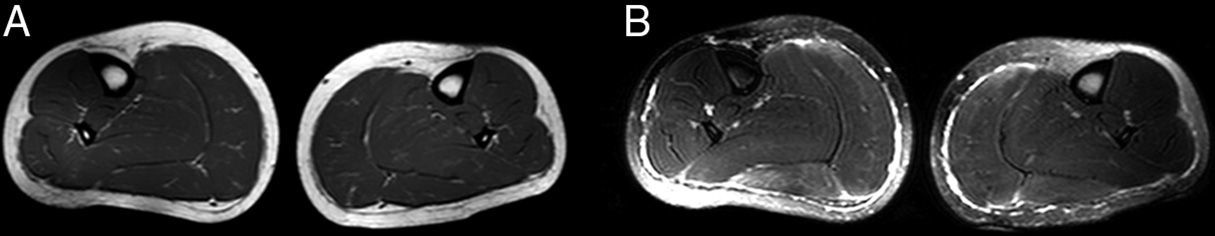
array:24 [ "pii" => "S2387020616001844" "issn" => "23870206" "doi" => "10.1016/j.medcle.2016.03.008" "estado" => "S300" "fechaPublicacion" => "2015-11-06" "aid" => "3201" "copyright" => "Elsevier España, S.L.U.. All rights reserved" "copyrightAnyo" => "2015" "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2015;145:413-4" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "Traduccion" => array:1 [ "es" => array:19 [ "pii" => "S0025775314008902" "issn" => "00257753" "doi" => "10.1016/j.medcli.2014.12.010" "estado" => "S300" "fechaPublicacion" => "2015-11-06" "aid" => "3201" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2015;145:413-4" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:2 [ "total" => 19 "formatos" => array:2 [ "HTML" => 8 "PDF" => 11 ] ] "es" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Carta al Editor</span>" "titulo" => "Afectación muscular en la anemia drepanocítica" "tienePdf" => "es" "tieneTextoCompleto" => "es" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "413" "paginaFinal" => "414" ] ] "titulosAlternativos" => array:1 [ "en" => array:1 [ "titulo" => "Muscle involvement in sickle cell disease" ] ] "contieneTextoCompleto" => array:1 [ "es" => true ] "contienePdf" => array:1 [ "es" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Figura 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 396 "Ancho" => 2028 "Tamanyo" => 82835 ] ] "descripcion" => array:1 [ "es" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Resonancia magnética de pierna. A. Secuencia T1 que muestra una hipertrofia de <span class="elsevierStyleItalic">tibialis anterior, peroneus longus, gastrocnemius</span> y <span class="elsevierStyleItalic">soleus</span>. B. Secuencia SPIR donde aparece una hiperintensidad en la fascia muscular de los compartimentos posterior y anterolateral.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Miguel Ángel Rubio, Laura Díez, Nuria Álvarez, Elvira Munteis" "autores" => array:4 [ 0 => array:2 [ "nombre" => "Miguel Ángel" "apellidos" => "Rubio" ] 1 => array:2 [ "nombre" => "Laura" "apellidos" => "Díez" ] 2 => array:2 [ "nombre" => "Nuria" "apellidos" => "Álvarez" ] 3 => array:2 [ "nombre" => "Elvira" "apellidos" => "Munteis" ] ] ] ] ] "idiomaDefecto" => "es" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S2387020616001844" "doi" => "10.1016/j.medcle.2016.03.008" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020616001844?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775314008902?idApp=UINPBA00004N" "url" => "/00257753/0000014500000009/v1_201510150221/S0025775314008902/v1_201510150221/es/main.assets" ] ] "itemSiguiente" => array:19 [ "pii" => "S2387020616001856" "issn" => "23870206" "doi" => "10.1016/j.medcle.2016.03.009" "estado" => "S300" "fechaPublicacion" => "2015-11-06" "aid" => "3200" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2015;145:414-5" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Dysferlinopathy masquerading as a refractory polymyositis" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "414" "paginaFinal" => "415" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Disferlinopatía, una causa de falsa polimiositis refractaria" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 988 "Ancho" => 1216 "Tamanyo" => 73762 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Western-blot dysferlin in monocytes. P1 (patient reported): 18% dysferlin expression. P2 (myopathy control): 82% dysferlin expression (normal). C: healthy control.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Jose Loureiro Amigo, Eduard Gallardo, Pia Gallano, Josep M. Grau-Junyent" "autores" => array:4 [ 0 => array:2 [ "nombre" => "Jose" "apellidos" => "Loureiro Amigo" ] 1 => array:2 [ "nombre" => "Eduard" "apellidos" => "Gallardo" ] 2 => array:2 [ "nombre" => "Pia" "apellidos" => "Gallano" ] 3 => array:2 [ "nombre" => "Josep M." "apellidos" => "Grau-Junyent" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0025775314008896" "doi" => "10.1016/j.medcli.2014.12.009" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775314008896?