array:24 [ "pii" => "S2387020619302323" "issn" => "23870206" "doi" => "10.1016/j.medcle.2019.05.003" "estado" => "S300" "fechaPublicacion" => "2019-07-19" "aid" => "4747" "copyright" => "Elsevier España, S.L.U.. All rights reserved" "copyrightAnyo" => "2019" "documento" => "article" "crossmark" => 1 "subdocumento" => "sco" "cita" => "Med Clin. 2019;153:78-81" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "Traduccion" => array:1 [ "es" => array:19 [ "pii" => "S0025775319300478" "issn" => "00257753" "doi" => "10.1016/j.medcli.2019.01.001" "estado" => "S300" "fechaPublicacion" => "2019-07-19" "aid" => "4747" "copyright" => "Elsevier España, S.L.U." "documento" => "article" "crossmark" => 1 "subdocumento" => "sco" "cita" => "Med Clin. 2019;153:78-81" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:2 [ "total" => 64 "formatos" => array:3 [ "EPUB" => 1 "HTML" => 33 "PDF" => 30 ] ] "es" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Artículo especial</span>" "titulo" => "Nuevos mecanismos en la trombosis venosa: inmunotrombosis" "tienePdf" => "es" "tieneTextoCompleto" => "es" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "78" "paginaFinal" => "81" ] ] "titulosAlternativos" => array:1 [ "en" => array:1 [ "titulo" => "New mechanisms in vein thrombosis: Immunothrombosis" ] ] "contieneTextoCompleto" => array:1 [ "es" => true ] "contienePdf" => array:1 [ "es" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Figura 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 614 "Ancho" => 1192 "Tamanyo" => 45782 ] ] "descripcion" => array:1 [ "es" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Mecanismos implicados en la iniciación de la trombosis venosa.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "José Antonio Páramo, Ramón Lecumberri" "autores" => array:2 [ 0 => array:2 [ "nombre" => "José Antonio" "apellidos" => "Páramo" ] 1 => array:2 [ "nombre" => "Ramón" "apellidos" => "Lecumberri" ] ] ] ] ] "idiomaDefecto" => "es" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S2387020619302323" "doi" => "10.1016/j.medcle.2019.05.003" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020619302323?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775319300478?idApp=UINPBA00004N" "url" => "/00257753/0000015300000002/v2_202005080620/S0025775319300478/v2_202005080620/es/main.assets" ] ] "itemSiguiente" => array:19 [ "pii" => "S2387020619302244" "issn" => "23870206" "doi" => "10.1016/j.medcle.2018.10.021" "estado" => "S300" "fechaPublicacion" => "2019-07-19" "aid" => "4704" "copyright" => "Elsevier España, S.L.U." "documento" => "article" "crossmark" => 1 "subdocumento" => "pgl" "cita" => "Med Clin. 2019;153:82.e1-82.e17" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:12 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Consensus statement</span>" "titulo" => "Clinical guide for the diagnosis and follow-up of myotonic dystrophy type 1, MD1 or Steinert's disease" "tienePdf" => "en" "tieneTextoCompleto" => "en" "tieneResumen" => array:2 [ 0 => "en" 1 => "es" ] "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "82.e1" "paginaFinal" => "82.e17" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Guía clínica para el diagnóstico y seguimiento de la distrofia miotónica tipo 1, DM1 o enfermedad de Steinert" ] ] "contieneResumen" => array:2 [ "en" => true "es" => true ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Gerardo Gutiérrez Gutiérrez, Jordi Díaz-Manera, Míriam Almendrote, Sharona Azriel, José Eulalio Bárcena, Pablo Cabezudo García, Ana Camacho Salas, Carlos Casanova Rodríguez, Ana María Cobo, Patricia Díaz Guardiola, Roberto Fernández-Torrón, María Pía Gallano Petit, Pablo García Pavía, María Gómez Gallego, Antonio José Gutiérrez Martínez, Ivonne Jericó, Solange Kapetanovic García, Adolfo López de Munaín Arregui, Loreto Martorell, Germán Morís de la Tassa, Raúl Moreno Zabaleta, José Luis Muñoz-Blanco, Juana Olivar Roldán, Samuel Ignacio Pascual Pascual, Rafael Peinado Peinado, Helena Pérez, Juan José Poza Aldea, María Rabasa, Alba Ramos, Alfredo Rosado Bartolomé, Miguel Ángel Rubio Pérez, Jon Andoni Urtizberea, Gustavo Zapata-Wainberg, Eduardo Gutiérrez-Rivas" "autores" => array:34 [ 0 => array:2 [ "nombre" => "Gerardo" "apellidos" => "Gutiérrez Gutiérrez" ] 1 => array:2 [ "nombre" => "Jordi" "apellidos" => "Díaz-Manera" ] 2 => array:2 [ "nombre" => "Míriam" "apellidos" => "Almendrote" ] 3 => array:2 [ "nombre" => "Sharona" "apellidos" => "Azriel" ] 4 => array:2 [ "nombre" => "José" "apellidos" => "Eulalio Bárcena" ] 5 => array:2 [ "nombre" => "Pablo" "apellidos" => "Cabezudo García" ] 6 => array:2 [ "nombre" => "Ana" "apellidos" => "Camacho Salas" ] 7 => array:2 [ "nombre" => "Carlos" "apellidos" => "Casanova Rodríguez" ] 8 => array:2 [ "nombre" => "Ana María" "apellidos" => "Cobo" ] 9 => array:2 [ "nombre" => "Patricia" "apellidos" => "Díaz Guardiola" ] 10 => array:2 [ "nombre" => "Roberto" "apellidos" => "Fernández-Torrón" ] 11 => array:2 [ "nombre" => "María Pía" "apellidos" => "Gallano Petit" ] 12 => array:2 [ "nombre" => "Pablo" "apellidos" => "García Pavía" ] 13 => array:2 [ "nombre" => "María" "apellidos" => "Gómez Gallego" ] 14 => array:2 [ "nombre" => "Antonio José" "apellidos" => "Gutiérrez Martínez" ] 15 => array:2 [ "nombre" => "Ivonne" "apellidos" => "Jericó" ] 16 => array:2 [ "nombre" => "Solange" "apellidos" => "Kapetanovic García" ] 17 => array:2 [ "nombre" => "Adolfo" "apellidos" => "López de Munaín Arregui" ] 18 => array:2 [ "nombre" => "Loreto" "apellidos" => "Martorell" ] 19 => array:2 [ "nombre" => "Germán" "apellidos" => "Morís de la Tassa" ] 20 => array:2 [ "nombre" => "Raúl" "apellidos" => "Moreno Zabaleta" ] 21 => array:2 [ "nombre" => "José Luis" "apellidos" => "Muñoz-Blanco" ] 22 => array:2 [ "nombre" => "Juana" "apellidos" => "Olivar Roldán" ] 23 => array:2 [ "nombre" => "Samuel Ignacio" "apellidos" => "Pascual Pascual" ] 24 => array:2 [ "nombre" => "Rafael" "apellidos" => "Peinado Peinado" ] 25 => array:2 [ "nombre" => "Helena" "apellidos" => "Pérez" ] 26 => array:2 [ "nombre" => "Juan José" "apellidos" => "Poza Aldea" ] 27 => array:2 [ "nombre" => "María" "apellidos" => "Rabasa" ] 28 => array:2 [ "nombre" => "Alba" "apellidos" => "Ramos" ] 29 => array:2 [ "nombre" => "Alfredo" "apellidos" => "Rosado Bartolomé" ] 30 => array:2 [ "nombre" => "Miguel Ángel" "apellidos" => "Rubio Pérez" ] 31 => array:2 [ "nombre" => "Jon Andoni" "apellidos" => "Urtizberea" ] 32 => array:2 [ "nombre" => "Gustavo" "apellidos" => "Zapata-Wainberg" ] 33 => array:2 [ "nombre" => "Eduardo" "apellidos" => "Gutiérrez-Rivas" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0025775318307310" "doi" => "10.1016/j.medcli.2018.10.028" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775318307310?