Objectives: To describe the frequency of feared discrimination in various social situations and of perceived discrimination in clinical settings, as well as to study the relationship between discrimination and depression and anger in women living with human immunodeficiency virus (HIV).
Material and methods: The scale of Feared and Perceived Discrimination for Women with HIV (DTP-40-MV), the Beck Depression Inventory (BDI-2), and the Anger Expression scale of State-Trait-anger expression inventory (STAXI-2-AX/EX) were applied to a random sample of 200 women living with HIV.
Results: These women feared being discriminated against, perceived discrimination upon the review of medical records, but perceived little discrimination in clinical care. A model with good adjustment to the data showed that the fear of being discriminated against creates a disposition toward perception of discrimination in the clinical settings (latent variable with 2 indicators: review of the medical records and clinical care) and increases cognitive/affective depressive symptoms; higher anger control decreases the anger manifestation; greater discrimination perceived in the clinical settings decreases anger control, which facilitates the expression of anger and slows cognitive/affective depressive symptoms; and these latter symptoms sensitize the perception of discrimination before the clinical records.
Conclusion: Feared discrimination is a clinically relevant aspect due to its frequency and effect on depressive symptoms and perception of discrimination before the review of medical records.
Introduction
Human immunodeficiency virus (HIV) infection is a chronic degenerative disease which has a life expectancy of over 40 years if detected early, and with an uninterrupted adherence to an antiretroviral treatment under medical supervision. Nowadays, HIV infection eventually evolves into a very advanced immunodeficiency stage, in which the organism undergoes other diseases as a result of the body's low immunological competence such as Pneumocystis jiroveci pneumonia or Kaposi's sarcoma.1 When first diagnosed as HIV-seropositive, the patient is faced with a death prognosis, as well as a lifetime of expensive treatments with side effects. Additionally, there is the social stigma involved with the diagnosis. HIV infection diagnosis is associated with morally-condemned behaviours such as men having sex with men, having multiple and concurrent sex partners, commercial sex, and intravenous drug use.2
In recent years, HIV infection risk factors have shifted, gaining ground amongst heterosexual transmission.3 in 2013, females represented half of the cases worldwide (17.7 million out of the 35.3 million infected people are women); as known, in the past the epidemic was found predominantly in males.4 in Mexico, the ratio of female cases has increased since 1983; however, cases are still mostly found in males.3
From 1983 to 2012, 18% of the cases corresponded to women and 82% to men.5 in 2013, in Nuevo Leon, Mexico the number of HIV-seropositive people was 4,938 with a male:female ratio of 7 to 1.5
Discrimination and stigmatization against people living with HIV and those around them is one of this infectious diseases' negative consequences, and a major obstacle in prevention and assistance.6 Oftentimes people with HIV are ostracized by their families as well as their communities;7 they are subjected to social and institutional discrimination, and on occasion even denied access to healthcare, insurance coverage, entry to some countries, and access to job opportunities.8 Fear of discrimination makes people avoid detection tests, which impedes early treatment.9
Depression is twice as common in people with HIV compared to the general population.10 Discrimination contributes to depression, especially in women.11 We must point out that most people experience anger when discriminated against as they feel their rights are being infringed upon. If discrimination persists and intensifies, it usually leads to helplessness and depression; however, there are people who do not react with anger but go straight to depression due to a personal history of helplessness.12
Anger, especially uncontrolled anger, can have a negative effect in medical attention as well as in the provider-patient relationship, possibly acting as a cause of discrimination. On the other hand, its assertive expression can increase awareness and a possible rectification of the injustice suffered.13 it is exactly this complaint of discrimination from HIV seropositive patients which is the most frequent in the clinical field, in which there is a great sensitivity to the patients' rigths.14
Even though there are studies that consider depression and anger as a response to discrimination against HIV- seropositive patients,15,16 these studies do not distinguish between discrimination feared (expectations) and discrimination perceived (experienced); besides, all of these studies have been conducted outside of Mexico. Therefore, the objective of the present investigation is to describe the frequency of feared discrimination in different social situations, and perceived discrimination in clinical settings against HIV-seropositive women, as well as to study the relationship between discrimination, depression, and anger in women living with HIV, in which anger and depression are consequences of discrimination.11,12,15,16 anger management increases depressive symptoms, and the manifestation of anger decreases them.13,17
Methods and materials
The population of our study consisted of women diagnosed as HIV-positive getting medical attention in Nuevo Leon. The inclusion criteria were: being 18 years or older, knowing how to read and write, and signing a consent form before 2 witnesses.18 exclusion criteria were the presence of symptoms impeding a proper comprehension and focus on the questionnaire.