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020616001856?idApp=UINPBA00004N" "url" => "/23870206/0000014500000009/v2_201605020201/S2387020616001856/v2_201605020201/en/main.assets" ] "itemAnterior" => array:19 [ "pii" => "S2387020616001832" "issn" => "23870206" "doi" => "10.1016/j.medcle.2016.03.007" "estado" => "S300" "fechaPublicacion" => "2015-11-06" "aid" => "3230" "copyright" => "Elsevier España, S.L.U." "documento" => "article" "crossmark" => 1 "subdocumento" => "sco" "cita" => "Med Clin. 2015;145:409-12" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:10 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Special article</span>" "titulo" => "Total knee prosthesis. Development of an objective selection tool for patients" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "409" "paginaFinal" => "412" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Elaboración de un índice objetivo de selección de pacientes subsidiarios de prótesis articular de rodilla" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Tomás Alcántara-Martos, Juan Carlos Rodríguez-Fernández, Antonio Evaristo Resola-García, Alberto Damián Delgado-Martínez" "autores" => array:4 [ 0 => array:2 [ "nombre" => "Tomás" "apellidos" => "Alcántara-Martos" ] 1 => array:2 [ "nombre" => "Juan Carlos" "apellidos" => "Rodríguez-Fernández" ] 2 => array:2 [ "nombre" => "Antonio Evaristo" "apellidos" => "Resola-García" ] 3 => array:2 [ "nombre" => "Alberto Damián" "apellidos" => "Delgado-Martínez" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S002577531500069X" "doi" => "10.1016/j.medcli.2015.01.012" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S002577531500069X?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020616001832?idApp=UINPBA00004N" "url" => "/23870206/0000014500000009/v2_201605020201/S2387020616001832/v2_201605020201/en/main.assets" ] "en" => array:16 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Muscle involvement in sickle cell disease" "tieneTextoCompleto" => true "saludo" => "Dear Editor," "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "413" "paginaFinal" => "414" ] ] "autores" => array:1 [ 0 => array:4 [ "autoresLista" => "Miguel Ángel Rubio, Laura Díez, Nuria Álvarez, Elvira Munteis" "autores" => array:4 [ 0 => array:4 [ "nombre" => "Miguel Ángel" "apellidos" => "Rubio" "email" => array:1 [ 0 => "97495@parcdesalutmar.cat" ] "referencia" => array:2 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">a</span>" "identificador" => "aff0005" ] 1 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">*</span>" "identificador" => "cor0005" ] ] ] 1 => array:3 [ "nombre" => "Laura" "apellidos" => "Díez" "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">a</span>" "identificador" => "aff0005" ] ] ] 2 => array:3 [ "nombre" => "Nuria" "apellidos" => "Álvarez" "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">b</span>" "identificador" => "aff0010" ] ] ] 3 => array:3 [ "nombre" => "Elvira" "apellidos" => "Munteis" "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">a</span>" "identificador" => "aff0005" ] ] ] ] "afiliaciones" => array:2 [ 0 => array:3 [ "entidad" => "Unidad de Enfermedades Neuromusculares, Servicio de Neurología, Hospital del Mar, Barcelona, Spain" "etiqueta" => "a" "identificador" => "aff0005" ] 1 => array:3 [ "entidad" => "Sección de Neurofisiología, Servicio de Neurología, Hospital del Mar, Barcelona, Spain" "etiqueta" => "b" "identificador" => "aff0010" ] ] "correspondencia" => array:1 [ 0 => array:3 [ "identificador" => "cor0005" "etiqueta" => "⁎" "correspondencia" => "Corresponding author." ] ] ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Afectación muscular en la anemia drepanocítica" ] ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 236 "Ancho" => 1215 "Tamanyo" => 46558 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">MRI of leg. (A) T1 sequence showing hypertrophy of tibialis anterior, peroneus longus, gastrocnemius and soleus. (B) SPIR sequence where hyperintensity appears in the fascia of the posterior, anterior and lateral compartments.</p>" ] ] ] "textoCompleto" => "<span class="elsevierStyleSections"><p id="par0005" class="elsevierStylePara elsevierViewall">Sickle cell disease, also called sickle cell anemia is a genetic disease characterized by a homozygous mutation in the gene encoding the beta chain of adult hemoglobin (Hb A). The result is an abnormal hemoglobin, hemoglobin S (Hb S). The deoxygenated form of Hb S has a lower solubility and tends to polymerize, leading to the characteristic symptoms of the disease: haemolytic anemia and vaso-occlusive crises. These episodes of vascular occlusion cause acute or chronic pain in thorax, abdomen, back and limbs, and more rarely inflammation, necrosis and fibrosis of the muscles of the lower limbs and adjacent soft tissues.