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020619302244?idApp=UINPBA00004N" "url" => "/23870206/0000015300000002/v2_202004301535/S2387020619302244/v2_202004301535/en/main.assets" ] "itemAnterior" => array:19 [ "pii" => "S2387020619302311" "issn" => "23870206" "doi" => "10.1016/j.medcle.2019.05.002" "estado" => "S300" "fechaPublicacion" => "2019-07-19" "aid" => "4759" "copyright" => "Elsevier España, S.L.U." "documento" => "article" "crossmark" => 1 "subdocumento" => "rev" "cita" => "Med Clin. 2019;153:70-7" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:13 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Review</span>" "titulo" => "Update in status epilepticus" "tienePdf" => "en" "tieneTextoCompleto" => "en" "tieneResumen" => array:2 [ 0 => "en" 1 => "es" ] "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "70" "paginaFinal" => "77" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Actualización en el estado de mal epiléptico (<span class="elsevierStyleItalic">status epilepticus</span>)" ] ] "contieneResumen" => array:2 [ "en" => true "es" => true ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 3886 "Ancho" => 2990 "Tamanyo" => 664325 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0020" class="elsevierStyleSimplePara elsevierViewall">Status epilepticus treatment diagram.</p> <p id="spar0025" class="elsevierStyleSimplePara elsevierViewall">cEEG: continuous electroencephalogram; SE: status epilepticus; EEG: electroencephalogram; AEDs: antiepileptic drugs; LCM: lacosamide; LEV: levetiracetam; MDZ: midazolam; min: minute; PB: phenobarbital; PHT: phenytoin; PPF: propofol; SE: status epilepticus; VPA: valproic acid.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Estevo Santamarina, Laura Abraira, Manuel Toledo" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Estevo" "apellidos" => "Santamarina" ] 1 => array:2 [ "nombre" => "Laura" "apellidos" => "Abraira" ] 2 => array:2 [ "nombre" => "Manuel" "apellidos" => "Toledo" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0025775319300594" "doi" => "10.1016/j.medcli.2019.01.013" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775319300594?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020619302311?idApp=UINPBA00004N" "url" => "/23870206/0000015300000002/v2_202004301535/S2387020619302311/v2_202004301535/en/main.assets" ] "en" => array:17 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Special article</span>" "titulo" => "New mechanisms in venous thrombosis: Immunothrombosis" "tieneTextoCompleto" => true "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "78" "paginaFinal" => "81" ] ] "autores" => array:1 [ 0 => array:4 [ "autoresLista" => "José Antonio Páramo, Ramón Lecumberri" "autores" => array:2 [ 0 => array:4 [ "nombre" => "José Antonio" "apellidos" => "Páramo" "email" => array:1 [ 0 => "japaramo@unav.es" ] "referencia" => array:4 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">a</span>" "identificador" => "aff0005" ] 1 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">b</span>" "identificador" => "aff0010" ] 2 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">c</span>" "identificador" => "aff0015" ] 3 => array:2 [ "etiqueta" => "*" "identificador" => "cor0005" ] ] ] 1 => array:3 [ "nombre" => "Ramón" "apellidos" => "Lecumberri" "referencia" => array:3 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">a</span>" "identificador" => "aff0005" ] 1 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">b</span>" "identificador" => "aff0010" ] 2 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">c</span>" "identificador" => "aff0015" ] ] ] ] "afiliaciones" => array:3 [ 0 => array:3 [ "entidad" => "Servicio de Hematología, Clínica Universidad de Navarra, Pamplona, Spain" "etiqueta" => "a" "identificador" => "aff0005" ] 1 => array:3 [ "entidad" => "Instituto Sanitario de Navarra (IdisNa), Pamplona, Spain" "etiqueta" => "b" "identificador" => "aff0010" ] 2 => array:3 [ "entidad" => "CIBER Investigación Cardiovascular (CIBERCV), Spain" "etiqueta" => "c" "identificador" => "aff0015" ] ] "correspondencia" => array:1 [ 0 => array:3 [ "identificador" => "cor0005" "etiqueta" => "⁎" "correspondencia" => "Corresponding author." ] ] ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Nuevos mecanismos en la trombosis venosa: inmunotrombosis" ] ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 648 "Ancho" => 1144 "Tamanyo" => 45236 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Mechanisms involved in the initiation of venous thrombosis.</p>" ] ] ] "textoCompleto" => "<span class="elsevierStyleSections"><p id="par0005" class="elsevierStylePara elsevierViewall">Deep vein thrombosis (DVT) and its main complication, pulmonary embolism (PE), collectively called venous thromboembolic disease (VTE), represent a global public health problem, as it is an important cause of mortality and morbidity. VTE is the third cause of cardiovascular mortality after acute myocardial infarction and ischaemic stroke, with more than 1,000,000 cases per year and more than 300,000 deaths in the European Union.<a class="elsevierStyleCrossRef" href="#bib0160"><span class="elsevierStyleSup">1</span></a> An interesting fact is that VTE prevalence and mortality have not decreased substantially in the last 30 years, despite progress in diagnostic and preventive methods.<a class="elsevierStyleCrossRef" href="#bib0165"><span class="elsevierStyleSup">2</span></a> DVT develops generally, though not exclusively, in the lower limb veins and occurs asymptomatically in most patients, but may cause symptoms including pain, redness, and swelling; the clot can be released and migrate into the pulmonary circulation causing a PE. The importance of the problem has given rise to different initiatives and calls for action related to conducting research in this condition.<a class="elsevierStyleCrossRef" href="#bib0170"><span class="elsevierStyleSup">3</span></a> Although DVT has been classically considered as a coagulation disorder, there is recent evidence showing that immune cells and inflammatory processes are involved in the initiation of the process, which implies a paradigm shift.