We took into consideration the recommendations made by the american Psychological association for conducting research with human participants,19 thus we provided each participant with information on the purpose of the study, guaranteed confidentiality of their information, and requested a signed consent form.
Considering that 60% of a population of 576 cases of women with HIV reported in Nuevo Leon during 20095 suffered discrimination,20 with a 95% confidence interval and a 5% exact standard error, we required a sample of 200 individuals. The 200 women who participated in the study were outpatients in Monterrey. They were interviewed by a psychologist while waiting for their appointments. The sampling process was performed between June 2010 and May 2011.
In a face-to-face interview we questioned patients in order to obtain sociodemographic and clinical information. After the interview, the patients were given 3 scales so they could answer them in the presence of the interviewer.
The scale of feared and perceived discrimination for women with HIV (DTP-40-MV)21 was developed for this study at a qualitative phase.19 This scale measures discrimination in expectation and perception aspects as a consequence of being HIV positive or having acquired immunodeficiency syndrome (AIDS). It consists of 40 Likert scale questions with a range from 1 "nothing" to 5 "completely". Patients are presented with a series of situations of discrimination against HIV-seropositive people and/or people with AIDS, and asked how much these situations describe their own expectations or experiences. All items are direct and their total discrimination score is obtained simply by adding them. Their internal consistency is high (α = 0.92). It incorporates 6 correlated factors: feared discrimination with 11 indicators (α = 0.94), perceived discrimination at work and in the neighborhood with 8 indicators (α = 0.93), perceived discrimination at home with 8 indicators (α = 0.88), perceived discrimination in clinical care with 5 indicators (α = 0.91), perceived discrimination upon review of medical records with 2 indicators (α = 0.91), and moments of discrimination with 6 indicators (α = 0.85), with an accepted scale-free least squares: χ2/gl = 1.75, GFI = 0.94, AGFI = 0.93, NFI = 0.92, RFI = 0.91, and RMS SR = 0.01.21 These psychometric properties were estimated in the same sample as the study. The BDI-222,23 consists of 21 questions with 4 options each scored 0 to 3. A higher score reflects a greater presence and intensity of depressive symptoms. The adjustment of the model of 2 correlated factors by least squares was acceptable: χ2/gl = 2.14, FD =2.02, PNCP = 1.08, GFI = 0.81, AGFI = 0.76, and RMSEA = 0.08.
The Anger Expression Scale of State-Trait-Anger Expression Inventory (STAXI-2-AX/EX)24,25 includes 21 Likert scale questions ranging from 1 "almost never" to 4 "almost always". It uses a 4-point frequency scale, 3 with 6 items each (anger control-out, anger control-in, anger expression-out), and 1 with 3 items (anger expression-in). The total score is obtained by adding the items. Total score of anger expression is obtained by adding the 9 items of anger expression-out and anger expression-in, constant 39 and deducting 12 items in anger control-in and anger control-out. In the present sample, in order to accomplish an acceptable solution in the confirmatory factor analysis, following the exploratory factor result, we added anger expression-in and anger expression-out (α = 0.89), anger control-in remained with 6 items (α = 0.88), just as anger control-out (α = 0.79). This correlated-factors model displayed good adjustment to generalized least squares: χ2/gl = 2.04, FD = 1.54, PNCP = 0.79, GFI = 0.84, AGFI = 0.80, and RMSEA = 0.07. The internal consistency of the 21 items was high (α = 0.89).
Using statistics we analyzed the relationship between sociodemographic and affective variables with 3 subscales of studied discrimination through Pearson's product-moment correlation coefficient (with numerical variables), biserial-punctual (with dichotomous variables), and ETA (with polytomous variables). We compared the statistical averages of each of the 3 studied discrimination subscales; analysis of variance and Student t test were used for paired samples.
Using linear structural equation modelling, we contrasted a relationship model between discrimination, depression, and anger. We performed this utilizing the maximum likelihood method.
