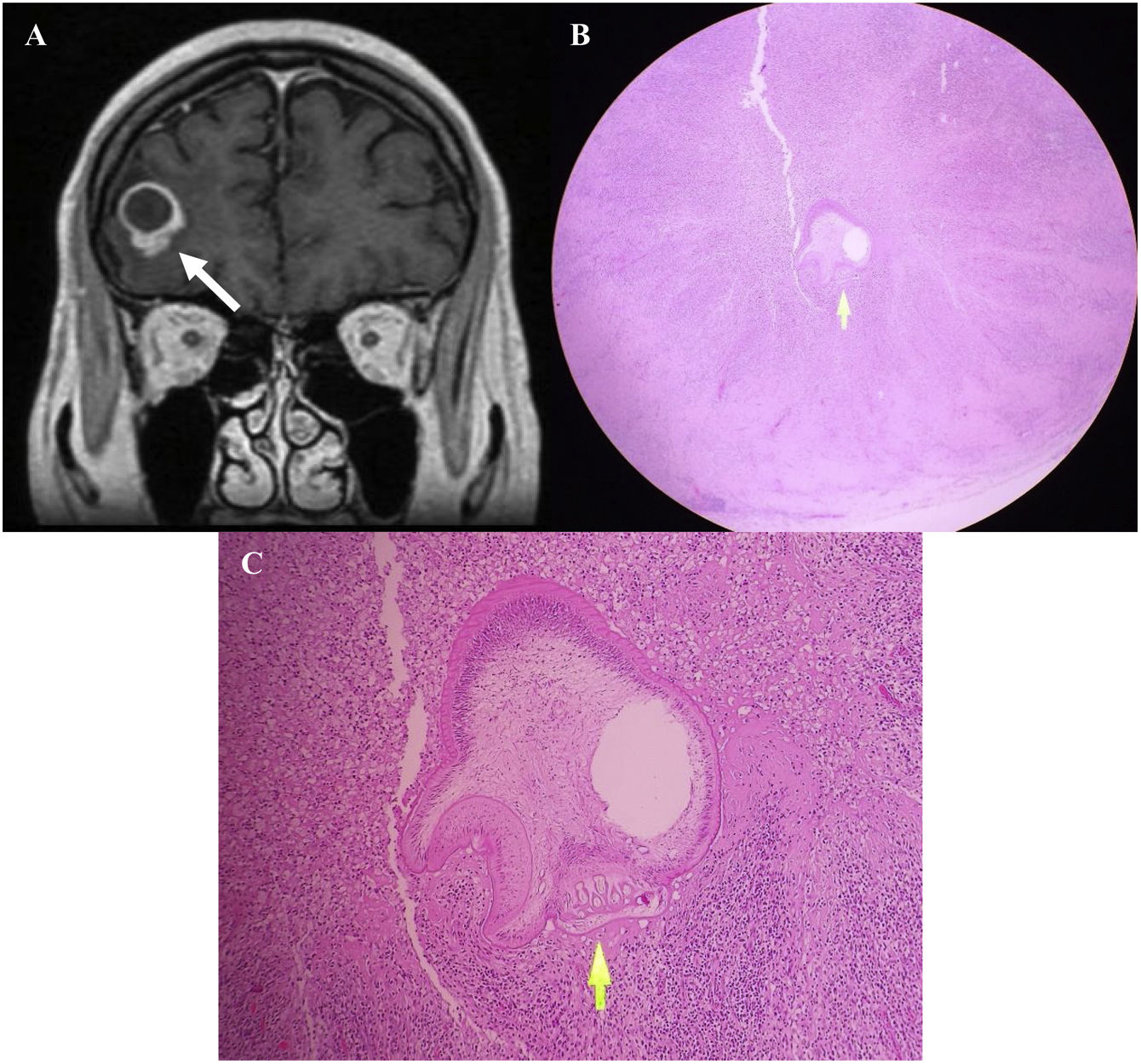
array:24 [ "pii" => "S2387020623003170" "issn" => "23870206" "doi" => "10.1016/j.medcle.2023.04.020" "estado" => "S300" "fechaPublicacion" => "2023-08-25" "aid" => "6269" "copyright" => "Elsevier España, S.L.U.. All rights reserved" "copyrightAnyo" => "2023" "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2023;161:177-8" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "Traduccion" => array:1 [ "es" => array:19 [ "pii" => "S0025775323002312" "issn" => "00257753" "doi" => "10.1016/j.medcli.2023.04.014" "estado" => "S300" "fechaPublicacion" => "2023-08-25" "aid" => "6269" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2023;161:177-8" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "es" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Carta al Editor</span>" "titulo" => "Neurocisticercosis: causa infrecuente de granuloma cerebral único" "tienePdf" => "es" "tieneTextoCompleto" => "es" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "177" "paginaFinal" => "178" ] ] "titulosAlternativos" => array:1 [ "en" => array:1 [ "titulo" => "Neurocysticercosis: A rare cause of a single brain granuloma" ] ] "contieneTextoCompleto" => array:1 [ "es" => true ] "contienePdf" => array:1 [ "es" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Figura 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1250 "Ancho" => 1340 "Tamanyo" => 297932 ] ] "descripcion" => array:1 [ "es" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">A<span class="elsevierStyleBold">.</span> Resonancia magética cerebral contrastada en corte coronal en secuencia T1 que evidencia una lesión quística que capta contraste en su periferia, teniendo un aparente nódulo en su parte inferomedial, con aparente necrosis central (flecha). B<span class="elsevierStyleBold">.</span> Presencia de severo infiltrado linfohistiocitario y abundantes macrófagos, y a nivel central se observa el corte transversal de una larva con invaginaciones de su pared (flecha). Hematoxilina-eosina 4×. C<span class="elsevierStyleBold">.</span> Corte transversal de larva de cisticerco al nivel del escólex, donde se observa el tegumento ondulado y con microvellosidades, además de la presencia de los ganchos (flecha). Hematoxilina-eosina 40×.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "John Vargas-Urbina, Raúl Martinez- Silva, William Anicama-Lima" "autores" => array:3 [ 0 => array:2 [ "nombre" => "John" "apellidos" => "Vargas-Urbina" ] 1 => array:2 [ "nombre" => "Raúl" "apellidos" => "Martinez- Silva" ] 2 => array:2 [ "nombre" => "William" "apellidos" => "Anicama-Lima" ] ] ] ] ] "idiomaDefecto" => "es" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S2387020623003170" "doi" => "10.1016/j.medcle.2023.04.020" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020623003170?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775323002312?idApp=UINPBA00004N" "url" => "/00257753/0000016100000004/v1_202308141143/S0025775323002312/v1_202308141143/es/main.assets" ] ] "itemSiguiente" => array:19 [ "pii" => "S2387020623003182" "issn" => "23870206" "doi" => "10.1016/j.medcle.2023.07.003" "estado" => "S300" "fechaPublicacion" => "2023-08-25" "aid" => "6270" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2023;161:178-9" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Use of continuous venovenous hemodiafiltration in a case of severe pentobarbital poisoning" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "178" "paginaFinal" => "179" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Uso de hemodiafiltración venovenosa continua en un caso de intoxicación grave por pentobarbital" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:8 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1004 "Ancho" => 1675 "Tamanyo" => 107034 ] ] "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at0170" "detalle" => "Fig. " "rol" => "short" ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Monitoring of pentobarbital level in serum and dialysate effluent during continuous venovenous haemodiafiltration treatment.