<a class="elsevierStyleCrossRef" href="#bib0175"><span class="elsevierStyleSup">4</span></a></p><span id="sec0005" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0005">Pathophysiology of thrombosis</span><p id="par0010" class="elsevierStylePara elsevierViewall">The purpose of the coagulation process is the generation of fibrin from its precursor fibrinogen by the action of thrombin. Fibrin represents the most important structural component of the thrombus. Thrombin is generated from prothrombin by the action of activated factor X. Factor X activation can occur in two ways, known as extrinsic and intrinsic; the first is initiated by the tissue factor (TF) present when the subendothelium is exposed after vascular injury. The intrinsic pathway begins with the activation of factor XII by negatively charged surfaces.<a class="elsevierStyleCrossRef" href="#bib0180"><span class="elsevierStyleSup">5</span></a></p><p id="par0015" class="elsevierStylePara elsevierViewall">According to this model, the current paradigm for the prevention of DVT is based on interfering with the coagulation system by means of vitamin K antagonist drugs (e.g. Sintrom®) or thrombin inhibitors (e.g. dabigatran) and factor Xa (e.g. rivaroxaban or apixaban). Nevertheless, due to the overlap between the mechanisms of haemostasis and thrombosis, the therapeutic window for the use of anticoagulants is narrow, which increases the risk of haemorrhagic complications. The role of the immune system in the pathogenesis of VTE involves a change of paradigm, as it is considered an inflammatory state with participation of the immune system, called immunothrombosis, rather than just a process exclusively dependent on coagulation.<a class="elsevierStyleCrossRefs" href="#bib0185"><span class="elsevierStyleSup">6,7</span></a></p></span><span id="sec0010" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0010">Initiation of venous thrombosis</span><p id="par0020" class="elsevierStylePara elsevierViewall">The initiation of venous thrombosis involves a cascade of processes that can be divided into: (1) circulatory stasis and hypoxia, (2) endothelial activation and (3) cellular recruitment, coagulation activation and thrombus development<a class="elsevierStyleCrossRef" href="#bib0175"><span class="elsevierStyleSup">4</span></a> (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>).</p><elsevierMultimedia ident="fig0005"></elsevierMultimedia><span id="sec0015" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0015">Stasis and hypoxia trigger venous thrombosis.</span><p id="par0025" class="elsevierStylePara elsevierViewall">DVT develops preferably in venous valves; as the blood pressure decreases from the heart to the veins, the function of the heart may be insufficient to maintain proper circulation. The auxiliary role of the calf muscles is necessary to pump blood and prevent its slowing down. When these muscles do not contract properly, the speed of the blood is reduced, producing circulatory stasis, which is currently considered one of the main factors of DVT.<a class="elsevierStyleCrossRef" href="#bib0195"><span class="elsevierStyleSup">8</span></a> This process can be favoured by the position of the individual, as happens after surgery, immobilization or after prolonged travel. Animal models have been developed that simulate totally or partially the situation of stasis by applying total or partial ligature of the inferior vena cava.<a class="elsevierStyleCrossRef" href="#bib0175"><span class="elsevierStyleSup">4</span></a> Likewise, the important role of circulatory stasis in the venous valve has been established using computer models.<a class="elsevierStyleCrossRef" href="#bib0200"><span class="elsevierStyleSup">9</span></a></p><p id="par0030" class="elsevierStylePara elsevierViewall">The only source of oxygen for a vein is the blood that circulates inside it. Slower circulation implies local hypoxia, which is considered a crucial pathogenic mechanism for the development of thrombosis. It has been demonstrated, both clinically and experimentally, that oxygenation in the venous valves significantly decreases when the flow becomes static, returning to normal when pulsatile (as is the case with the effect produced by the calf muscles). Hypoxia will contribute to DVT by activating various cell types, such as mast cells and endothelium, leading to the expression of adhesion receptors (such as ICAM-1) and release of constituents present in the Weibel–Palade granules of the endothelium, such as von Willebrand factor (VWF); this cascade of events is considered a prerequisite for the local recruitment of leukocytes and platelets, promoting thrombosis.<a class="elsevierStyleCrossRef" href="#bib0205"><span class="elsevierStyleSup">10</span></a></p></span><span id="sec0020" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0020">Endothelial activation</span><p id="par0035" class="elsevierStylePara elsevierViewall">Endothelial activation is a central process in the initiation of DVT. During the same, endothelial cells release constituents present in the Weibel–Palade granules, such as VWF and P-selectin, which are elevated in patients with DVT and can play an important role, since their inhibition reduces DVT and improves the recanalization in animal models.<a class="elsevierStyleCrossRef" href="#bib0210"><span class="elsevierStyleSup">11</span></a> Hypoxia will favour endothelial activation mediated by reactive oxygen species (ROS), inducing complement activation, which is associated with an increased susceptibility to DVT in experimental models.<a class="elsevierStyleCrossRef" href="#bib0215"><span class="elsevierStyleSup">12</span></a> It has been shown that mice deficient in C3 or C5 show a reduction in DVT at an experimental level, while high levels of C3 are associated with a high risk of DVT at clinical level.<a class="elsevierStyleCrossRef" href="#bib0220"><span class="elsevierStyleSup">13</span></a></p><p id="par0040" class="elsevierStylePara elsevierViewall">Endothelial activation favours the recruitment and extravasation of leukocytes that will also play a relevant pathophysiological role. In addition, the activated endothelium exerts procoagulant functions contributing to thrombus formation.