For linear structural equation modeling, a model was contrasted between discrimination, depression, and anger using the maximum verisimilitude method.This method was chosen because it is the most accurate for parameter estimation and the multivariate normality assumption, required for this method, was fulfilled as it was indicated by a normalized value of the multivariate kurtosis of Mardia (critical reason) lower than 2.26 Nine adjustment indexes were considered: the statistical chi-squared (x2), the quotient between the statistical chi-squared and its degrees of freedom (x2/gl), the function of discrepancy (FD), the parameter of non-central populations (PNCP), Jöreskog and Sörbom's goodness-of-fit index (GFI) and its corrected form (AGFI), Bentler-Bonett's normed fit index (NFI) and comparative fit index (CFI), and Steiger-Lind's root mean square error of approximation (RMSEA). The following were stipulated as good adjustment values: p of χ2 > 0.05, χ2/gl ≤ 2, FD and PNCP ≤ 1/5 of the corresponding values to the independent model, GFI and CFI ≥ 0.95, AGFI, NFI and RFI ≥ 0.90, RMSEA and RMS SR ≤ 0.05. And as acep-table adjustment values: p of χ2 > 0.01 χ2/gl ≤ 3, FD and PNCP ≤ 1/4 of the values corresponding to the independent model, GFI,CFI and RFI ≥ 0.85, AGFI and NFI ≥ 0.80, RMSEA and RMS SR < 0.08.26,27 The correlation values less than 0.30 were considered low, from 0.30 to 0.69 were considered moderate, and greater than 0.69 were considered high.28 in contrasts of parameters, the equivalence to 0 null hypothesis was rejected with p ≤ 0.05.28
Results
Sample description
Seventy-nine percent of patients reported having been infected by their spouse or live-in partner, 15.5% by a casual partner, 2% by a customer, 1.5% by a partner outside of marriage, 1% by a boyfriend, 0.5% as a result of rape, and 0.5% by vertical transmission (mother-child). The average time elapsed from the moment they had been diagnosed was 3.7 years (SD= 3.17), varying from 1 month