<a class="elsevierStyleCrossRef" href="#bib0045"><span class="elsevierStyleSup">1</span></a> Patients with sickle cell trait or carrier status, have heterozygous mutation, with varying degrees of co-existence of abnormal hemoglobin (Hb S) and normal adult hemoglobin (Hb A). Although the carrier status is considered a benign condition, in recent years, complications of sickle cell disease have also been reported in heterozygous carriers.<a class="elsevierStyleCrossRefs" href="#bib0050"><span class="elsevierStyleSup">2,3</span></a></p><p id="par0010" class="elsevierStylePara elsevierViewall">We report the case of a 33-year-old heterozygous carrier of Hb S (Hb S 35%) with a history of pulmonary embolism at age 21, taking oral contraceptives for the treatment of ovarian polycystic syndrome. The patient was referred for evaluation for a 3-month pain in both lower limbs, in the posterior, anterior and lateral compartment of legs. Pain began acutely, and patient described it as continuous but with intensity fluctuations throughout the day, with difficult ambulation. There was not a pain trigger such as physical exercise, dehydration, or changes in medication. Physical examination showed muscle hypertrophy of both calfs (or tibialis anterior), without the presence of signs of inflammation, edema or a motor sensory disorder. The bone-tendon reflexes were preserved. The blood cell count showed hemoglobin levels of 14.1<span class="elsevierStyleHsp" style=""></span>g/dl (11.7–15.5<span class="elsevierStyleHsp" style=""></span>g/dl), mean corpuscular volume 77<span class="elsevierStyleHsp" style=""></span>fl (82–99<span class="elsevierStyleHsp" style=""></span>fl), mean corpuscular hemoglobin 26.1<span class="elsevierStyleHsp" style=""></span><span class="elsevierStyleHsp" style=""></span>pg (27–34<span class="elsevierStyleHsp" style=""></span>pg), and 1.4% reticulocytes (0.5–1.5%). Serum CK levels were normal (178<span class="elsevierStyleHsp" style=""></span>IU/l [38–176<span class="elsevierStyleHsp" style=""></span>IU/l]). A study was conducted to rule out peripheral vascular disease, without pathological findings. Given the existence of muscle hypertrophy, the patient underwent magnetic resonance imaging (MRI) of the lower limbs. It was identified a symmetrical increase in the muscle volume of gastrocnemius, soleus, tibialis anterior and peroneus longus. Furthermore, the SPIR sequences, a sequence of fat suppression and T2 showed bilateral hyperintensity consistent with perifascial edema located on the surface of all muscles listed above (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>). There were no signal changes in the muscles, indicating the absence of edema and fatty infiltration. Both, bone and bone marrow signals were preserved.</p><elsevierMultimedia ident="fig0005"></elsevierMultimedia><p id="par0015" class="elsevierStylePara elsevierViewall">While myositis and fasciitis have been reported in patients with sickle cell disease,<a class="elsevierStyleCrossRef" href="#bib0060"><span class="elsevierStyleSup">4</span></a> they represent a very rare complication, especially in a carrier status. The presence of a perifascial hyperintensity on MRI has been found in all reported cases of sickle cell disease and fascitis.<a class="elsevierStyleCrossRef" href="#bib0065"><span class="elsevierStyleSup">5</span></a> Muscle hypertrophy, although it is a nonspecific feature, has also been reported in sickle cell disease.</p><p id="par0020" class="elsevierStylePara elsevierViewall">In this case, the symptoms were nonspecific, and after an initial inconclusive etiologic study, muscle MRI findings were key to the diagnosis. Although these radiological findings were subtle, they led to the diagnosis of fasciitis with global preservation of muscle tissue. In both, cases of sickle cell disease or sickle cell trait, the presence of fascial edema is considered secondary to progression of histological changes in inflammation and muscle necrosis.