<a class="elsevierStyleCrossRef" href="#bib0225"><span class="elsevierStyleSup">14</span></a></p><p id="par0045" class="elsevierStylePara elsevierViewall">It has recently been shown that endothelial activation and cellular recruitment induced by local hypoxia require another intermediate component, mast cells. Mast cells are part of the innate immune system in the vicinity of blood vessels. They contain granules rich in inflammatory mediators, such as tumour necrosis factor (TNF-α) and histamine, but also antithrombotic factors, such as tissue plasminogen activator (t-PA) and heparin. Its role in the onset of DVT is supported by the accumulation observed in the sites of venous thrombosis formation. In addition, mice deficient in mast cells are protected from DVT. These data suggest that the presence of mast cells is a requirement for the initiation of thrombosis.<a class="elsevierStyleCrossRef" href="#bib0230"><span class="elsevierStyleSup">15</span></a> While mast cell deficiency provides antithrombotic protection that is accompanied by a reduction in cellular recruitment, its degranulation exacerbates venous thrombosis, in part by the release of histamine, which possesses prothrombotic properties, inducing the release of VWF and P-selectin by leukocytes, as well as increased expression of selectins and ICAM-1. Histamine also stimulates the expression of TF, the main initiator of coagulation.<a class="elsevierStyleCrossRef" href="#bib0235"><span class="elsevierStyleSup">16</span></a> The importance of mast cells in venous thrombosis is confirmed by the clear link between allergic reactions and DVT. The severity of asthma correlates, not only with DVT, but with pulmonary embolism.<a class="elsevierStyleCrossRef" href="#bib0240"><span class="elsevierStyleSup">17</span></a></p><p id="par0050" class="elsevierStylePara elsevierViewall">The mechanisms of mast cell activation by hypoxia are not well known, but oxidative stress and ROS generation seem to play a role in this process.<a class="elsevierStyleCrossRef" href="#bib0245"><span class="elsevierStyleSup">18</span></a> Therefore, inhibiting the activation or degranulation of mast cells may constitute a new therapeutic approach in DVT.</p></span><span id="sec0025" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0025">Cell recruitment and activation</span><p id="par0055" class="elsevierStylePara elsevierViewall">The restriction of the venous flow induces a rapid leucocyte recruitment. After causing stenosis in the inferior vena cava for the first hour, the leukocytes begin to move and adhere to the venous endothelium, covering the endothelial surface at 5–6<span class="elsevierStyleHsp" style=""></span>h. The main component are neutrophils that represent 80% of adherent cells followed by monocytes.<a class="elsevierStyleCrossRef" href="#bib0250"><span class="elsevierStyleSup">19</span></a> Leucocyte recruitment is dependent on the exposure of selectin-P in the luminal region of the venous endothelium, since the number of leukocytes recruited is significantly reduced in mice deficient in this adhesion molecule, being also protected from DVT in response to a slow flow. Leucocyte recruitment may also be affected by low density lipoprotein (LDL) plasma levels since PCSK9 deficiency (proprotein convertase subtilisin/kexin type 9) significantly reduces adhesion and thrombus growth in stenosis models.<a class="elsevierStyleCrossRef" href="#bib0255"><span class="elsevierStyleSup">20</span></a></p></span><span id="sec0030" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0030">Neutrophils</span><p id="par0060" class="elsevierStylePara elsevierViewall">Recent studies have shown a critical role of neutrophils in the pathophysiology of DVT. After their recruitment, neutrophils undergo processes of activation and release of their nuclear material forming structures called <span class="elsevierStyleItalic">neutrophil extracellular traps</span> (NET), composed of DNA, histones and constituents secreted by granules such as myeloperoxidase, involved in antimicrobial defense.<a class="elsevierStyleCrossRef" href="#bib0260"><span class="elsevierStyleSup">21</span></a> Various signals trigger the NET generation process, known as NETosis. Experiments performed in neutropenic mice show that neutrophils are the main source of NET in DVT, which are present inside thrombi<a class="elsevierStyleCrossRefs" href="#bib0265"><span class="elsevierStyleSup">22,23</span></a> the prevention of NETosis or NET destruction by infusion of DNAses protects the mouse from thrombus formation in stenosis models, indicating the important role of NETs in the initiation of DVT.<a class="elsevierStyleCrossRefs" href="#bib0260"><span class="elsevierStyleSup">21,22</span></a></p><p id="par0065" class="elsevierStylePara elsevierViewall">The mechanisms by which NETs can contribute to thrombosis have been an area of important research. It is known that histones induce endothelial activation and that NETs stimulate adhesion and platelet aggregation, effects that are abolished by histone inactivation. Another important mechanism of NETs prothrombotic effect has to do with the activation of the coagulation cascade and the reduction of anticoagulant activity. NETs activate the contact system by factor XII and degrade anticoagulants such as the inhibitor of the tissue factor pathway and the activation of protein C mediated by thrombomodulin, thus enhancing the generation of thrombin. Consequently, NETs represent an important mechanism in venous thrombogenesis.<a class="elsevierStyleCrossRefs" href="#bib0185"><span class="elsevierStyleSup">6,7,24</span></a></p></span><span id="sec0035" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0035">Monocytes</span><p id="par0070" class="elsevierStylePara elsevierViewall">Monocytes recruited to the area of venous thrombosis serve as a source of TF, the main initiator of blood coagulation and fibrin deposition. Deletion of TF in leukocytes completely prevents the formation of the thrombus in animal models of stenosis, without affecting its recruitment. This prothrombotic function is negatively regulated by the <span class="elsevierStyleItalic">toll-like</span> receptor 9 (TLR-9), since the deficiency of this receptor reduces the monocyte recruitment in the venous thrombus.<a class="elsevierStyleCrossRef" href="#bib0280"><span class="elsevierStyleSup">25</span></a></p></span><span id="sec0040" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0040">Platelets</span><p id="par0075" class="elsevierStylePara elsevierViewall">Platelets are recruited very early in the venous wall once flow restriction occurs and play an important role in thrombogenesis, since platelet depletion and antiplatelet therapy (aspirin) reduces DVT in mice,<a class="elsevierStyleCrossRef" href="#bib0285"><span class="elsevierStyleSup">26</span></a> as well as in patients undergoing orthopaedic surgery.