Based on initial evidence about this pandemic, the older population and/or those with associated chronic pathology (high blood pressure, diabetes, obesity…) have been identified as being more likely to develop more severe clinical forms of the infection. Obesity as a risk factor and predictor of COVID-19 infection severity is being reported by some studies, but there is still a great lack of evidence. Even so, it has been postulated as an independent risk factor for COVID-19 since it was recognized as such during the 2009 H1N1 pandemic. Our objective is to study the relationship between obesity, the need for oxygen therapy with a reservoir (non-rebreather) mask, and the need for ICU, as well as to analyse the cardiovascular profile of patients who have required hospital admission for COVID-19 pneumonia.
A retrospective and descriptive cohort study of 49 consecutive patients admitted to the Internal Medicine hospital ward for COVID-19 infection at the Toledo Hospital Complex was conducted from 23rd March to 14th April 2020. Variables were collected on cardiovascular disease, need for a reservoir (non-rebreather) mask and admission to the ICU. According to the body mass index (BMI), overweight was defined for values from 25.0 to 29.9 kg/m2 and obesity for BMI >30.0 kg/m2.
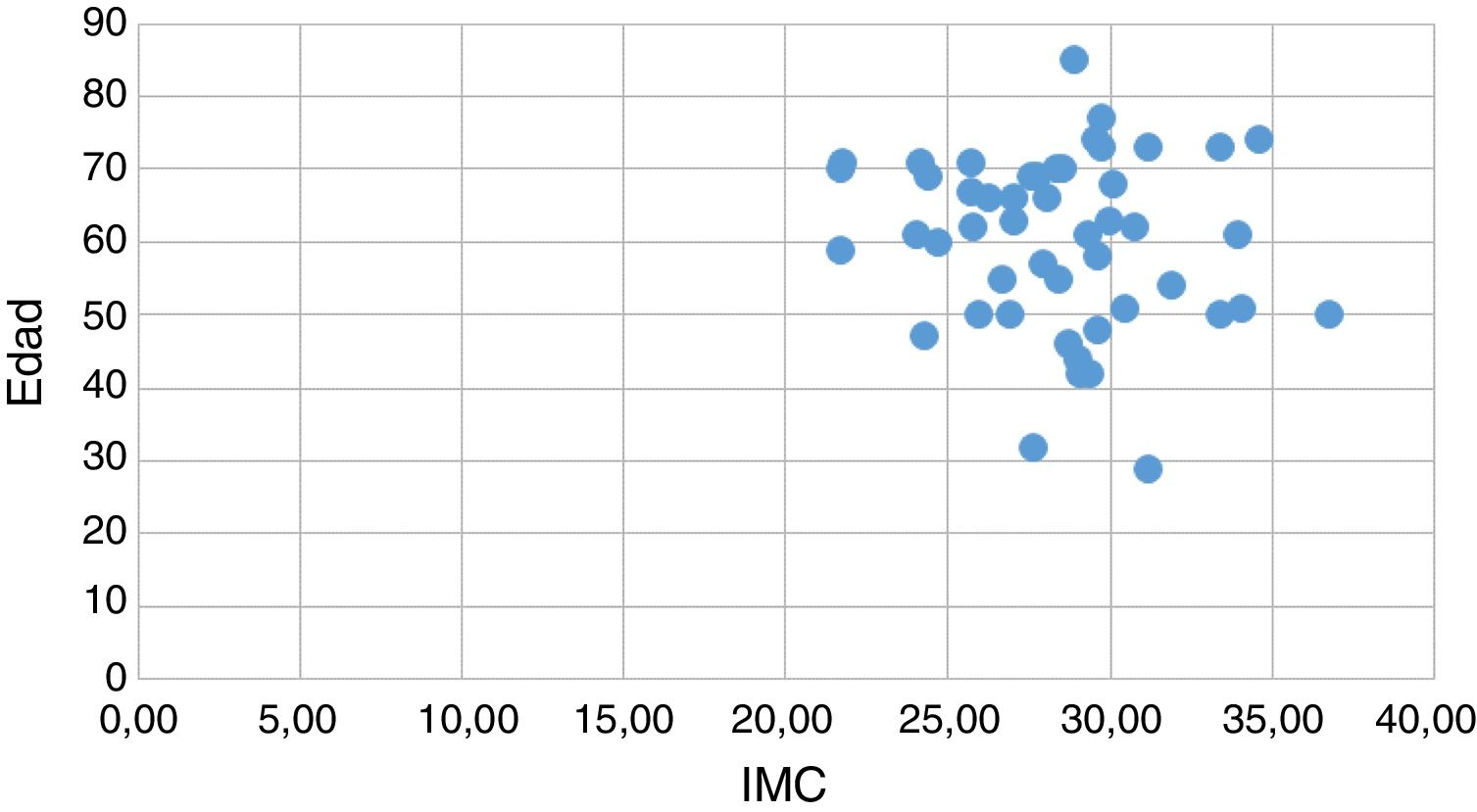
57.14% were male, the mean age was 60.30 years (SD 11.88) and the mean BMI of 28.40 kg/m2 (SD 3.34). 59.2% were overweight and 24.5% were obese. The prevalence of hypertension was 48.98%, that of dyslipidaemia was 38.78% and that of diabetes mellitus was 18.37%. 38.78% required a mask with a reservoir and 28.57% were admitted to the ICU. The mean BMI of the patients who required a reservoir mask was 28.74 kg/m2 (SD 3,169), compared to 28.19 kg/m2 (SD 3.493) in those who did not need it, resulting in a difference of 0.98, with a CI 95% between ↓2.54 and 1.43. Regarding the patients who required admission to the ICU, a mean BMI of 28.16 kg/m2 (SD 3,240) was obtained, compared to 28.50 kg/m2 (SD 3.432) of those who did not require one, resulting in a difference of 1.06, with a 95% CI between ↓1.80 and 2.49. No statistically significant relationship was obtained between the need for a reservoir mask and the variables BMI, hypertension, dyslipidaemia, and diabetes. Regarding the need for admission to the ICU, its association was statistically significant with diabetes mellitus (p = 0.037), but not with the rest of the variables analysed (multivariate analysis).