to 18 years. Patients' average age was 34.8 years (SD = 8.63; 18 to 50 years). Median and average level of education was incomplete junior high school. Forty-three percent of participants reported being married, 22.5% single, 14% living with a partner, 9.5% widows, 6% separated, and 5% divorced. Sixty-two percent of these women reported having children. Concerning religious beliefs; 88.5% were catholic and 11.5% christian.
Discrimination feared in diverse social situations
By dividing the average discrimination feared subscale (M = 35.2) by its number of items (11), and rounding up the result, we obtained 3 which corresponded to "a lot", in a range from 1 ("nothing") to 5 ("completely").
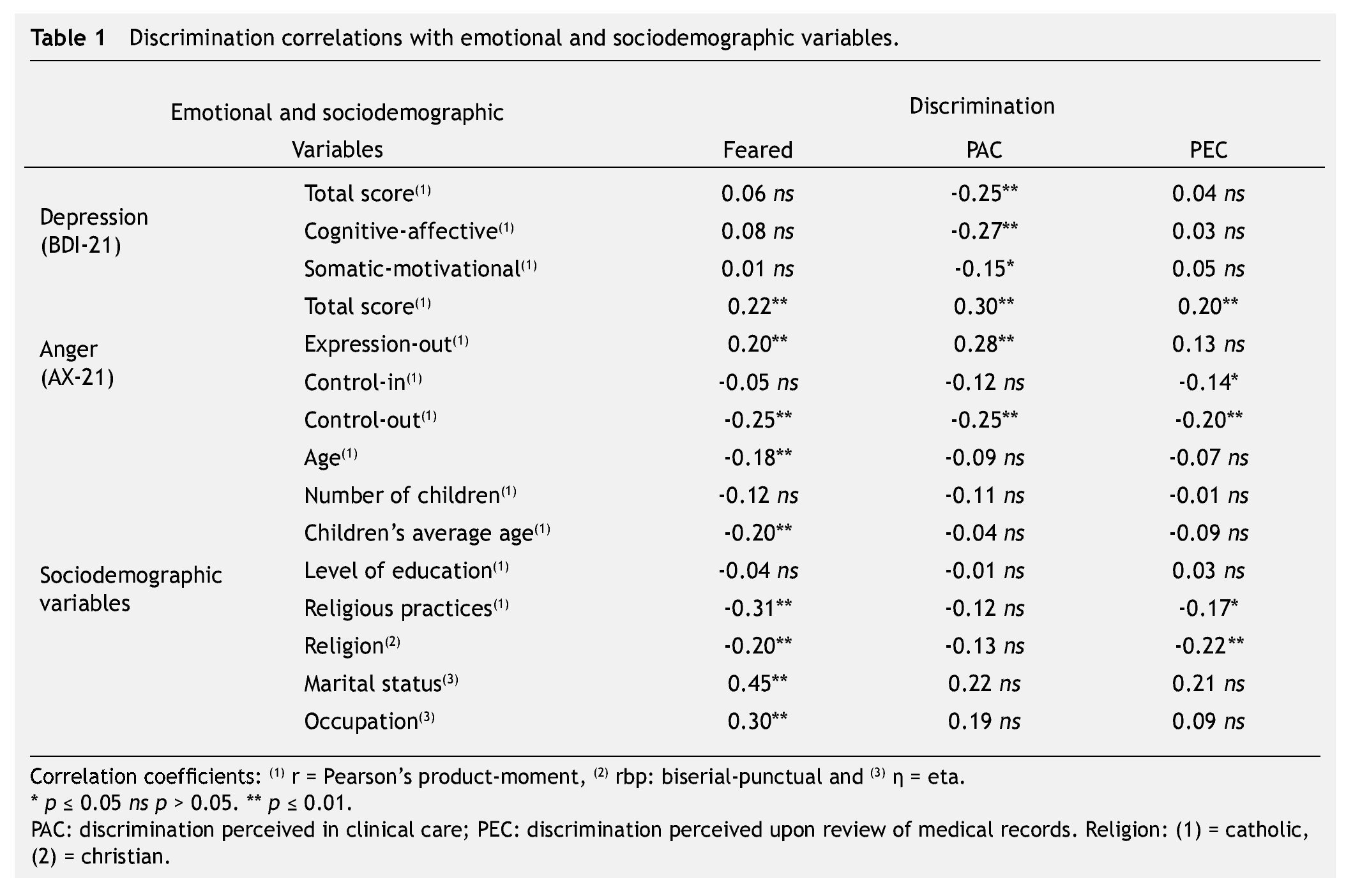
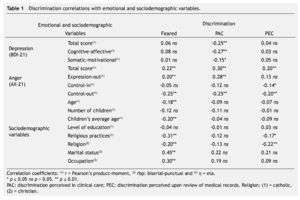
Feared discrimination correlated with a younger age in the participants, a lower average of their children's ages, a lower frequency in attendance to religious services, their marital status, religion, and occupation; moreover, and among the affective variables with a higher total score of anger, higher anger expression-out, and lower anger control-out. Single women who were living from commercial sex and catholics had a greater fear of being discriminated against (Table 1).
Discrimination perceived in clinical care, and upon review of medical records
After dividing the average of the discrimination perceived subscale in the clinical care (M = 11.0) by the number of items (5) and rounding up the result, we obtained 2, which corresponds to "a little".
Discrimination perceived in clinical care was independent of sociodemographic variables. It correlated with a lower total score of depression and its 2 factors of cognitive-affective and somatic-motivational symptoms, as well as a higher total score of anger, higher anger expression-out, and a lower anger control-out (Table 1).
After dividing the average of the discrimination perceived upon review of medical records (M = 6.4) by the number of items (2) and rounding up the result, we obtained 3, which corresponds to "a lot".