<a class="elsevierStyleCrossRef" href="#bib0290"><span class="elsevierStyleSup">27</span></a> Unlike arterial thrombosis, where platelets form large aggregates, in DVT they are recruited unitarily, adhering directly to the endothelium or to leukocytes forming small heterotypic aggregates. Platelet recruitment is mediated by the binding of the GpIb-α platelet receptor to VWF exposed on the endothelial surface, since its deficiency prevents DVT in experimental models. More recently, murine models of venous stenosis have demonstrated that platelet recruitment depends on another CLEC-2 receptor, which is capable of binding to a transmembrane protein expressed in the medial and adventitial layers, called podoplanin, whose expression is significantly increased in the course of thrombus formation.<a class="elsevierStyleCrossRef" href="#bib0295"><span class="elsevierStyleSup">28</span></a></p><p id="par0080" class="elsevierStylePara elsevierViewall">Platelet recruitment in hypoxic conditions depends on the inflammasome (NLRP3), a molecular platform responsible for the generation of proinflammatory cytokines such as IL-1β and IL18. NLRP3 deficiency is associated with reduction of thrombosis in stasis models, while an increase in IL-1 β and IL-1 has been observed in patients with DVT.<a class="elsevierStyleCrossRef" href="#bib0300"><span class="elsevierStyleSup">29</span></a></p><p id="par0085" class="elsevierStylePara elsevierViewall">In addition to platelet procoagulant activity, its vascular recruitment is a source of inflammatory stimuli, like danger-associated molecular patterns (DAMP), such as myeloid protein (MRP-14), favouring thrombogenesis, as well as NETosis and leucocyte recruitment.<a class="elsevierStyleCrossRef" href="#bib0305"><span class="elsevierStyleSup">30</span></a> It is interesting to note that the ability of platelets to promote such recruitment in the venous thrombus is regulated by the amyloid precursor protein (APP), since the genetic deficiency of APP is associated with increased NETosis and DVT growth<a class="elsevierStyleCrossRef" href="#bib0310"><span class="elsevierStyleSup">31</span></a>; therefore APP can represent a new approach in the prevention of DVT, reducing inflammation and NET production.</p></span></span><span id="sec0045" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0045">Conclusions</span><p id="par0090" class="elsevierStylePara elsevierViewall">DVT initiation mechanisms represent a cascade of episodes virtually identical to the local inflammatory response, recently called immunothrombosis, beyond a simple coagulation problem (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>). This is of interest because of the possibility of identifying new therapeutic targets that, acting on the immune system, are not involved in haemostasis, which would reduce or eradicate bleeding, which is the main complication of anticoagulation. Therefore, strategies aimed at reducing endothelial activation, cell content release and leucocyte recruitment may be promising in the prevention of venous thrombosis. For example, endothelial activation could be diminished by controlling mast cells degranulation. Other strategies would include improving the local response to hypoxia or the control of NETosis.</p><p id="par0095" class="elsevierStylePara elsevierViewall">In conclusion, DVT can be considered as a form of immunothrombosis with local inflammation playing an important role in the initial stages of thrombus formation. Acting on inflammation may prevent DVT more safely than by inhibiting coagulation mechanisms.</p></span><span id="sec0050" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0050">Conflict of interests</span><p id="par0100" class="elsevierStylePara elsevierViewall">The authors declare no conflict of interest.</p></span></span>" "textoCompletoSecciones" => array:1 [ "secciones" => array:5 [ 0 => array:2 [ "identificador" => "sec0005" "titulo" => "Pathophysiology of thrombosis" ] 1 => array:3 [ "identificador" => "sec0010" "titulo" => "Initiation of venous thrombosis" "secciones" => array:6 [ 0 => array:2 [ "identificador" => "sec0015" "titulo" => "Stasis and hypoxia trigger venous thrombosis." ] 1 => array:2 [ "identificador" => "sec0020" "titulo" => "Endothelial activation" ] 2 => array:2 [ "identificador" => "sec0025" "titulo" => "Cell recruitment and activation" ] 3 => array:2 [ "identificador" => "sec0030" "titulo" => "Neutrophils" ] 4 => array:2 [ "identificador" => "sec0035" "titulo" => "Monocytes" ] 5 => array:2 [ "identificador" => "sec0040" "titulo" => "Platelets" ] ] ] 2 => array:2 [ "identificador" => "sec0045" "titulo" => "Conclusions" ] 3 => array:2 [ "identificador" => "sec0050" "titulo" => "Conflict of interests" ] 4 => array:1 [ "titulo" => "References" ] ] ] "pdfFichero" => "main.pdf" "tienePdf" => true "fechaRecibido" => "2018-12-28" "fechaAceptado" => "2019-01-17" "NotaPie" => array:1 [ 0 => array:2 [ "etiqueta" => "☆" "nota" => "<p class="elsevierStyleNotepara" id="npar0005">Please cite this article as: Páramo JA, Lecumberri R. Nuevos mecanismos en la trombosis venosa: inmunotrombosis. Med Clin (Barc). 2019;153:78–81.</p>" ] ] "multimedia" => array:1 [ 0 => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 648 "Ancho" => 1144 "Tamanyo" => 45236 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Mechanisms involved in the initiation of venous thrombosis.