<a class="elsevierStyleCrossRef" href="#bib0070"><span class="elsevierStyleSup">6</span></a> In addition, rhabdomyolysis has also been reported after physical exercise in patients with sickle cell trait.<a class="elsevierStyleCrossRef" href="#bib0075"><span class="elsevierStyleSup">7</span></a> In experimental studies, muscle hypertrophy has been shown to occur as a response secondary to chronic blood flow restriction to muscles.<a class="elsevierStyleCrossRef" href="#bib0080"><span class="elsevierStyleSup">8</span></a> In our patient, the absence of signal abnormalities in muscle tissue on MRI, CK levels within the normal range, as well as the absence of a pain trigger, might imply that the perifascial edema was secondary to mild and incipient inflammatory changes in muscle and in the surrounding soft tissues.</p><p id="par0025" class="elsevierStylePara elsevierViewall">This case is focused, on the one hand, on the value of muscle RMI as a sensitive non-invasive method for reporting early and subtle changes in soft tissues, and also makes us remember that patients with sickle cell trait may have similar complications to those of homozygous mutation carriers.</p><span id="sec0005" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0005">Conflicts of interest</span><p id="par0030" class="elsevierStylePara elsevierViewall">The authors report no conflicts of interest.</p></span></span>" "textoCompletoSecciones" => array:1 [ "secciones" => array:2 [ 0 => array:2 [ "identificador" => "sec0005" "titulo" => "Conflicts of interest" ] 1 => array:1 [ "titulo" => "References" ] ] ] "pdfFichero" => "main.pdf" "tienePdf" => true "NotaPie" => array:1 [ 0 => array:2 [ "etiqueta" => "☆" "nota" => "<p class="elsevierStyleNotepara" id="npar0005">Please cite this article as: Rubio MÁ, Díez L, Álvarez N, Munteis E. Afectación muscular en la anemia drepanocítica. Med Clin (Barc). 2015;145:413–414.</p>" ] ] "multimedia" => array:1 [ 0 => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 236 "Ancho" => 1215 "Tamanyo" => 46558 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">MRI of leg. (A) T1 sequence showing hypertrophy of tibialis anterior, peroneus longus, gastrocnemius and soleus. (B) SPIR sequence where hyperintensity appears in the fascia of the posterior, anterior and lateral compartments.</p>" ] ] ] "bibliografia" => array:2 [ "titulo" => "References" "seccion" => array:1 [ 0 => array:2 [ "identificador" => "bibs0005" "bibliografiaReferencia" => array:8 [ 0 => array:3 [ "identificador" => "bib0045" "etiqueta" => "1" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "MRI of soft tissue abnormalities: a primary cause of sickle cell crisis" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "F. Feldman" 1 => "A. Zwass" 2 => "R.B. Staron" 3 => "N. Haramati" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "Skeletal Radiol" "fecha" => "1993" "volumen" => "22" "paginaInicial" => "501" "paginaFinal" => "506" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/8272885" "web" => "Medline" ] ] ] ] ] ] ] ] 1 => array:3 [ "identificador" => "bib0050" "etiqueta" => "2" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Sickle-cell trait: novel clinical significance" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "N.S. Key" 1 => "V.K. Derebail" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Hematol Am Soc Hematol Educ Prog" "fecha" => "2010" "volumen" => "2010" "paginaInicial" => "418" "paginaFinal" => "422" ] ] ] ] ] ] 2 => array:3 [ "identificador" => "bib0055" "etiqueta" => "3" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Complications associated with sickle cell trait: a brief narrative review" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "G. Tsaras" 1 => "A. Owusu-Ansah" 2 => "F.O. Boateng" 3 => "Y. Amoateng-Adjepong" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.amjmed.2008.12.020" "Revista" => array:6 [ "tituloSerie" => "Am J Med" "fecha" => "2009" "volumen" => "122" "paginaInicial" => "507" "paginaFinal" => "512" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/19393983" "web" => "Medline" ] ] ] ] ] ] ] ] 3 => array:3 [ "identificador" => "bib0060" "etiqueta" => "4" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Acute muscle injury