Discrimination perceived upon review of medical records correlated with religion (catholics perceived more discrimination), a higher total score of anger, lower anger control-out, and a lower frequency of attendance to religious services (Table 1).
Correlation and differences of averages between 3 discrimination subscales
Correlation of feared discrimination with perceived discrimination in clinical care was moderate (r = 0.40, p < 0.01), whereas correlation with perceived discrimination upon review of medical records was low (r = 0.29, p < 0.01). Correlation between both perception subscales was moderate as well (r = 0.40, p < 0.01).
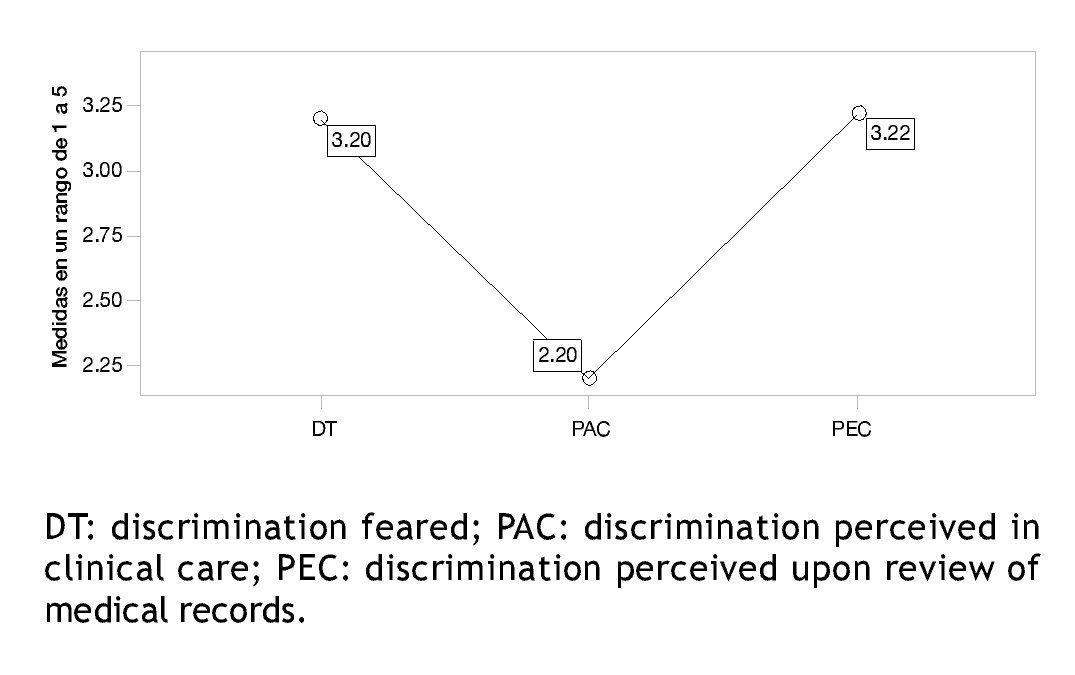
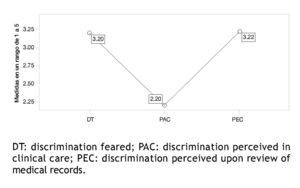
In order to accomplish a homogeneous range from 1 to 5, thus to be able to make intra-group average comparisons, we divided each scale's score by its number of items. There was a difference between averages in the 3 subscales (F[2, 398] = 68.76, p < 0.01, assuming sphericity in the Mauchsly test: W = 0.99, χ2[2, N = 200] = 1.11, p = 0.57). The average of perceived discrimination in clinical care was lower than the average of perceived discrimination upon review of medical records (t[199] = -10.67, p < 0.01), and feared discrimination average (t[199] = -9.92, p < 0.01), being the averages statistically equivalent in these last 2 subscales (t[199] = -0.20, p = 0.83) (Fig. 1).
Figure 1 averages diagram.
Structural model of discrimination, anger, and depression
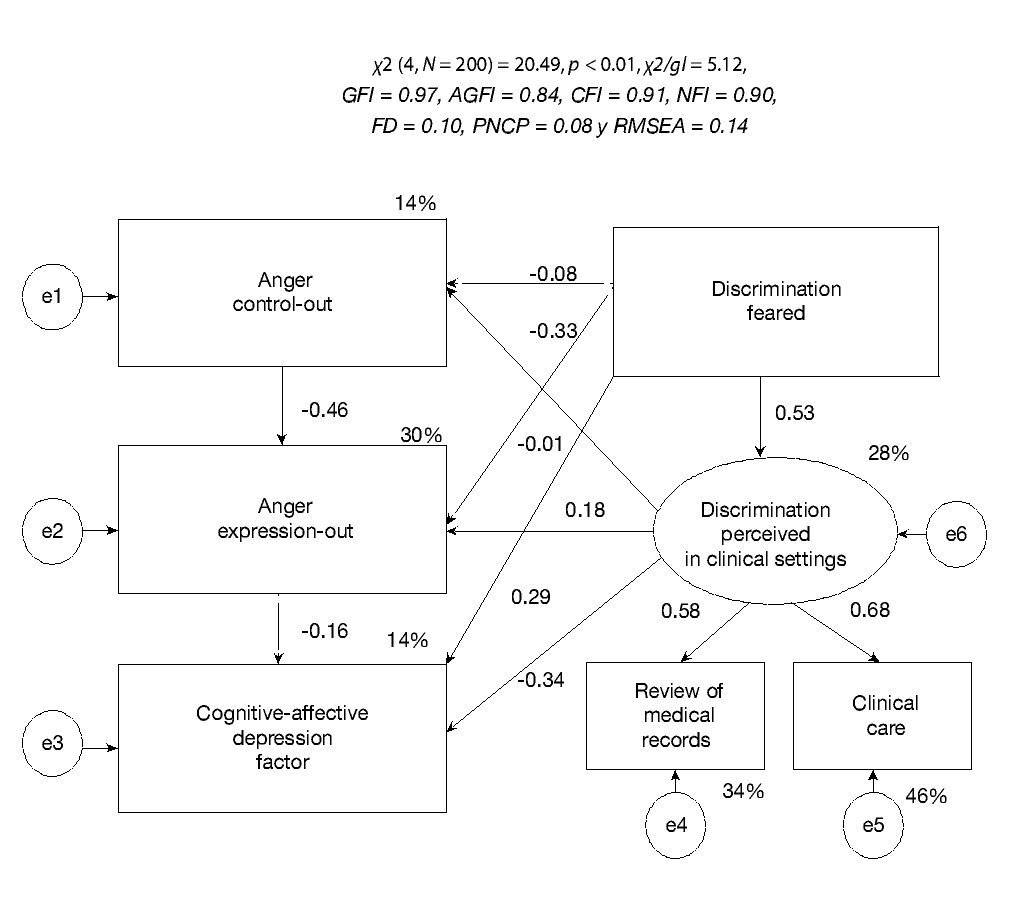
The model was calculated only with the subscales. We specified a latent perception of discrimination in clinical settings factored with 2 indicators (clinical care and upon review of medical records). Given its highest correlation with the 3 discrimination subscales, we considered cognitive-motivational depression symptoms as well as anger expression-out and control-out.
