsevierStyleSup">3–5</span></a> The symptoms occurred 35 days after the start of LAmB and began to be resolved just days after its discontinuation. In addition, LAmB discontinuation was the only therapeutic measure established in the patient. The temporal relationship and the resolution of the symptoms following LAmB discontinuation supports our hypothesis that treatment with LAmB was the trigger in this case. According to the Naranjo algorithm calculation, the causal relationship between LAmB and MAS is probable (6 points). For all these reasons, MAS should be considered as a possible severe adverse reaction of prolonged treatment with LAmB. The case has been reported to the national pharmacovigilance system.</p></span>" "pdfFichero" => "main.pdf" "tienePdf" => true "NotaPie" => array:1 [ 0 => array:2 [ "etiqueta" => "☆" "nota" => "<p class="elsevierStyleNotepara" id="npar0005">Please cite this article as: Jung G, Reverter E, Fernández J. Síndrome de activación macrofágica inducido por administración prolongada de anfotericina-B liposomal. Med Clin (Barc). 2018;151:84–85.</p>" ] ] "multimedia" => array:1 [ 0 => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1874 "Ancho" => 2500 "Tamanyo" => 725123 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">(a and b) H&E staining of liver biopsy: (a) part of the cylinder that, at lower magnification, shows a normal architecture of the hepatic lobe; (b) higher magnification of “a”. The arrows indicate histiocytes with peripheral nuclei and an elongated and granular cytoplasm; (c and d) lower and higher increase in immunohistochemical staining of CD68, confirming the presence of abundant histiocytes.</p>" ] ] ] "bibliografia" => array:2 [ "titulo" => "References" "seccion" => array:1 [ 0 => array:2 [ "identificador" => "bibs0015" "bibliografiaReferencia" => array:5 [ 0 => array:3 [ "identificador" => "bib0030" "etiqueta" => "1" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Histiocytic disorders: recent insights into pathophysiology and practical guidelines" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "A. Filipovich" 1 => "K. McClain" 2 => "A. Grom" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.bbmt.2009.11.014" "Revista" => array:7 [ "tituloSerie" => "Biol Blood Marrow Transplant" "fecha" => "2010" "volumen" => "16" "numero" => "Suppl 1" "paginaInicial" => "S82" "paginaFinal" => "S89" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/19932759" "web" => "Medline" ] ] ] ] ] ] ] ] 1 => array:3 [ "identificador" => "bib0035" "etiqueta" => "2" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Clinical features and correct diagnosis of macrophage activation syndrome" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "R.Q. Cron" 1 => "S. Davi" 2 => "F. Minoia" 3 => "A. Ravelli" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1586/1744666X.2015.1058159" "Revista" => array:6 [ "tituloSerie" => "Expert Rev Clin Immunol" "fecha" => "2015" "volumen" => "11" "paginaInicial" => "1043" "paginaFinal" => "1053" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/26082353" "web" => "Medline" ] ] ] ] ] ] ] ] 2 => array:3 [ "identificador" => "bib0040" "etiqueta" => "3" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Effects of amphotericin B on macrophages and their precursor cells" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "S.H. Lin" 1 => "G. Medoff" 2 => "G.S. Kobayashi" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "Antimicrob Agents Chemother" "fecha" => "1977" "volumen" => "11" "paginaInicial" => "154" "paginaFinal" => "160" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/836011" "web" => "Medline" ] ] ] ] ] ] ] ] 3 => array:3 [ "identificador" => "bib0045" "etiqueta" => "4" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Amphotericin B stimulates γδ T and NK cells, and enhances protection from Salmonella infection" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "J.F. Hedges" 1 => "A.M. Mitchell" 2 => "K. Jones" 3 => "E. Kimmel" 4 => "A.G. Ramstead" 5 => "D.T. Snyder" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1177/1753425914567692" "Revista" => array:6 [ "tituloSerie" => "Innate Immun" "fecha" => "2015" "volumen" => "21" "paginaInicial" => "598" "paginaFinal" => "608" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/25608515" "web" => "Medline" ] ] ] ] ] ] ] ] 4 => array:3 [ "identificador" => "bib0050" "etiqueta" => "5" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Therapeutic and immunomodulatory activities of short-course treatment of murine visceral leishmaniasis with KALSOME10, a new liposomal amphotericin B" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "M. Asad" 1 => "P. Bhattacharya" 2 => "A. Banerjee" 3 => "N. Ali" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1186/s12879-015-0928-6" "Revista" => array:5 [ "tituloSerie" => "BMC Infect Dis" "fecha" => "2015" "volumen" => "15" "paginaInicial" => "188" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/25884796" "web" => "Medline" ] ] ] ] ] ] ] ] ] ] ] ] ] "idiomaDefecto" => "en" "url" => "/23870206/0000015100000002/v1_201807220502/S2387020618302146/v1_201807220502/en/main.assets" "Apartado" => array:4 [ "identificador" => "43309" "tipo" => "SECCION" "en" => array:2 [ "titulo" => "Letters to the Editor" "idiomaDefecto" => true ] "idiomaDefecto" => "en" ] "PDF" => "https://static.elsevier.es/multimedia/23870206/0000015100000002/v1_201807220502/S2387020618302146/v1_201807220502/en/main.pdf?idApp=UINPBA00004N&text.app=https://www.elsevier.es/" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020618302146?idApp=UINPBA00004N" ]
Journal Information
Vol. 151. Issue 2.
Pages 84-85 (July 2018)
Share
Download PDF
More article options
Vol. 151. Issue 2.
Pages 84-85 (July 2018)
Letter to the Editor
Macrophage activation syndrome induced by prolonged treatment with liposomal amphotericin B
Síndrome de activación macrofágica inducido por administración prolongada de anfotericina-B liposomal
Visits
3
Gerhard Jung
, Enric Reverter, Javier Fernández
Corresponding author
Unidad de Cuidados Intensivos Hepática, Hospital Clínic de Barcelona, Instituto de Enfermedades Digestivas y Metabólicas (IMDM), Barcelona, Spain
This item has received
Article information
These are the options to access the full texts of the publication Medicina Clínica (English Edition)
Subscriber
Subscribe
Purchase
Contact
Phone for subscriptions and reporting of errors
From Monday to Friday from 9 a.m. to 6 p.m. (GMT + 1) except for the months of July and August which will be from 9 a.m. to 3 p.m.
Calls from Spain
932 415 960
Calls from outside Spain
+34 932 415 960
E-mail