complicating sickle cell crisis" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "H.R. Schumacher" 1 => "W.M. Murray" 2 => "M.K. Dalinka" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "Semin Arthritis Rheum" "fecha" => "1990" "volumen" => "19" "paginaInicial" => "243" "paginaFinal" => "247" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/2321031" "web" => "Medline" ] ] ] ] ] ] ] ] 4 => array:3 [ "identificador" => "bib0065" "etiqueta" => "5" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Musculoskeletal manifestations of sickle cell disease" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:5 [ 0 => "V.C. Ejindu" 1 => "A.L. Hine" 2 => "M. Mashayekhi" 3 => "P.J. Shorvon" 4 => "R.R. Misra" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1148/rg.274065142" "Revista" => array:6 [ "tituloSerie" => "Radiographics" "fecha" => "2007" "volumen" => "27" "paginaInicial" => "1005" "paginaFinal" => "1021" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/17620464" "web" => "Medline" ] ] ] ] ] ] ] ] 5 => array:3 [ "identificador" => "bib0070" "etiqueta" => "6" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Myonecrosis in sickle cell anemia: case report and review of the literature" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "P. Vicari" 1 => "R. Achkar" 2 => "K.R. Oliveira" 3 => "M.L. Miszpupten" 4 => "A.R.C. Fernandes" 5 => "M.S. Figuereido" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1097/01.SMJ.0000125172.95454.B7" "Revista" => array:6 [ "tituloSerie" => "South Med J" "fecha" => "2004" "volumen" => "97" "paginaInicial" => "894" "paginaFinal" => "896" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/15455982" "web" => "Medline" ] ] ] ] ] ] ] ] 6 => array:3 [ "identificador" => "bib0075" "etiqueta" => "7" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Exertional rhabdomyolysis and renal failure in patients with sickle cell trait: is it time to change our approach?" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "J.N. Makaryus" 1 => "J.N. Catanzaro" 2 => "K.C. Katona" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1080/10245330701255254" "Revista" => array:6 [ "tituloSerie" => "Hematology" "fecha" => "2007" "volumen" => "12" "paginaInicial" => "349" "paginaFinal" => "352" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/17654064" "web" => "Medline" ] ] ] ] ] ] ] ] 7 => array:3 [ "identificador" => "bib0080" "etiqueta" => "8" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Effects of blood flow restricted low-intensity concentric or eccentric training on muscle size and strength" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "T. Yasuda" 1 => "J.P. Loenneke" 2 => "R.S. Thiebayd" 3 => "T. Abe" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1371/journal.pone.0052843" "Revista" => array:5 [ "tituloSerie" => "PLoS ONE" "fecha" => "2012" "volumen" => "7" "paginaInicial" => "e52843" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/23300795" "web" => "Medline" ] ] ] ] ] ] ] ] ] ] ] ] ] "idiomaDefecto" => "en" "url" => "/23870206/0000014500000009/v2_201605020201/S2387020616001844/v2_201605020201/en/main.assets" "Apartado" => array:4 [ "identificador" => "43309" "tipo" => "SECCION" "en" => array:2 [ "titulo" => "Letters to the Editor" "idiomaDefecto" => true ] "idiomaDefecto" => "en" ] "PDF" => "https://static.elsevier.es/multimedia/23870206/0000014500000009/v2_201605020201/S2387020616001844/v2_201605020201/en/main.pdf?idApp=UINPBA00004N&text.app=https://www.elsevier.es/" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020616001844?idApp=UINPBA00004N" ]
Journal Information
Vol. 145. Issue 9.
Pages 413-414 (November 2015)
Share
Download PDF
More article options
Vol. 145. Issue 9.
Pages 413-414 (November 2015)
Letter to the Editor
Muscle involvement in sickle cell disease
Afectación muscular en la anemia drepanocítica
Visits
1
This item has received
Article information
These are the options to access the full texts of the publication Medicina Clínica (English Edition)
Subscriber
Subscribe
Purchase
Contact
Phone for subscriptions and reporting of errors
From Monday to Friday from 9 a.m. to 6 p.m. (GMT + 1) except for the months of July and August which will be from 9 a.m. to 3 p.m.
Calls from Spain
932 415 960
Calls from outside Spain
+34 932 415 960
E-mail