Cognitive-affective symptoms correlated with anger expression-out (r = -0.19, p < 0.01) and were independent from anger control (r = 0.13, p = 0.06).
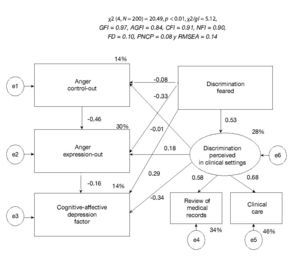
Taking into account these last 2 correlations, we specified a first model where the loss of anger control-out predicted anger expression-out. Anger expression-out predicted a reduction of the cognitive-affective symptoms of depression. Feared discrimination (manifest exogenous variable) predicted awareness of perceived discrimination in clinical settings (latent endogenous variable), loss of anger control-out, anger expression-out, and cognitive-affective symptoms of depression. Perceived discrimination in clinical settings predicted loss of anger control-out, anger expression-out, and a decrease in cognitive-affective symptoms of depression.
Three out of the 9 adjustment indexes were bad (χ2[4, N = 200] = 20.49, p < 0.01, χ2/gl = 5.12 and RMSEA = 0.14), 2 were acceptable (AGFI = 0.84 and CFI = 0.91), and 4 good (GFI = 0.97, NFI = 0.90, FD = 0.10 and PNCP = 0.08). Three parameters of the directional relations of the structural model were not significant: the determination of anger control-out and anger manifestation due to feared discrimination, and the determination of the cognitive-affective symptoms due to expression-out. We explained 28% of perceived discrimination in clinical settings, 14% of anger control-out, 30% of anger expression-out, and 14% of cognitive-affective symptoms of depression (Fig. 2).
Figure 2 Standardized model of anger and depression as a consequence of discrimination, estimated by maximum verisimilitude.
According to the BDI in samples from the United States22 and Spain23, the internal consistency of its 21 items of BDI-2 was high, varying from 0.87 to 0.92; BDI-2's factorial analysis provided a 2 correlated factors solution (cognitive-affective and somatic-motivational symptoms) with an acceptable adjustment to data. In the present Mexican sample, BDI-2's 21 items had high internal consistency (α = 0.94), as well as the 14 items of factors of cognitive-affective symptoms (α = 0.93) and the 7 factors of somatic-motivational symptoms (α = 0.83). After reviewing the adjustment improvement indexes of this first model, we suggested the introduction of determination of perceived discrimination upon review of medical records by cognitive-affective symptoms of depression. We must take into account that when we partialized the effect of discrimination perceived upon review of medical records (latent factor), the correlation between anger expression-out and cognitive-affective symptoms of depression ceased to be significant (rp = -0.12, p = 0.08). When we partialized the effect of discrimination perceived in clinical care and upon review of medical records (latent factor), the correlation between discrimination feared and anger expression-out ceased to be significant (rp = 0.13, p = 0.07). The correlation between perceived discrimination and anger control-out only ceased to be significant when we partialized anger expression-out apart from the latent factor (rp = -0.12, p = 0.09). On the contrary, the correlation of feared discrimination and cognitive-affective symptoms of depression was significant, when we partialized anger expression-out effect and anger control-out (rp = 0.15, p < 0.05), and when partializing the effect of perceived discrimination in clinical care (rp = 0.17, p = 0.01), yet it had not been before (r = 0.08, p = 0.27). Furthermore, when we patialized the effect of perceived discrimination in clinical care, the correlation between cognitive-affective symptoms of depression and perceived discrimination upon review of medical records was significant (rp = 0.16, p < 0.05), yet it had not been before (r = 0.03, p = 0.68).