According to the literature, higher mortality has been observed in a diabetic population with COVID-19 over 65 years of age. The largest study reported from China (72,314 cases) showed an increased incidence of mortality in diabetic patients with COVID-19 (2.3% over 7.3%).1 Our study also found a significant relationship between diabetes and the need for admission to the ICU. Regarding obesity, several studies carried out in China, Italy and the United States have demonstrated that this population is more likely to be infected by the virus and more likely to develop more serious pneumonia, complications and death, as well as a greater risk of developing a more virulent strain and prolonging the time of infection to the rest of the population.2 Similar data have been obtained in France, demonstrating that a BMI ≥35 kg/m2 is an independent factor of severity in COVID-19 infection.3 However, there are conflicting results on obesity. Our sample did not show a greater need for oxygen therapy with a reservoir mask nor a greater need for ICU admission for subjects with a higher BMI, in accordance with studies such as those by Li et al. and Qingxian et al., that do not establish a link between obesity and the severity of COVID-19 pneumonia.4,5 A limitation of this study is the high prevalence of overweight in the population under study, which provides us with a very homogeneous sample with little dispersion (BMI 28.40 kg/m2 [SD 3.34]) (Fig. 1) and that can lead to contradictory findings.
To conclude, this study has not been able to establish obesity as a factor influencing COVID-19 infection, in terms of requiring admission to the ICU and/or the need for oxygen therapy supplementation with a reservoir (non-rebreather) mask, but an association between diabetes and admission to the ICU has been demonstrated.
FundingThis research has not received specific support from public sector agencies, the commercial sector, or non-profit organisations.
Conflict of interestsThe authors declare no conflict of interest.
We wish to thank all front-line health personnel, for their work, dedication, and sacrifice. Also, Pedro Beneyto Martín and J. Puentes Gutiérrez for their methodological support.
Please cite this article as: Fernández García L, Puentes Gutiérrez AB, García Bascones M. Relación entre obesidad, diabetes e ingreso en UCI en pacientes COVID-19. Med Clin (Barc). 2020;155:314–315.