</p> <p id="spar0010" class="elsevierStyleSimplePara elsevierViewall">L.C.: lethal concentration; T.C.: therapeutic concentration; CVVHDF: continuous venovenous haemodiafiltration.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Yasmina Nieto Piñar, Maria Sala Carazo, Bernardino Barceló Martín" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Yasmina" "apellidos" => "Nieto Piñar" ] 1 => array:2 [ "nombre" => "Maria" "apellidos" => "Sala Carazo" ] 2 => array:2 [ "nombre" => "Bernardino" "apellidos" => "Barceló Martín" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0025775323002300" "doi" => "10.1016/j.medcli.2023.04.015" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775323002300?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020623003182?idApp=UINPBA00004N" "url" => "/23870206/0000016100000004/v1_202308280911/S2387020623003182/v1_202308280911/en/main.assets" ] "itemAnterior" => array:19 [ "pii" => "S2387020623003145" "issn" => "23870206" "doi" => "10.1016/j.medcle.2023.04.018" "estado" => "S300" "fechaPublicacion" => "2023-08-25" "aid" => "6267" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2023;161:176-7" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:10 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "A new mutation associated with severe factor XI deficiency" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "176" "paginaFinal" => "177" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Una nueva mutación asociada con déficit grave de factor XI" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Irene Payá, Silvina Judith Rios, Amparo Santamaría" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Irene" "apellidos" => "Payá" ] 1 => array:2 [ "nombre" => "Silvina Judith" "apellidos" => "Rios" ] 2 => array:2 [ "nombre" => "Amparo" "apellidos" => "Santamaría" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0025775323002282" "doi" => "10.1016/j.medcli.2023.04.012" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775323002282?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020623003145?idApp=UINPBA00004N" "url" => "/23870206/0000016100000004/v1_202308280911/S2387020623003145/v1_202308280911/en/main.assets" ] "en" => array:15 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Neurocysticercosis: A rare cause of a single brain granuloma" "tieneTextoCompleto" => true "saludo" => "<span class="elsevierStyleItalic">Dear Editor,</span>" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "177" "paginaFinal" => "178" ] ] "autores" => array:1 [ 0 => array:4 [ "autoresLista" => "John Vargas-Urbina, Raúl Martinez-Silva, William Anicama-Lima" "autores" => array:3 [ 0 => array:4 [ "nombre" => "John" "apellidos" => "Vargas-Urbina" "email" => array:1 [ 0 => "johnkilin27@hotmail.com" ] "referencia" => array:2 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">a</span>" "identificador" => "aff0005" ] 1 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">*</span>" "identificador" => "cor0005" ] ] ] 1 => array:3 [ "nombre" => "Raúl" "apellidos" => "Martinez-Silva" "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">a</span>" "identificador" => "aff0005" ] ] ] 2 => array:3 [ "nombre" => "William" "apellidos" => "Anicama-Lima" "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">b</span>" "identificador" => "aff0010" ] ] ] ] "afiliaciones" => array:2 [ 0 => array:3 [ "entidad" => "Servicio de Neurocirugía Vascular, Tumores y Funcional, Departamento de Neurocirugía, Hospital Nacional Guillermo Almenara Irigoyen, Lima, Peru" "etiqueta" => "a" "identificador" => "aff0005" ] 1 => array:3 [ "entidad" => "Servicio de Anatomía Patológica, Hospital Nacional Guillermo Almenara Irigoyen, Lima, Peru" "etiqueta" => "b" "identificador" => "aff0010" ] ] "correspondencia" => array:1 [ 0 => array:3 [ "identificador" => "cor0005" "etiqueta" => "⁎" "correspondencia" => "Corresponding author." ] ] ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Neurocisticercosis: causa infrecuente de granuloma cerebral único" ] ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:8 [ "identificador" => "fig0005" "etiqueta" => "Figure 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1250 "Ancho" => 1340 "Tamanyo" => 298298 ] ] "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at0005" "detalle" => "Figure " "rol" => "short" ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">A. Coronal T1-weighted contrast-enhanced brain magnetic resonance showing a cystic lesion with contrast enhancement in its periphery, with an apparent nodule in its inferomedial part, with apparent central necrosis (arrow). B. Presence of severe lymphohistiocytic infiltrate and abundant macrophages, and centrally, a cross section of a larva with invaginations of its wall (arrow). Haematoxylin-eosin 4×. C. Cross section of cysticercus larva at the level of the scolex, showing the wavy tegument with microvilli and the presence of the hooks (arrow). Haematoxylin-eosin 40×.</p>" ] ] ] "textoCompleto" => "<span class="elsevierStyleSections"><p id="par0005" class="elsevierStylePara elsevierViewall">Neurocysticercosis (NCC) usually involves the cerebral hemispheres, with lesions found at the grey and white matter junction. It can be associated with several imaging findings, including a single enhancing lesion, which creates a medical dilemma due to a high rate of negative serological studies.<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a> Specific 3D and FLAIR MRI allows us to better visualise the cyst wall and the scolex.<a class="elsevierStyleCrossRef" href="#bib0010"><span class="elsevierStyleSup">2</span></a></p><p id="par0010" class="elsevierStylePara elsevierViewall">Therefore, we report an illustrative case of a 41-year-old male patient with no medical or surgical history. The clinical manifestations began a year before, with a generalised tonic-clonic seizure. A contrast-enhanced brain magnetic resonance imaging (MRI) was performed, which showed an irregular right frontobasal expansive process, with ring-like contrast enhancement, which did not restrict diffusion and which showed a lipid-lactate peak in the spectroscopy. The cerebrospinal fluid (CSF) study was normal. Based on the clinical/radiological characteristics, the presumptive diagnosis was bacterial abscess, and empirical treatment was started for 21 days with meropenem plus vancomycin, with no lesion resolution, so anti-tuberculosis treatment was initiated. The patient developed an adverse drug reaction (Dress's syndrome) in the second week, so drugs were discontinued. After improvement, the patient asked for voluntary discharge.