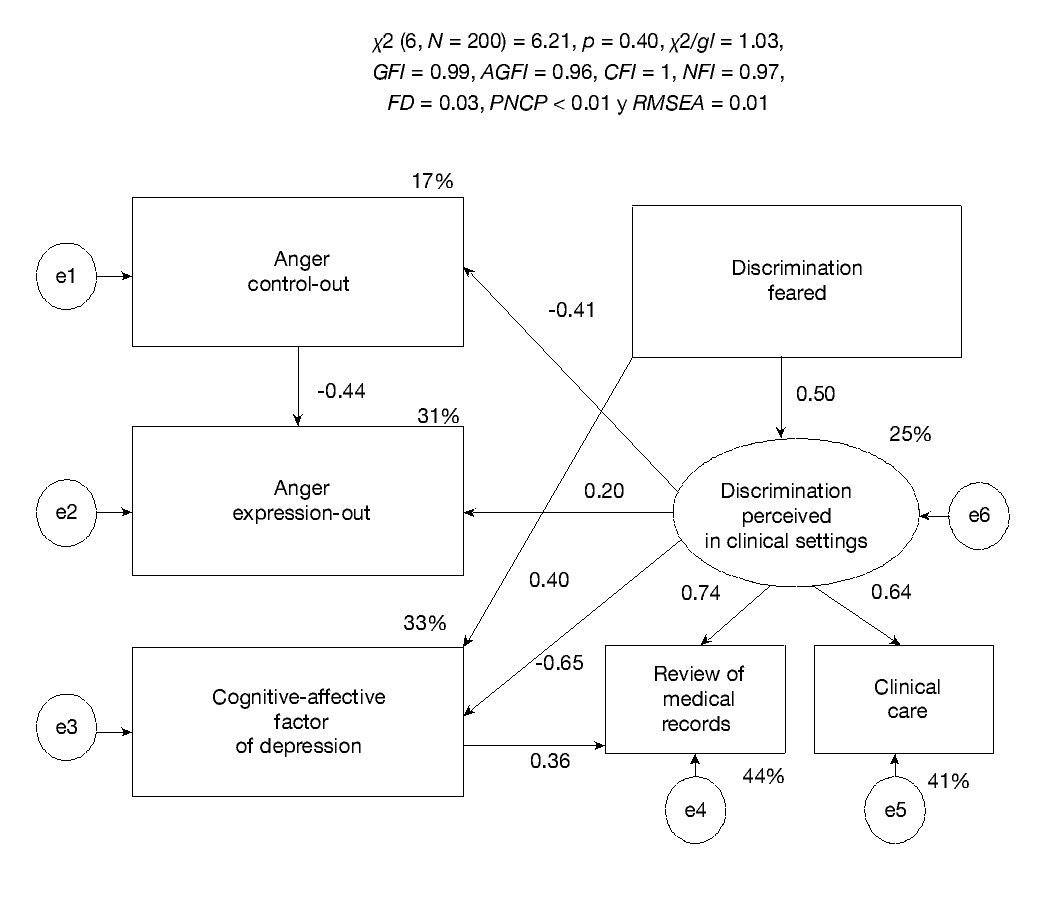
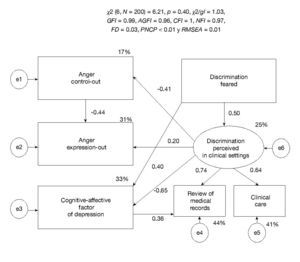
We specified a second model, eliminating non-significant parameters from the first one and considering partial correlations data, as well as suggested correction from the adjustment improvement indexes. Loss of anger control-out predicted anger expression-out. Feared discrimination (exogenous manifest variable) predicted perceived discrimination in the clinical setting (endogenous manifest variable) and cognitive-affective symptoms of depression. Perceived discrimination in the clinical setting predicted anger control-out and anger expression-out, as well as cognitive-affective symptoms of depression. Cognitive-affective symptoms predicted perception of discrimination upon review of medical records.
The value of the 9 adjustment indexes was good. The parameters of the 6 directional relationships in the structural model, and both of the parameters in the measurement model were significant. We explained 25% of perceived discrimination in the clinical setting, 17% anger control-out, 31% anger expression-out, and 33% cognitive-affective symptoms of depression (Fig. 3).
Figure 3 Reviewed standardized model of anger and depression as a consequence of discrimination, estimated by maximum verisimilitude.
Discussion
These HIV-seropositive women, mostly young women, reported fearing being discriminated against in several social situations and perceive discrimination upon review of medical records; however, the perception of discrimination in clinical care, without considering review of medical records, was low. We must point out that perception of discrimination upon review of medical records, within the group of the 6 subscales of DTP-40-MV, defined a factor of second order with feared discrimination, thus reflecting a greater connotation of expectations rather than facts. Therefore, this perception seems to be generated by administrative and auxiliary staff, and not at the moment of going in to see the doctors, nurses, psychologists, and social workers. If any of the previous studies in Mexico have directed discrimination perception in the clinical setting,29 these also seem to focus upon review of medical records amongst administration staff and auxiliaries.
