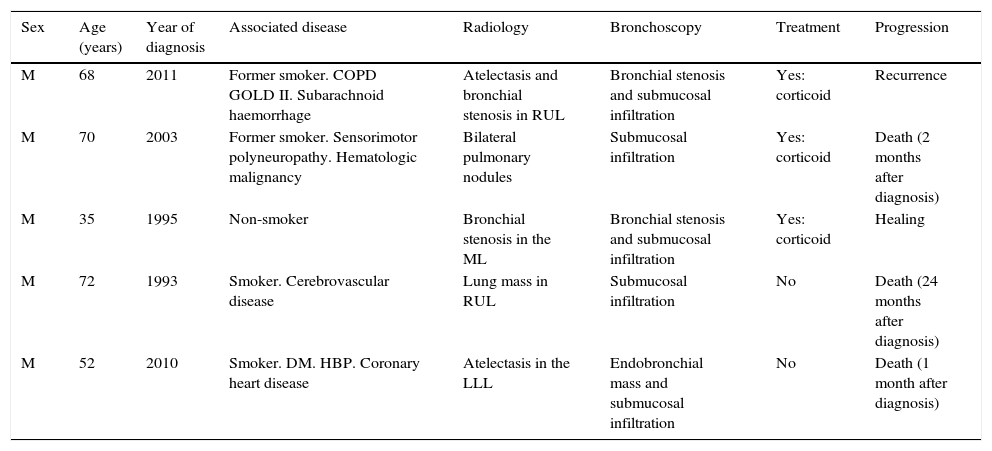
array:24 [ "pii" => "S2387020616002102" "issn" => "23870206" "doi" => "10.1016/j.medcle.2016.03.020" "estado" => "S300" "fechaPublicacion" => "2015-11-20" "aid" => "3251" "copyright" => "Elsevier España, S.L.U.. All rights reserved" "copyrightAnyo" => "2015" "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2015;145:460-2" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "Traduccion" => array:1 [ "es" => array:19 [ "pii" => "S0025775315001098" "issn" => "00257753" "doi" => "10.1016/j.medcli.2015.01.024" "estado" => "S300" "fechaPublicacion" => "2015-11-20" "aid" => "3251" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2015;145:460-2" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:2 [ "total" => 13 "formatos" => array:2 [ "HTML" => 7 "PDF" => 6 ] ] "es" => array:10 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Carta al Editor</span>" "titulo" => "Amiloidosis traqueobronquial: diagnóstico, tratamiento y evolución en 5 casos" "tienePdf" => "es" "tieneTextoCompleto" => "es" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "460" "paginaFinal" => "462" ] ] "titulosAlternativos" => array:1 [ "en" => array:1 [ "titulo" => "Tracheobronchial amyloidosis: Diagnosis, treatment and evolution in 5 patients" ] ] "contieneTextoCompleto" => array:1 [ "es" => true ] "contienePdf" => array:1 [ "es" => true ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Ana Pando Sandoval, Miguel Angel Ariza Prota, Marta García Clemente, Pere Casan" "autores" => array:4 [ 0 => array:2 [ "nombre" => "Ana" "apellidos" => "Pando Sandoval" ] 1 => array:2 [ "nombre" => "Miguel Angel" "apellidos" => "Ariza Prota" ] 2 => array:2 [ "nombre" => "Marta" "apellidos" => "García Clemente" ] 3 => array:2 [ "nombre" => "Pere" "apellidos" => "Casan" ] ] ] ] ] "idiomaDefecto" => "es" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S2387020616002102" "doi" => "10.1016/j.medcle.2016.03.020" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020616002102?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775315001098?idApp=UINPBA00004N" "url" => "/00257753/0000014500000010/v1_201510290045/S0025775315001098/v1_201510290045/es/main.assets" ] ] "itemSiguiente" => array:19 [ "pii" => "S2387020616002114" "issn" => "23870206" "doi" => "10.1016/j.medcle.2015.01.002" "estado" => "S300" "fechaPublicacion" => "2015-11-20" "aid" => "3242" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2015;145:462-3" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:2 [ "total" => 1 "HTML" => 1 ] "en" => array:10 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Neuralgic amyotrophy associated to hepatitis E virus infection" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "462" "paginaFinal" => "463" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Neuralgia amiotrófica en relación con infección por el virus de la hepatitis E" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Laura Martínez Rodríguez, Paula Carvajal, Germán Morís" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Laura" "apellidos" => "Martínez Rodríguez" ] 1 => array:2 [ "nombre" => "Paula" "apellidos" => "Carvajal" ] 2 => array:2 [ "nombre" => "Germán" "apellidos" => "Morís" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0025775315000846" "doi" => "10.1016/j.medcli.2015.01.021" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775315000846?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020616002114?idApp=UINPBA00004N" "url" => "/23870206/0000014500000010/v1_201604230100/S2387020616002114/v1_201604230100/en/main.assets" ] "itemAnterior" => array:19 [ "pii" => "S2387020616002096" "issn" => "23870206" "doi" => "10.1016/j.medcle.2016.03.019" "estado" => "S300" "fechaPublicacion" => "2015-11-20" "aid" => "3257" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2015;145:459-60" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:10 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "First case of bacteremia by <span class="elsevierStyleItalic">Sphingomonas anadarae</span> in a patient with cancer" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "459" "paginaFinal" => "460" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Primer caso de bacteriemia por <span class="elsevierStyleItalic">Sphingomonas anadarae</span> en un paciente con cáncer" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Tomás García-Lozano, Ana M. García-García, Agustín Iranzo-Tatay, Eduardo Aznar-Oroval" "autores" => array:4 [ 0 => array:2 [ "nombre" => "Tomás" "apellidos" => "García-Lozano" ] 1 => array:2 [ "nombre" => "Ana M." "apellidos" => "García-García" ] 2 => array:2 [ "nombre" => "Agustín" "apellidos" => "Iranzo-Tatay" ] 3 => array:2 [ "nombre" => "Eduardo" "apellidos" => "Aznar-Oroval" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0025775315001153" "doi" => "10.1016/j.medcli.2015.01.026" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775315001153?