</p><p id="par0015" class="elsevierStylePara elsevierViewall">A year later he was readmitted for a new seizure of similar characteristics. He underwent further tests, starting with a contrast-enhanced brain MRI, which showed a right frontobasal expansive process, measuring 1.6 × 1,7 × 1,6 cm (AP × T × CC), completely cystic, ring-like contrast enhancement, with perilesional oedema (in its anterior part), which restricted diffusion, but no scolex was evident in the 3D sequence, with lipid-lactate peak in the spectroscopy (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>). The CSF study was normal, with normal CSF adenosine deaminase, negative CSF BK, negative CSF Gen-Xpert, negative CSF Gen-Xpert, negative Quantiferon TB, negative Western Blot for NCC and echinococcosis. The patient was given a new antibiotic regimen for 21 days with no objective improvement on imaging tests.</p><elsevierMultimedia ident="fig0005"></elsevierMultimedia><p id="par0020" class="elsevierStylePara elsevierViewall">Due to a history of adverse reaction to antituberculosis drugs, having completed a new antibiotic treatment regimen with no response and with all etiological studies being negative, an excisional biopsy was decided. The patient underwent a lateral orbital craniotomy, through a supraciliary incision, first performing a supraorbital craniotomy plus biopsy, which was reported as a severe inflammatory infiltrate without an aetiological diagnosis, so he was admitted for a second surgery, in which the craniotomy was extended laterally and complete lesion resection was achieved. The pathological anatomy showed brain tissue with severe chronic lymphohistiocytic inflammatory process in association with the presence of an isolated structure with cuticular outer layer corresponding to cysticercus larvae (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>).</p><p id="par0025" class="elsevierStylePara elsevierViewall">The patient was given a course of albendazole 400 mg orally every 12 h for 2 weeks without corticosteroids, with clinical improvement, with no new seizures. The contrast-enhanced brain MRI and the follow-up contrast-enhanced brain CT scan at 3 months showed no lesion recurrence, with no major complications. The MRI performed a year earlier showed a lesion with poorly defined but contrast-enhancing margins and no restriction, i.e., it could correspond to a lesion in the colloidal stage. The new MRI showed a lesion that had a hyperintense ring sign due to gliosis, which already showed restriction, so it could correspond to the granular-nodular stage. In patients with a single enhancing lesion, morphology is inconclusive and serology is commonly negative.<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a> The differential diagnosis includes other intracranial infections such as tuberculoma, toxoplasmosis, primary or secondary tumours.<a class="elsevierStyleCrossRef" href="#bib0015"><span class="elsevierStyleSup">3</span></a></p><p id="par0030" class="elsevierStylePara elsevierViewall">Regarding diagnosis, the enzyme-linked immunoelectrotransfer blot has a sensitivity of 98% and a specificity of 100%. There are false negatives, but these are restricted to patients with calcified NCC or in patients with a single cyst or in single degenerative lesion, with the sensitivity in the latter being as low as 60%.<a class="elsevierStyleCrossRef" href="#bib0020"><span class="elsevierStyleSup">4</span></a> This is why our patient's test results were negative.</p><p id="par0035" class="elsevierStylePara elsevierViewall">According to the Infectious Diseases Society of America, the recommended treatment for such patients is the administration of antiparasitic drugs, preferably albendazole, with or without corticosteroids, as well as anticonvulsant medication until resolution of the lesion on neuroimaging. Surgical resection is not recommended as first line. In addition, anticonvulsants are given for 6 months if the seizures are controlled and the Imaging study is negative.