Moreover, we must point out the fact that the low frequency of discrimination in clinical consultations observed is coherent with other reports.30 This tendency is also reflected by the second National Survey on Discrimination in Mexico,31 in which as compared with the first one,32 the percentage of people who would not agree to live with an HIV-seropositive person went from 44% to 35.9%.
Besides the fact that the expected discrimination level in different social situations was higher than the discrimination perception in clinical care, requiring intervention, such expectations influence perception, creating awareness. This is an aspect that is not addressed in any program directed toward HIV-seropositive patients.33,34
Frequency of attendance to religious services is an indicator of a degree of religiousness, in addition to a strong social support. This study's correlated data show that women who practice their religion more often suffer less expectations of being rejected, and perceive less discrimination upon review of medical records, as observed in other researches.35 We shall not attribute this to the context of religious community communication and support, since their effect is often the opposite,36 this due to the fact that amongst women who practice their religion more often are the widows and married who were infected by their husbands, which frees them from the social stigma of the main risk factors of HIV infection, and brings compassion from the people closer to them; on the contrary, amongst women who practice religion the least there are single women and sex-workers who attract greater social stigma.12,20 in favor of this argument we have the correlations between religious practice and discrimination increased when calculated without married women, but it ceases to be significant when single women are disregarded, making the association between marital status and religious practice significant (η = 0.38, p < 0.01).
Within depression, the cognitive-affective symptoms factor was the most related to discrimination, which can be explained by a higher affinity to evaluated contents in comparison to the somatic-motivational symptoms factor. Contrary to what was expected, cognitive-affective symptoms of depression seem to be independent of feared discrimination, but when we partialized the effect of anger control-out and anger expression-out, the relation was significant; that is, anger would disguise the relationship with the adjustment improvement of data that fear of being discriminated against increases cognitive-affective symptoms of depression.
Furthermore, perception of discrimination in the clinical setting which generated an activating reaction (more anger and less depression) was hiding the fact that the cognitive-affective symptoms of depression aroused by feared discrimination increased the perception of discrimination upon review of medical records.
These data seem to reflect the fact that these women consider it a right to be attended to and an obligation of clinical and administrative staff to provide respectful and quality care,31 hence the infringement of this right creating a reaction of anger which even reduces depressive feelings or thoughts. This relation is so well defined that it annuls anger expression-out over depression, when there is a negative correlation between these 2 variables.
We must point out as one of the limitations of the study the fact that we utilized a sample composed solely of women. Given the size of the sample, with a sample fraction of a third of the women attended to in Nuevo León, Mexico, this sample is representative, with an absolute error of 5% and a confidence interval of 95%; however, the extrapolation to similar populations must be made in the form of a hypothesis.
In conclusion, these HIV-seropositive women fear being discriminated against; however, the perception of discrimination in clinical care, aside from review of medical records, is low. As is the perception of a clinical chart with a different color from other patients', or subtle markings, certain gestures or distances from administrative and auxiliary staff seem to generate expectation of discrimination which is not confirmed by the doctors.
The expectation of discrimination increases depressive thoughts and feelings, as expected; however, this relation is only observed when we statistically control the effect of perception of discrimination in clinical care by a strong anger outburst (activator) which it generates; besides, the expectation of discrimination sensitizes perception of discrimination, in accordance with expectations.
On the other hand, cognitive-affective symptoms of depression aroused by the expectation of discrimination sensitize perception of discrimination upon review of medical records, which seems to define a closed self-reinforcing circle. This is broken by an anger outburst when discrimination in the clinical settings by doctors is perceived, when patients feel deprived of care which they are entitled to, and which has to be performed then and there without complaining.
Based on these data, we suggest contemplating the expectation of discrimination in interventions within this population of women with HIV, especially because of its depressive effect and sensitizing to the perception of discrimination upon review of medical records by administrative and auxiliary staff, which constitutes as the most frequent act of perceived discrimination in the clinical setting, even when in the consult with doctors, nurses, psychologists, and social workers they do not confirm the expectation generated by this first impression.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
No financial support was provided.
Received: November 2012;
accepted: November 2013
* Corresponding author:
Dr. Carlos Canseco 110, Mitras Centro, Z.P.
64460, Monterrey, N. L., México.
Telephono: (81) 8333 8233, ext. 423. Fax: ext. 103.
E-mail address: jose_moral@hotmail.com (J. Moral-de la Rubia).