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020616002096?idApp=UINPBA00004N" "url" => "/23870206/0000014500000010/v1_201604230100/S2387020616002096/v1_201604230100/en/main.assets" ] "en" => array:15 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Tracheobronchial amyloidosis: Diagnosis, treatment and evolution in 5 patients" "tieneTextoCompleto" => true "saludo" => "<span class="elsevierStyleItalic">Dear Editor</span>," "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "460" "paginaFinal" => "462" ] ] "autores" => array:1 [ 0 => array:4 [ "autoresLista" => "Ana Pando Sandoval, Miguel Angel Ariza Prota, Marta García Clemente, Pere Casan" "autores" => array:4 [ 0 => array:4 [ "nombre" => "Ana" "apellidos" => "Pando Sandoval" "email" => array:1 [ 0 => "ana_pando@hotmail.com" ] "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">*</span>" "identificador" => "cor0005" ] ] ] 1 => array:2 [ "nombre" => "Miguel Angel" "apellidos" => "Ariza Prota" ] 2 => array:2 [ "nombre" => "Marta" "apellidos" => "García Clemente" ] 3 => array:2 [ "nombre" => "Pere" "apellidos" => "Casan" ] ] "afiliaciones" => array:1 [ 0 => array:2 [ "entidad" => "Área del Pulmón, Instituto Nacional de Silicosis (INS), Hospital Universitario Central de Asturias (HUCA), Facultad de Medicina, Universidad de Oviedo, Oviedo, Asturias, Spain" "identificador" => "aff0005" ] ] "correspondencia" => array:1 [ 0 => array:3 [ "identificador" => "cor0005" "etiqueta" => "⁎" "correspondencia" => "Corresponding author." ] ] ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Amiloidosis traqueobronquial: diagnóstico, tratamiento y evolución en 5 casos" ] ] "textoCompleto" => "<span class="elsevierStyleSections"><p id="par0005" class="elsevierStylePara elsevierViewall">Amyloidosis includes a group of conditions characterized by the deposition in different tissues of a protein of insoluble fibrillary structure called amyloid, in an amount sufficient to impair normal function of the affected tissue.<a class="elsevierStyleCrossRefs" href="#bib0055"><span class="elsevierStyleSup">1,2</span></a> The disease can be inherited or acquired and may be systemic or localized. Virchow first described pulmonary involvement of amyloidosis in 1875.<a class="elsevierStyleCrossRef" href="#bib0065"><span class="elsevierStyleSup">3</span></a> The most common types of amyloid proteins are primary (AL) and secondary (AA). AL amyloidosis mainly affects the upper respiratory, urogenital and gastrointestinal tracts, and the skin.<a class="elsevierStyleCrossRef" href="#bib0055"><span class="elsevierStyleSup">1</span></a> It usually affects patients between the fourth and fifth decades of life. Some individuals remain asymptomatic, while others present symptoms; in some cases, the disorder can be severe and even life-threatening.<a class="elsevierStyleCrossRefs" href="#bib0070"><span class="elsevierStyleSup">4–8</span></a> Next, we describe a series of 5 cases of tracheobronchial amyloidosis.</p><p id="par0010" class="elsevierStylePara elsevierViewall">Our objective was to analyze the symptoms and describe the radiological findings, treatment guidelines and progression of patients with tracheobronchial amyloidosis. We conducted a retrospective study of patients diagnosed with tracheobronchial amyloidosis from January 1993 to January 2013 in our hospital. The variables studied were: age, sex, associated diseases, smoking and drinking habits, symptoms, radiological and endobronchial alterations, treatment and progression. During the study period, 5 patients were diagnosed with tracheobronchial amyloidosis. All of them were male, with an average age of 59<span class="elsevierStyleHsp" style=""></span>±<span class="elsevierStyleHsp" style=""></span>15 years. Two were smokers (40%), and other 2 former smokers (40%). Among the associated