<a class="elsevierStyleCrossRef" href="#bib0025"><span class="elsevierStyleSup">5</span></a></p><p id="par0040" class="elsevierStylePara elsevierViewall">In conclusion, the single enhancing lesion is a subtype of parenchymal NCC, which becomes a diagnostic challenge due to the high rate of negative serological studies, and has granulomas (tuberculous or not), abscesses and even primary or secondary neoplasms as differential diagnoses.</p><span id="sec0005" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0005">Authorship</span><p id="par0045" class="elsevierStylePara elsevierViewall">John F. Vargas Urbina conceived and designed the research. John F. Vargas Urbina, Raúl E. Martinez Silva and William Anicama Lima collected the data and drafted and approved the final version of the article. John F. Vargas Urbina and Raúl E. Martinez Silva analysed the data and drafted the tables and graphs. John F. Vargas Urbina and William Anicama Lima critically reviewed the article. Authors are responsible for the content of the article and undertake to respond appropriately to any questions that may be necessary to ensure the accuracy of the data and the integrity of any part of their research.</p></span><span id="sec0010" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0010">Funding</span><p id="par0050" class="elsevierStylePara elsevierViewall">Self-funded.</p></span><span id="sec0015" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0015">Conflict of interest</span><p id="par0055" class="elsevierStylePara elsevierViewall">The authors declare that they have no conflict of interest.</p></span></span>" "textoCompletoSecciones" => array:1 [ "secciones" => array:4 [ 0 => array:2 [ "identificador" => "sec0005" "titulo" => "Authorship" ] 1 => array:2 [ "identificador" => "sec0010" "titulo" => "Funding" ] 2 => array:2 [ "identificador" => "sec0015" "titulo" => "Conflict of interest" ] 3 => array:1 [ "titulo" => "References" ] ] ] "pdfFichero" => "main.pdf" "tienePdf" => true "multimedia" => array:1 [ 0 => array:8 [ "identificador" => "fig0005" "etiqueta" => "Figure 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1250 "Ancho" => 1340 "Tamanyo" => 298298 ] ] "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at0005" "detalle" => "Figure " "rol" => "short" ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">A. Coronal T1-weighted contrast-enhanced brain magnetic resonance showing a cystic lesion with contrast enhancement in its periphery, with an apparent nodule in its inferomedial part, with apparent central necrosis (arrow). B. Presence of severe lymphohistiocytic infiltrate and abundant macrophages, and centrally, a cross section of a larva with invaginations of its wall (arrow). Haematoxylin-eosin 4×. C. Cross section of cysticercus larva at the level of the scolex, showing the wavy tegument with microvilli and the presence of the hooks (arrow). Haematoxylin-eosin 40×.</p>" ] ] ] "bibliografia" => array:2 [ "titulo" => "References" "seccion" => array:1 [ 0 => array:2 [ "identificador" => "bibs0005" "bibliografiaReferencia" => array:5 [ 0 => array:3 [ "identificador" => "bib0005" "etiqueta" => "1" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Solitary brain mass in a patient with seizures: An unexpected infectious etiology" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "M. Raja" 1 => "J. Gonzales Zamora" 2 => "A. Hassoun" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.3390/diseases6030054" "Revista" => array:5 [ "tituloSerie" => "Diseases" "fecha" => "2018" "volumen" => "6" "paginaInicial" => "54" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/29932160" "web" => "Medline" ] ] ] ] ] ] ] ] 