</p>" ] ] ] "bibliografia" => array:2 [ "titulo" => "References" "seccion" => array:1 [ 0 => array:2 [ "identificador" => "bibs0015" "bibliografiaReferencia" => array:31 [ 0 => array:3 [ "identificador" => "bib0160" "etiqueta" => "1" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Thrombosis: a major contributor to global disease burden" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "G.E. Raskob" 1 => "P. Angchaisuksiri" 2 => "A.N. Blanco" 3 => "H. Buller" 4 => "A. Gallus" 5 => "B.J. Hunt" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1161/ATVBAHA.114.304488" "Revista" => array:6 [ "tituloSerie" => "Arterioscler Thromb Vasc Biol" "fecha" => "2014" "volumen" => "34" "paginaInicial" => "2363" "paginaFinal" => "2371" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/25304324" "web" => "Medline" ] ] ] ] ] ] ] ] 1 => array:3 [ "identificador" => "bib0165" "etiqueta" => "2" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Reasons for the persistent incidence of venous thromboembolism" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:6 [ 0 => "J.A. Heit" 1 => "A. Ashrani" 2 => "D.J. Crusan" 3 => "R.D. McBane" 4 => "T.M. Petterson" 5 => "K.R. Bailey" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Thromb Haemost" "fecha" => "2017" "volumen" => "117" "paginaInicial" => "390" "paginaFinal" => "400" ] ] ] ] ] ] 2 => array:3 [ "identificador" => "bib0170" "etiqueta" => "3" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Venous thromboembolism: an urgent call for action" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "J.A. Páramo" 1 => "R. Lecumberri" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Med Clin (Barc)" "fecha" => "2009" "volumen" => "133" "paginaInicial" => "547" "paginaFinal" => "551" ] ] ] ] ] ] 3 => array:3 [ "identificador" => "bib0175" "etiqueta" => "4" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Immune factors in deep vein thrombosis initiation" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "I. Budnik" 1 => "A. Brill" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.it.2018.04.010" "Revista" => array:6 [ "tituloSerie" => "Trends Immunol" "fecha" => "2018" "volumen" => "39" "paginaInicial" => "610" "paginaFinal" => "623" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/29776849" "web" => "Medline" ] ] ] ] ] ] ] ] 4 => array:3 [ "identificador" => "bib0180" "etiqueta" => "5" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "New fundamentals in hemostasis" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "H.H. Versteeg" 1 => "J.W. Heemskerk" 2 => "M. Levi" 3 => "P.H. Reitsma" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1152/physrev.00016.2011" "Revista" => array:6 [ "tituloSerie" => "Physiol Rev" "fecha" => "2013" "volumen" => "93" "paginaInicial" => "327" "paginaFinal" => "358" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/23303912" "web" => "Medline" ] ] ] ] ] ] ] ] 5 => array:3 [ "identificador" => "bib0185" "etiqueta" => "6" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Thrombosis as an intravascular effector of innate immunity" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "B. Englemann" 1 => "S. Massberg" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1038/nri3345" "Revista" => array:6 [ "tituloSerie" => "Nat Rev Immunol" "fecha" => "2013" "volumen" => "13" "paginaInicial" => "34" "paginaFinal" => "45" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/23222502" "web" => "Medline" ] ] ] ] ] ] ] ] 6 => array:3 [ "identificador" => "bib0190" "etiqueta" => "7" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Blood coagulation in immunothrombosis – at the frontline of intravascular immunity" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "F. Gaertner" 1 => "S. Massberg" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.smim.2016.10.010" "Revista" => array:6 [ "tituloSerie" => "Semin Immunol" "fecha" => "2016" "volumen" => "28" "paginaInicial" => "561" "paginaFinal" => "569" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/27866916" "web" => "Medline" ] ] ] ] ] ] ] ] 7 => array:3 [ "identificador" => "bib0195" "etiqueta" => "8" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Venous valvular stasis-associated hypoxia and thrombosis: what is the link?" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "E.G. Bovill" 1 => "A. van der Vliet" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1146/annurev-physiol-012110-142305" "Revista" => array:6 [ "tituloSerie" => "Annu Rev Physiol" "fecha" => "2011" "volumen" => "73" "paginaInicial" => "527" "paginaFinal" => "545" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/21034220" "web" => "Medline" ] ] ] ] ] ] ] ] 8 => array:3 [ "identificador" => "bib0200" "etiqueta" => "9" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Modelling and simulation of flow and agglomeration in deep veins valves using discrete multi physics" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "M. Ariane" 1 => "W. Wen" 2 => "D. Vigolo" 3 => "A. Brill" 4 => "F.G.B. Nash" 5 => "M. Barigou" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Comput Biol Med" "fecha" => "2017" "volumen" => "89" "paginaInicial" => "96" "paginaFinal" => "103" ] ] ] ] ] ] 9 => array:3 [ "identificador" => "bib0205" "etiqueta" => "10" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Activation of NLRP3 inflammasome complex potentiates venous thrombosis in response to hypoxia" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "N. Gupta" 1 => "A. Sahu" 2 => "A. Prabhakar" 3 => "T. Chatterjee" 4 => "T. Tyagi" 5 => "B. Kumari" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1073/pnas.1620458114" "Revista" => array:6 [ "tituloSerie" => "Proc Natl Acad Sci U S A" "fecha" => "2017" "volumen" => "114" "paginaInicial" => "4763" "paginaFinal" => "4768" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/28420787" "web" => "Medline" ] ] ] ] ] ] ] ] 10 => array:3 [ "identificador" => "bib0210" "etiqueta" => "11" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Circulating and vein wall P-selectin promote venous thrombogenesis during aging in a rodent model" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "D.L. Culmer" 1 => "J.A. Diaz" 2 => "A.E. Hawley" 3 => "T.O. Jackson" 4 => "K.A. Shuster" 5 => "R.E. Sigler" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.thromres.2012.10.013" "Revista" => array:6 [ "tituloSerie" => "Thromb Res" "fecha" => "2013" "volumen" => "131" "paginaInicial" => "42" "paginaFinal" => "48" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/23174624" "web" => "Medline" ] ] ] ] ] ] ] ] 11 => array:3 [ "identificador" => "bib0215" "etiqueta" => "12" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Oxidative stress and reactive oxygen species in endothelial dysfunction associated with cardiovascular and metabolic diseases" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:6 [ 0 => "M.A. Incalza" 1 => "R. D’Oria" 2 => "A. Natalicchio" 3 => "S. Perrini" 4 => "L. Laviola" 5 => "F. Giorgino" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.vph.2017.05.005" "Revista" => array:6 [ "tituloSerie" => "Vascul Pharmacol" "fecha" => "2018" "volumen" => "100" "paginaInicial" => "1" "paginaFinal" => "19" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/28579545" "web" => "Medline" ] ] ] ] ] ] ] ] 12 => array:3 [ "identificador" => "bib0220" "etiqueta" => "13" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Distinct contributions of complement factors to platelet activation and fibrin formation in venous thrombus development" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "S. Subramaniam" 1 => "K. Jurk" 2 => "L. Hobohm" 3 => "S. Jäckel" 4 => "M. Saffarzadeh" 5 => "K. Schwierczek" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1182/blood-2016-11-749879" "Revista" => array:6 [ "tituloSerie" => "Blood" "fecha" => "2017" "volumen" => "129" "paginaInicial" => "2291" "paginaFinal" => "2302" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/28223279" "web" => "Medline" ] ] ] ] ] ] ] ] 13 => array:3 [ "identificador" => "bib0225" "etiqueta" => "14" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Thrombotic regulation from the endothelial cell perspectives" "autores" => array:1 [ 0 => array:3 [ "colaboracion" => "on behalf of the Early Career Committee" "etal" => false "autores" => array:4 [ 0 => "M. Wang" 1 => "H. Hao" 2 => "N.J. Leeper" 3 => "L. Zhu" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1161/ATVBAHA.118.310367" "Revista" => array:6 [ "tituloSerie" => "Arterioscler Thromb Vasc Biol" "fecha" => "2018" "volumen" => "38" "paginaInicial" => "e90" "paginaFinal" => "e95" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/29793992" "web" => "Medline" ] ] ] ] ] ] ] ] 14 => array:3 [ "identificador" => "bib0230" "etiqueta" => "15" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Mast cells granular contents are crucial for deep vein thrombosis in mice" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:5 [ 0 => "T. Ponomaryov" 1 => "H. Payne" 2 => "L. Fabritz" 3 => "D.D. Wagner" 4 => "A. Brill" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1161/CIRCRESAHA.117.311185" "Revista" => array:6 [ "tituloSerie" => "Circ Res" "fecha" => "2017" "volumen" => "121" "paginaInicial" => "941" "paginaFinal" => "950" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/28739590" "web" => "Medline" ] ] ] ] ] ] ] ] 15 => array:3 [ "identificador" => "bib0235" "etiqueta" => "16" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Histamine induces activation of protein kinase D that mediates tissue factor expression and activity in human aortic smooth muscle cells" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "F. Hao" 1 => "D.D. Wu" 2 => "X. Xu" 3 => "M.Z. Cui" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1152/ajpheart.00500.2011" "Revista" => array:6 [ "tituloSerie" => "Am J Physiol Heart Circ Physiol" "fecha" => "2012" "volumen" => "303" "paginaInicial" => "H1344" "paginaFinal" => "H1352" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/23001835" "web" => "Medline" ] ] ] ] ] ] ] ] 16 => array:3 [ "identificador" => "bib0240" "etiqueta" => "17" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Adult asthmatics increase the risk of acute coronary syndrome: a nationwide population-based cohort study" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:6 [ 0 => "W.S. Chung" 1 => "T.C. Shen" 2 => "C.L. Lin" 3 => "Y.H. Chu" 4 => "W.H. Hsu" 5 => "C.H. Kao" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.ejim.2014.10.023" "Revista" => array:6 [ "tituloSerie" => "Eur J Intern Med" "fecha" => "2014" "volumen" => "25" "paginaInicial" => "941" "paginaFinal" => "945" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/25468246" "web" => "Medline" ] ] ] ] ] ] ] ] 17 => array:3 [ "identificador" => "bib0245" "etiqueta" => "18" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Role of reactive oxygen species in mast cell degranulation" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:5 [ 0 => "M.A. Chelombitko" 1 => "A.V. Fedorov" 2 => "O.P. Ilyinskaya" 3 => "R.A. Zinovkin" 4 => "B.V. Chernyak" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Biochemistry (Mosc)" "fecha" => "2016" "volumen" => "81" "paginaInicial" => "1564" "paginaFinal" => "1577" ] ] ] ] ] ] 18 => array:3 [ "identificador" => "bib0250" "etiqueta" => "19" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Monocytes, neutrophils, and platelets cooperate to initiate and propagate venous thrombosis in mice in vivo" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "M.L. Von Brühl" 1 => "K. Stark" 2 => "A. Steinhart" 3 => "S. Chandraratne" 4 => "I. Konrad" 5 => "M. Lorenz" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1084/jem.20112322" "Revista" => array:6 [ "tituloSerie" => "J Exp Med" "fecha" => "2012" "volumen" => "209" "paginaInicial" => "819" "paginaFinal" => "835" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/22451716" "web" => "Medline" ] ] ] ] ] ] ] ] 19 => array:3 [ "identificador" => "bib0255" "etiqueta" => "20" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Proprotein convertase subtilisin/kexin type 9 (PCSK9) deficiency is protective against venous thrombosis in mice" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "H. Wang" 1 => "Q. Wang" 2 => "J. Wang" 3 => "C. Guo" 4 => "K. Kleiman" 5 => "H. Meng" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1038/s41598-017-14307-x" "Revista" => array:5 [ "tituloSerie" => "Sci Rep" "fecha" => "2017" "volumen" => "7" "paginaInicial" => "14360" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/29084995" "web" => "Medline" ] ] ] ] ] ] ] ] 20 => array:3 [ "identificador" => "bib0260" "etiqueta" => "21" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Thrombosis: tangled up in NETs" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "K. Martinod" 1 => "D.D. Wagner" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1182/blood-2013-10-463646" "Revista" => array:6 [ "tituloSerie" => "Blood" "fecha" => "2014" "volumen" => "123" "paginaInicial" => "2768" "paginaFinal" => "2776" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/24366358" "web" => "Medline" ] ] ] ] ] ] ] ] 21 => array:3 [ "identificador" => "bib0265" "etiqueta" => "22" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Neutrophil extracellular trap (NET) impact on deep vein thrombosis" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "T.A. Fuchs" 1 => "A. Brill" 2 => "D.D. Wagner" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1161/ATVBAHA.111.242859" "Revista" => array:6 [ "tituloSerie" => "Arterioscler Thromb Vasc Biol" "fecha" => "2012" "volumen" => "32" "paginaInicial" => "1777" "paginaFinal" => "1783" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/22652600" "web" => "Medline" ] ] ] ] ] ] ] ] 22 => array:3 [ "identificador" => "bib0270" "etiqueta" => "23" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Neutrophil extracellular traps promote deep vein thrombosis in mice" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "A. Brill" 1 => "T.A. Fuchs" 2 => "A.S. Savchenko" 3 => "G.M. Thomas" 4 => "K. Martinod" 5 => "S.F. De Meyer" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "J Thromb Haemost" "fecha" => "2012" "volumen" => "10" "paginaInicial" => "136" "paginaFinal" => "144" ] ] ] ] ] ] 23 => array:3 [ "identificador" => "bib0275" "etiqueta" => "24" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Propagation of thrombosis by neutrophils and extracellular nucleosome networks" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "S. Pfeiler" 1 => "K. Stark" 2 => "S. Massberg" 3 => "B. Engelmann" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.3324/haematol.2016.142471" "Revista" => array:6 [ "tituloSerie" => "Haematologica" "fecha" => "2017" "volumen" => "102" "paginaInicial" => "206" "paginaFinal" => "213" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/27927771" "web" => "Medline" ] ] ] ] ] ] ] ] 24 => array:3 [ "identificador" => "bib0280" "etiqueta" => "25" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Divergent effects of Tlr9 deletion in experimental late venous thrombosis resolution and vein wall injury" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "N.A. Dewyer" 1 => "O.M. El-Sayed" 2 => "C.E. Luke" 3 => "M. Elfline" 4 => "N. Kittan" 5 => "R. Allen" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Thromb Haemost" "fecha" => "2015" "volumen" => "114" "paginaInicial" => "1028" "paginaFinal" => "1037" ] ] ] ] ] ] 25 => array:3 [ "identificador" => "bib0285" "etiqueta" => "26" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Role of thromboxane-dependent platelet activation in venous thrombosis: aspirin effects in mouse model" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "E. Tarantino" 1 => "P. Amadio" 2 => "I. Squellerio" 3 => "B. Porro" 4 => "L. Sandrini" 5 => "L. Turnu" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Pharmacol Res" "fecha" => "2016" "volumen" => "107" "paginaInicial" => "415" "paginaFinal" => "425" ] ] ] ] ] ] 26 => array:3 [ "identificador" => "bib0290" "etiqueta" => "27" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Systematic review on the use of aspirin in the prevention of deep vein thrombosis in major elective lower limb orthopedic surgery: an update from the past 3 years" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "D.A. Mistry" 1 => "A. Chandratreya" 2 => "P.Y.F. Lee" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Surg J (N Y)" "fecha" => "2017" "volumen" => "3" "paginaInicial" => "e191" "paginaFinal" => "e196" ] ] ] ] ] ] 27 => array:3 [ "identificador" => "bib0295" "etiqueta" => "28" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Podoplanin expression in primary brain tumors induces platelet aggregation and increases risk of venous thromboembolism" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "J. Riedl" 1 => "M. Preusser" 2 => "P.M. Nazari" 3 => "F. Posch" 4 => "S. Panzer" 5 => "C. Marosi" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Blood" "fecha" => "2017" "volumen" => "129" "paginaInicial" => "1831" "paginaFinal" => "1839" ] ] ] ] ] ] 28 => array:3 [ "identificador" => "bib0300" "etiqueta" => "29" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Initiation and perpetuation of NLRP3 inflammasome activation and assembly" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "E.I. Elliott" 1 => "F.S. Sutterwala" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1111/imr.12286" "Revista" => array:6 [ "tituloSerie" => "Immunol Rev" "fecha" => "2015" "volumen" => "265" "paginaInicial" => "35" "paginaFinal" => "52" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/25879282" "web" => "Medline" ] ] ] ] ] ] ] ] 29 => array:3 [ "identificador" => "bib0305" "etiqueta" => "30" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Myeloid-related protein-14 regulates deep vein thrombosis" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:6 [ 0 => "Y. Wang" 1 => "H. Gao" 2 => "C.W. Kessinger" 3 => "A. Schmaier" 4 => "F.A. Jaffer" 5 => "D.I. Simon" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1172/jci.insight.91356" "Revista" => array:5 [ "tituloSerie" => "JCI Insight" "fecha" => "2017" "volumen" => "2" "paginaInicial" => "91356" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/28570273" "web" => "Medline" ] ] ] ] ] ] ] ] 30 => array:3 [ "identificador" => "bib0310" "etiqueta" => "31" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Platelet amyloid precursor protein is a modulator of venous thromboembolism in mice" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "I. Canobbio" 1 => "C. Visconte" 2 => "S. Momi" 3 => "G.F. Guidetti" 4 => "M. Zarà" 5 => "J. Canino" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1182/blood-2017-01-764910" "Revista" => array:6 [ "tituloSerie" => "Blood" "fecha" => "2017" "volumen" => "130" "paginaInicial" => "527" "paginaFinal" => "536" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/28611024" "web" => "Medline" ] ] ] ] ] ] ] ] ] ] ] ] ] "idiomaDefecto" => "en" "url" => "/23870206/0000015300000002/v2_202004301535/S2387020619302323/v2_202004301535/en/main.assets" "Apartado" => array:4 [ "identificador" => "44145" "tipo" => "SECCION" "en" => array:2 [ "titulo" => "Special article" "idiomaDefecto" => true ] "idiomaDefecto" => "en" ] "PDF" => "https://static.elsevier.es/multimedia/23870206/0000015300000002/v2_202004301535/S2387020619302323/v2_202004301535/en/main.pdf?idApp=UINPBA00004N&text.app=https://www.elsevier.es/" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020619302323?idApp=UINPBA00004N" ]
Journal Information
Vol. 153. Issue 2.
Pages 78-81 (July 2019)
Share
Download PDF
More article options
Vol. 153. Issue 2.
Pages 78-81 (July 2019)
Special article
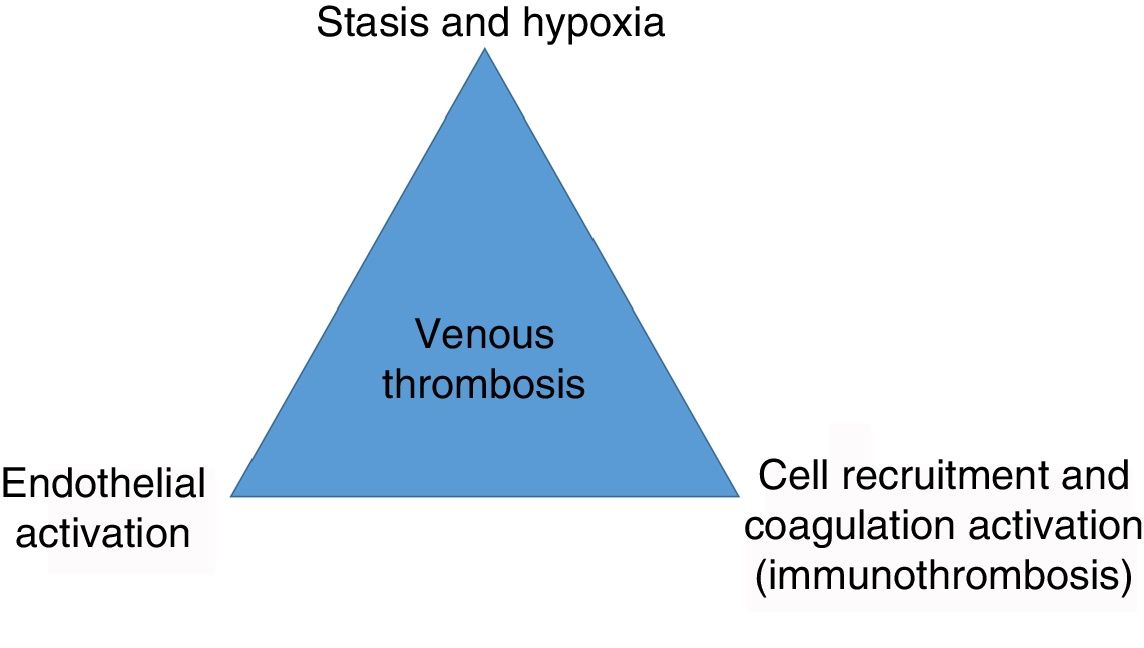
New mechanisms in venous thrombosis: Immunothrombosis
Nuevos mecanismos en la trombosis venosa: inmunotrombosis
Visits
4
This item has received
Article information
These are the options to access the full texts of the publication Medicina Clínica (English Edition)
Subscriber
Subscribe
Purchase
Contact
Phone for subscriptions and reporting of errors
From Monday to Friday from 9 a.m. to 6 p.m. (GMT + 1) except for the months of July and August which will be from 9 a.m. to 3 p.m.
Calls from Spain
932 415 960
Calls from outside Spain
+34 932 415 960
E-mail