diseases we found a patient with COPD, another with diabetes mellitus, another with hypertension, another with coronary heart disease, 3 with neurological disease and one with hematologic malignancy. Charlson index was 1.4<span class="elsevierStyleHsp" style=""></span>±<span class="elsevierStyleHsp" style=""></span>2. Two patients had a previous episode of pneumonia. The main symptoms were cough in 4 patients (80%), dyspnoea in 3 (60%), expectoration in one (20%), asthenia in another (20%) and weight loss in another (20%). The average time of symptoms progression was 6 months (5.6), with an average of 0.4 visits to the emergency room in the previous year (0–2). The initial clinical suspicion after evaluating the patient was neoplasm in 3 cases (60%), and infectious processes in the remaining 2 (40%). The radiographic findings from computed tomography (CT) showed the presence of bronchial stenosis, atelectasis, pulmonary nodules or pulmonary masses. All patients underwent bronchoscopy, which showed submucosal infiltration (100%), bronchial stenosis (40%) and/or endobronchial mass (20%), and one patient underwent CT-guided core needle biopsy. The diagnosis was obtained by bronchial biopsy in 4 patients (80%) and by CT-guided core needle biopsy in one (20%), with a compatible histological diagnosis. 3 patients were treated with corticosteroids (60%), one of them presented local recurrence (25 months after diagnosis and 7 months after completion of treatment). Of the 2 patients who did not receive treatment, one was not treated because of being asymptomatic and the other died before undergoing surgery. During the progression, 2 more patients died of other medical causes. The main features of the series described in <a class="elsevierStyleCrossRef" href="#tbl0005">Table 1</a>.</p><elsevierMultimedia ident="tbl0005"></elsevierMultimedia><p id="par0015" class="elsevierStylePara elsevierViewall">Tracheobronchial amyloidosis is a rare form of amyloidosis, and is characterized by submucosal amyloid deposits in the trachea and main and segmental bronchi and/or polypoid tumours in the airways.<a class="elsevierStyleCrossRefs" href="#bib0070"><span class="elsevierStyleSup">4,5,9</span></a> The endobronchial form is not associated with systemic amyloidosis.<a class="elsevierStyleCrossRefs" href="#bib0070"><span class="elsevierStyleSup">4–6</span></a> It is a slow progression disease that requires diagnostic tests for histopathologic confirmation with Congo Red staining, which remains the <span class="elsevierStyleItalic">gold standard</span>.<a class="elsevierStyleCrossRef" href="#bib0100"><span class="elsevierStyleSup">10</span></a> In our series we present 5 cases of tracheobronchial amyloidosis, one combines tracheobronchial involvement with bilateral nodular involvement. This entity is a rare condition and represents 0.5% of symptomatic tracheobronchial lesions. Different imaging techniques have been used for disease diagnosing, mainly CT scan, but also a more novel way, PET-CT scan, where the amyloid material exhibits intense uptake of 18-fluorodeoxyglucose and is useful for monitoring patients, since it allows assessing the degree of disease activity. A histopathologic examination is required in order to establish the diagnosis of the disease, which in the case of tracheobronchial amyloidosis, is usually obtained by bronchoscopy. Although an effective treatment for pulmonary amyloidosis has not described, the Nd:YAG laser or cryotherapy has been used to treat bronchial obstructions by amyloid deposition, prosthesis and local external radiotherapy. In systemic involvement, increased survival has been demonstrated with dexamethasone or a combination of prednisone and melphalan. The prognosis in lung involvement is better than the systemic condition. In the study by Utz et al.,<a class="elsevierStyleCrossRef" href="#bib0065"><span class="elsevierStyleSup">3</span></a> the median survival was 16 months. In our series, 3 patients died, one after 1 month of diagnosis, before surgery, and 2 patients at 2 and 24 months, respectively, after diagnosis due to various medical causes. The main causes of death associated with tracheobronchial amyloidosis are massive haemoptysis and respiratory failure.</p><span id="sec0005" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0005">Conflict of interests</span><p id="par0020" class="elsevierStylePara elsevierViewall">There are no opposing conflicts or conflicts of interest to declare.