Critical patients, despite initial recovery in the intensive care unit (ICU), may require readmission to the ICU or even die in the same hospital episode. The objectives are to determine the incidence and to identify risk factors for ICU readmission, and to determine hospital mortality.
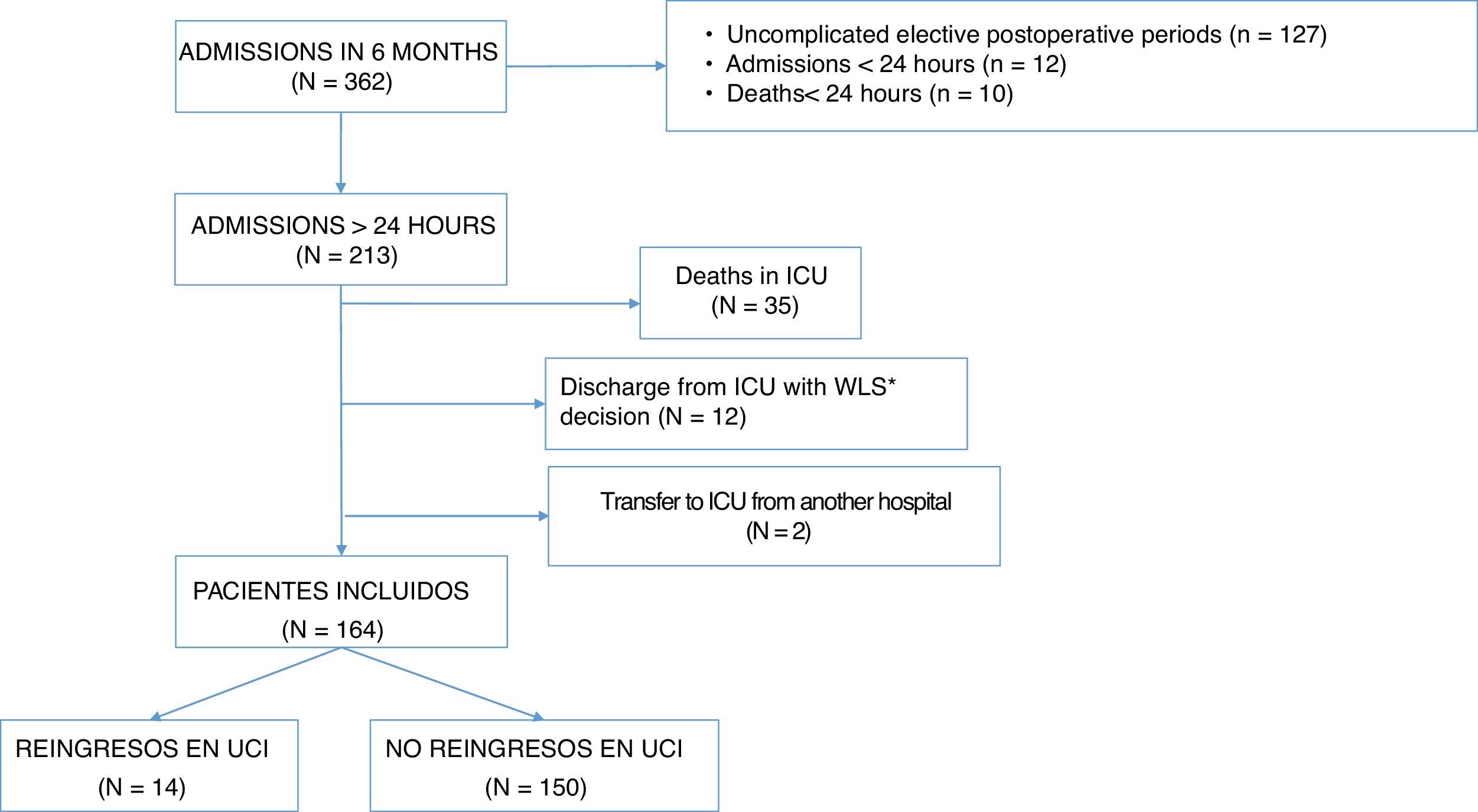
MethodsObservational cohort study of all patients admitted consecutively for more than 24 h to the ICU of the University Hospital of Getafe between April 1, 2018 and September 30, 2018 and discharged alive from their first ICU admission.