1 => array:3 [ "identificador" => "bib0010" "etiqueta" => "2" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "New diagnostic criteria for neurocysticercosis: Reliability and validity" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "A. Carpio" 1 => "A. Fleury" 2 => "M.L. Romo" 3 => "R. Abraham" 4 => "J. Fandiño" 5 => "J. Durán" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1002/ana.24732" "Revista" => array:6 [ "tituloSerie" => "Ann Neurol" "fecha" => "2016" "volumen" => "80" "paginaInicial" => "434" "paginaFinal" => "442" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/27438337" "web" => "Medline" ] ] ] ] ] ] ] ] 2 => array:3 [ "identificador" => "bib0015" "etiqueta" => "3" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Neurocysticercosis presented as a solitary cystic parenchymal lesion mimicking primary brain tumor: A case report" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:6 [ 0 => "A. Soejitno" 1 => "I.W. Niryana" 2 => "N.P. Sriwidyani" 3 => "N.M. Susilawathi" 4 => "N.P. Witari" 5 => "A.A.R. Sudewi" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.idcr.2020.e01004" "Revista" => array:3 [ "tituloSerie" => "IDCases" "fecha" => "2020" "volumen" => "22" ] ] ] ] ] ] 3 => array:3 [ "identificador" => "bib0020" "etiqueta" => "4" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Neurocysticercosis" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "O.H. Del Brutto" 1 => "H.H. Garcia" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/B978-0-444-53490-3.00025-X" "Libro" => array:4 [ "fecha" => "2013" "paginaInicial" => "313" "paginaFinal" => "325" "editorial" => "Elsevier" ] ] ] ] ] ] 4 => array:3 [ "identificador" => "bib0025" "etiqueta" => "5" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Diagnosis and Treatment of Neurocysticercosis: 2017 Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA) and the American Society of Tropical Medicine and Hygiene (ASTMH)" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "A.C. White" 1 => "C.M. Coyle" 2 => "V. Rajshekhar" 3 => "G. Singh" 4 => "W.A. Hauser" 5 => "A. Mohanty" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1093/cid/cix1084" "Revista" => array:5 [ "tituloSerie" => "Clin Infect Dis" "fecha" => "2018" "volumen" => "66" "paginaInicial" => "e49" "paginaFinal" => "e75" ] ] ] ] ] ] ] ] ] ] ] "idiomaDefecto" => "en" "url" => "/23870206/0000016100000004/v1_202308280911/S2387020623003170/v1_202308280911/en/main.assets" "Apartado" => array:4 [ "identificador" => "43309" "tipo" => "SECCION" "en" => array:2 [ "titulo" => "Letters to the Editor" "idiomaDefecto" => true ] "idiomaDefecto" => "en" ] "PDF" => "https://static.elsevier.es/multimedia/23870206/0000016100000004/v1_202308280911/S2387020623003170/v1_202308280911/en/main.pdf?idApp=UINPBA00004N&text.app=https://www.elsevier.es/" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020623003170?idApp=UINPBA00004N" ]
Journal Information
Vol. 161. Issue 4.
Pages 177-178 (August 2023)
Share
Download PDF
More article options
Vol. 161. Issue 4.
Pages 177-178 (August 2023)
Letter to the Editor
Neurocysticercosis: A rare cause of a single brain granuloma
Neurocisticercosis: causa infrecuente de granuloma cerebral único
Article information
These are the options to access the full texts of the publication Medicina Clínica (English Edition)
Subscriber
Subscribe
Purchase
Contact
Phone for subscriptions and reporting of errors
From Monday to Friday from 9 a.m. to 6 p.m. (GMT + 1) except for the months of July and August which will be from 9 a.m. to 3 p.m.
Calls from Spain
932 415 960
Calls from outside Spain
+34 932 415 960
E-mail