</p></span></span>" "textoCompletoSecciones" => array:1 [ "secciones" => array:2 [ 0 => array:2 [ "identificador" => "sec0005" "titulo" => "Conflict of interests" ] 1 => array:1 [ "titulo" => "References" ] ] ] "pdfFichero" => "main.pdf" "tienePdf" => true "NotaPie" => array:1 [ 0 => array:2 [ "etiqueta" => "☆" "nota" => "<p class="elsevierStyleNotepara" id="npar0005">Please cite this article as: Pando Sandoval A, Ariza Prota MA, García Clemente M, Casan P. Amiloidosis traqueobronquial: diagnóstico, tratamiento y evolución en 5 casos. Med Clin (Barc). 2015;145:460–462.</p>" ] ] "multimedia" => array:1 [ 0 => array:8 [ "identificador" => "tbl0005" "etiqueta" => "Table 1" "tipo" => "MULTIMEDIATABLA" "mostrarFloat" => true "mostrarDisplay" => false "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at1" "detalle" => "Table " "rol" => "short" ] ] "tabla" => array:2 [ "leyenda" => "<p id="spar0010" class="elsevierStyleSimplePara elsevierViewall">DM, diabetes mellitus; COPD, chronic obstructive pulmonary disease; GOLD, <span class="elsevierStyleItalic">the Global Initiative for Chronic Obstructive Lung Disease</span>; HBP, high blood pressure; LLL, left lower lobe; ML, middle lobe; RUL, right upper lobe; M, male.</p>" "tablatextoimagen" => array:1 [ 0 => array:2 [ "tabla" => array:1 [ 0 => """ <table border="0" frame="\n \t\t\t\t\tvoid\n \t\t\t\t" class=""><thead title="thead"><tr title="table-row"><th class="td" title="table-head " align="left" valign="top" scope="col" style="border-bottom: 2px solid black">Sex \t\t\t\t\t\t\n \t\t\t\t</th><th class="td" title="table-head " align="left" valign="top" scope="col" style="border-bottom: 2px solid black">Age (years) \t\t\t\t\t\t\n \t\t\t\t</th><th class="td" title="table-head " align="left" valign="top" scope="col" style="border-bottom: 2px solid black">Year of diagnosis \t\t\t\t\t\t\n \t\t\t\t</th><th class="td" title="table-head " align="left" valign="top" scope="col" style="border-bottom: 2px solid black">Associated disease \t\t\t\t\t\t\n \t\t\t\t</th><th class="td" title="table-head " align="left" valign="top" scope="col" style="border-bottom: 2px solid black">Radiology \t\t\t\t\t\t\n \t\t\t\t</th><th class="td" title="table-head " align="left" valign="top" scope="col" style="border-bottom: 2px solid black">Bronchoscopy \t\t\t\t\t\t\n \t\t\t\t</th><th class="td" title="table-head " align="left" valign="top" scope="col" style="border-bottom: 2px solid black">Treatment \t\t\t\t\t\t\n \t\t\t\t</th><th class="td" title="table-head " align="left" valign="top" scope="col" style="border-bottom: 2px solid black">Progression \t\t\t\t\t\t\n \t\t\t\t</th></tr></thead><tbody title="tbody"><tr title="table-row"><td class="td-with-role" title="table-entry ; entry_with_role_rowhead " align="left" valign="top">M \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">68 \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">2011 \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Former smoker. COPD GOLD II. Subarachnoid haemorrhage \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Atelectasis and bronchial stenosis in RUL \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Bronchial stenosis and submucosal infiltration \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Yes: corticoid \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Recurrence \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="table-entry ; entry_with_role_rowhead " align="left" valign="top">M \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">70 \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">2003 \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Former smoker. Sensorimotor polyneuropathy. Hematologic malignancy \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Bilateral pulmonary nodules \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Submucosal infiltration \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Yes: corticoid \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Death (2 months after diagnosis) \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="table-entry ; entry_with_role_rowhead " align="left" valign="top">M \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">35 \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">1995 \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Non-smoker \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Bronchial stenosis in the ML \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Bronchial stenosis and submucosal infiltration \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Yes: corticoid \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Healing \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="table-entry ; entry_with_role_rowhead " align="left" valign="top">M \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">72 \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">1993 \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Smoker. Cerebrovascular disease \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Lung mass in RUL \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Submucosal infiltration \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">No \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Death (24 months after diagnosis) \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="table-entry ; entry_with_role_rowhead " align="left" valign="top">M \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">52 \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">2010 \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Smoker. DM. HBP. Coronary heart disease \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Atelectasis in the LLL \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Endobronchial mass and submucosal infiltration \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">No \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="table-entry " align="left" valign="top">Death (1 month after diagnosis) \t\t\t\t\t\t\n \t\t\t\t</td></tr></tbody></table> """ ] "imagenFichero" => array:1 [ 0 => "xTab1034948.png" ] ] ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Main characteristics of the series.</p>" ] ] ] "bibliografia" => array:2 [ "titulo" => "References" "seccion" => array:1 [ 0 => array:2 [ "identificador" => "bibs0005" "bibliografiaReferencia" => array:10 [ 0 => array:3 [ "identificador" => "bib0055" "etiqueta" => "1" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Amyloidosis" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:1 [ 0 => "M.B. Pepys" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "LibroEditado" => array:4 [ "titulo" => "Oxford textbook of medicine" "paginaInicial" => "1512" "paginaFinal" => "1524" "serieFecha" => "1995" ] ] ] ] ] ] 1 => array:3 [ "identificador" => "bib0060" "etiqueta" => "2" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Amyloidosis and the respiratory tract" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "A.E. Tattersfield" 1 => "J.D. Gillmore" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "Thorax" "fecha" => "1999" "volumen" => "54" "paginaInicial" => "444" "paginaFinal" => "451" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/10212113" "web" => "Medline" ] ] ] ] ] ] ] ] 2 => array:3 [ "identificador" => "bib0065" "etiqueta" => "3" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Pulmonary amyloidosis: the Mayo Clinic experience from 1980–1993" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "J.P. Utz" 1 => "S.J. Swensen" 2 => "M.A. Gertz" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "Ann Intern Med" "fecha" => "1996" "volumen" => "124" "paginaInicial" => "407" "paginaFinal" => "413" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/8554249" "web" => "Medline" ] ] ] ] ] ] ] ] 3 => array:3 [ "identificador" => "bib0070" "etiqueta" => "4" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Amyloidosis presenting in the lower respiratory tract" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "A.N. Hui" 1 => "M.N. Koss" 2 => "L. Hochholzer" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "Arch Pathol Lab Med" "fecha" => "1986" "volumen" => "110" "paginaInicial" => "212" "paginaFinal" => "218" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/3753854" "web" => "Medline" ] ] ] ] ] ] ] ] 4 => array:3 [ "identificador" => "bib0075" "etiqueta" => "5" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Amyloidosis of the tracheobronchial tree" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "J.F. Cordier" 1 => "R. Loire" 2 => "J. Brune" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1056/NEJM196203222661204" "Revista" => array:6 [ "tituloSerie" => "N Engl J Med" "fecha" => "1962" "volumen" => "266" "paginaInicial" => "587" "paginaFinal" => "591" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/14453403" "web" => "Medline" ] ] ] ] ] ] ] ] 5 => array:3 [ "identificador" => "bib0080" "etiqueta" => "6" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Localized amyloidosis of central airways" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "W. Petermann" 1 => "J. Barth" 2 => "E. Schluter" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "Eur J Respir Dis" "fecha" => "1987" "volumen" => "71" "paginaInicial" => "210" "paginaFinal" => "212" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/3678423" "web" => "Medline" ] ] ] ] ] ] ] ] 6 => array:3 [ "identificador" => "bib0085" "etiqueta" => "7" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Amyloid and the lower respiratory tract" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "P.J. Thompson" 1 => "K.M. Citron" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "Thorax" "fecha" => "1983" "volumen" => "38" "paginaInicial" => "84" "paginaFinal" => "87" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/6344311" "web" => "Medline" ] ] ] ] ] ] ] ] 7 => array:3 [ "identificador" => "bib0090" "etiqueta" => "8" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Amyloid tumor of the trachea and the lung, resembling bronchial asthma" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "K. Shinoi" 1 => "Y. Shiraishi" 2 => "J.I. Yahata" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "Dis Chest" "fecha" => "1962" "volumen" => "42" "paginaInicial" => "442" "paginaFinal" => "445" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/13977343" "web" => "Medline" ] ] ] ] ] ] ] ] 8 => array:3 [ "identificador" => "bib0095" "etiqueta" => "9" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Cough and persistent wheeze with long-standing asthma" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:5 [ 0 => "H.C. Chew" 1 => "S.Y. Low" 2 => "P. Eng" 3 => "T. Agasthian" 4 => "F.K. Cheah" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1378/chest.06-2810" "Revista" => array:6 [ "tituloSerie" => "Chest" "fecha" => "2007" "volumen" => "132" "paginaInicial" => "727" "paginaFinal" => "731" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/17699149" "web" => "Medline" ] ] ] ] ] ] ] ] 9 => array:3 [ "identificador" => "bib0100" "etiqueta" => "10" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "On the binding of Congo red by amyloid" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "H. Puchtler" 1 => "F. Sweat" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "J Histochem Cytochem" "fecha" => "1962" "volumen" => "10" "paginaInicial" => "355" "paginaFinal" => "364" ] ] ] ] ] ] ] ] ] ] ] "idiomaDefecto" => "en" "url" => "/23870206/0000014500000010/v1_201604230100/S2387020616002102/v1_201604230100/en/main.assets" "Apartado" => array:4 [ "identificador" => "43309" "tipo" => "SECCION" "en" => array:2 [ "titulo" => "Letters to the Editor" "idiomaDefecto" => true ] "idiomaDefecto" => "en" ] "PDF" => "https://static.elsevier.es/multimedia/23870206/0000014500000010/v1_201604230100/S2387020616002102/v1_201604230100/en/main.pdf?idApp=UINPBA00004N&text.app=https://www.elsevier.es/" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020616002102?idApp=UINPBA00004N" ]
Journal Information
Vol. 145. Issue 10.
Pages 460-462 (November 2015)
Share
Download PDF
More article options
Vol. 145. Issue 10.
Pages 460-462 (November 2015)
Letter to the Editor
Tracheobronchial amyloidosis: Diagnosis, treatment and evolution in 5 patients
Amiloidosis traqueobronquial: diagnóstico, tratamiento y evolución en 5 casos
Ana Pando Sandoval
, Miguel Angel Ariza Prota, Marta García Clemente, Pere Casan
Corresponding author
Área del Pulmón, Instituto Nacional de Silicosis (INS), Hospital Universitario Central de Asturias (HUCA), Facultad de Medicina, Universidad de Oviedo, Oviedo, Asturias, Spain
Article information
These are the options to access the full texts of the publication Medicina Clínica (English Edition)
Subscriber
Subscribe
Purchase
Contact
Phone for subscriptions and reporting of errors
From Monday to Friday from 9 a.m. to 6 p.m. (GMT + 1) except for the months of July and August which will be from 9 a.m. to 3 p.m.
Calls from Spain
932 415 960
Calls from outside Spain
+34 932 415 960
E-mail