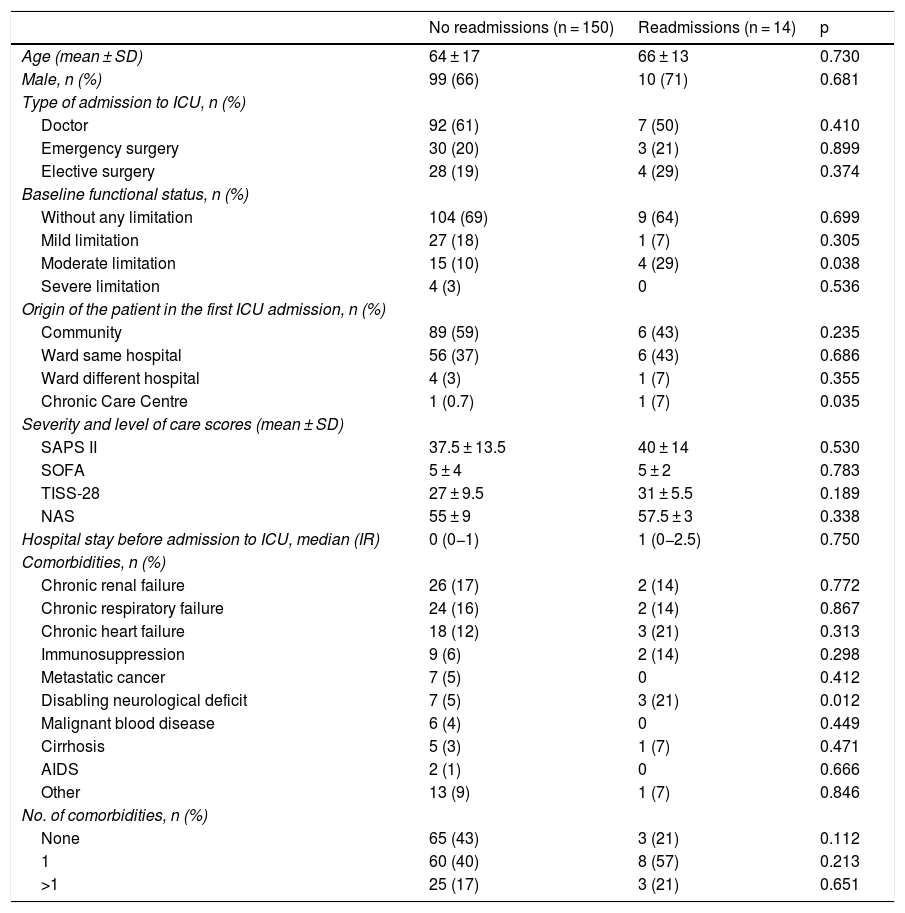
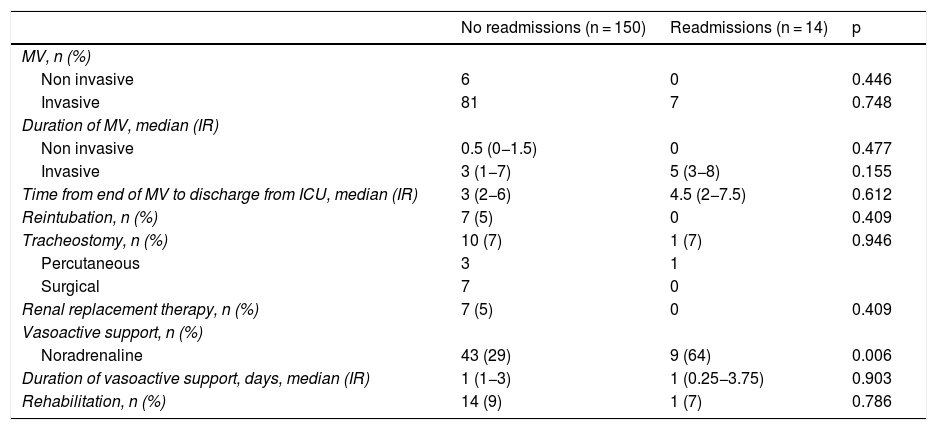
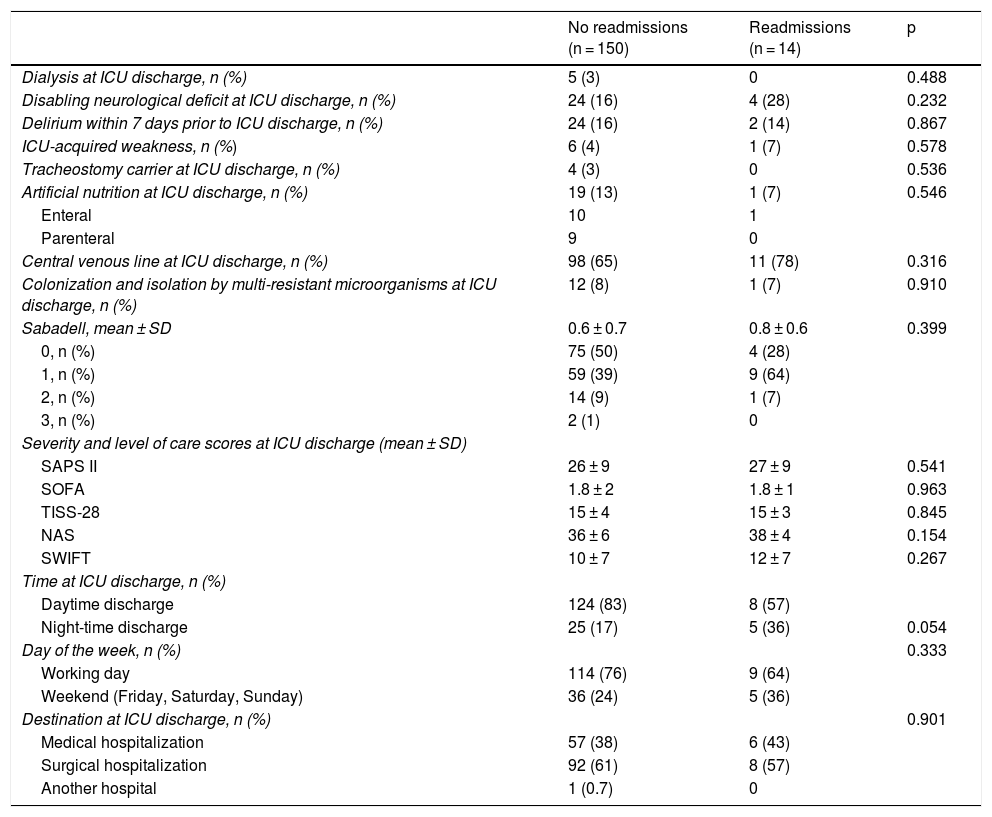
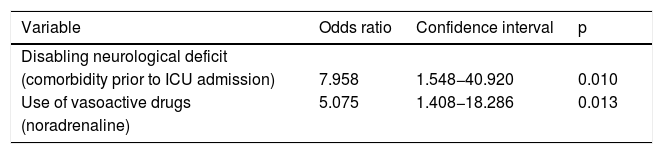
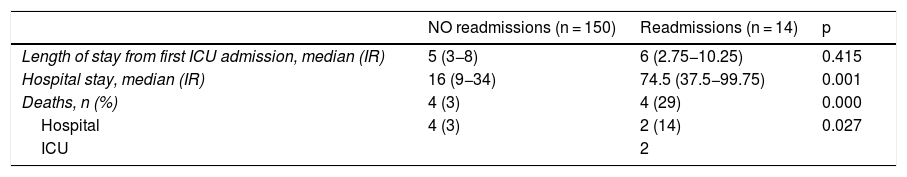
ResultsOf the 164 patients alive at ICU discharge, 14 (8.5%) were readmitted to ICU (2.4% at ≤48 h). The adjusted risk of ICU readmission was higher in patients with disabling neurological deficits prior to ICU admission [odds ratio (OR) 7.96, 95% confidence interval (CI) 1.55–40.92] or who received vasoactive drugs (OR 5.07, 95% CI 1.41–18.29) during their ICU stay. Readmitted patients had higher hospital mortality (4 of 14 [29%] versus 5 of 150 [3%], P < 0.001) and longer hospital stay (74.5 [37.5−99.75] days versus 16 [9−34] days, median [interquartile range], P = 0.001).
ConclusionsPatients with disabling neurological deficits prior to hospital admission or who received vasoactive drugs during their ICU stay have a higher risk of readmission to the ICU, which increases hospital stay and mortality.
Los pacientes críticos, a pesar de la recuperación inicial en la unidad de cuidados intensivos (UCI), pueden precisar reingreso en UCI o incluso fallecer en el mismo episodio hospitalario. Los objetivos son: conocer la incidencia e identificar factores de riesgo de reingreso en UCI, y determinar la mortalidad hospitalaria.
MétodosEstudio de cohortes observacional de todos los pacientes ingresados consecutivamente más de 24 h en la UCI del Hospital Universitario de Getafe entre el 1-04-2018 y el 30-09-2018 y dados de alta vivos de su primer ingreso en UCI.
ResultadosDe los 164 pacientes vivos al alta de UCI, 14 (8,5%) fueron reingresados en UCI (2,4% en ≤ 48 h). El riesgo ajustado de reingreso en UCI fue mayor en los pacientes con déficit neurológico discapacitante previo al ingreso en UCI (odds ratio [OR]: 7,96; intervalo de confianza del 95% [IC 95%]: 1,55−40,92) o que recibieron fármacos vasoactivos (OR: 5,07; IC 95%: 1,41−18,29) durante su estancia en UCI. Los pacientes reingresados tuvieron mayor mortalidad hospitalaria (4 de 14 [29%] versus 5 de 150 [3%], p < 0,001) y mayor estancia hospitalaria (74,5 [37,5–99,75] días versus 16 [9−34] días, mediana [rango intercuartílico], p = 0,001).
ConclusionesLos pacientes con déficit neurológico discapacitante previo al ingreso hospitalario o que recibieron fármacos vasoactivos durante la estancia en UCI tienen mayor riesgo de reingreso en UCI, lo que aumenta la estancia y la mortalidad hospitalaria.