Objectives: To determine the frequency of metabolic syndrome (MS) in patients with menopause, and to compare the incidence of MS between surgical and natural menopause.
Methods: This was an observational, longitudinal, descriptive, retrospective, unblinded study of cases seen at the Menopause Clinic of the University Hospital "Dr. José Eleuterio González" of the Universidad Autónoma de Nuevo León from March 2009 to December 2011. The frequency of MS was determined based on Adult Treatment Panel III (ATPIII) classification.
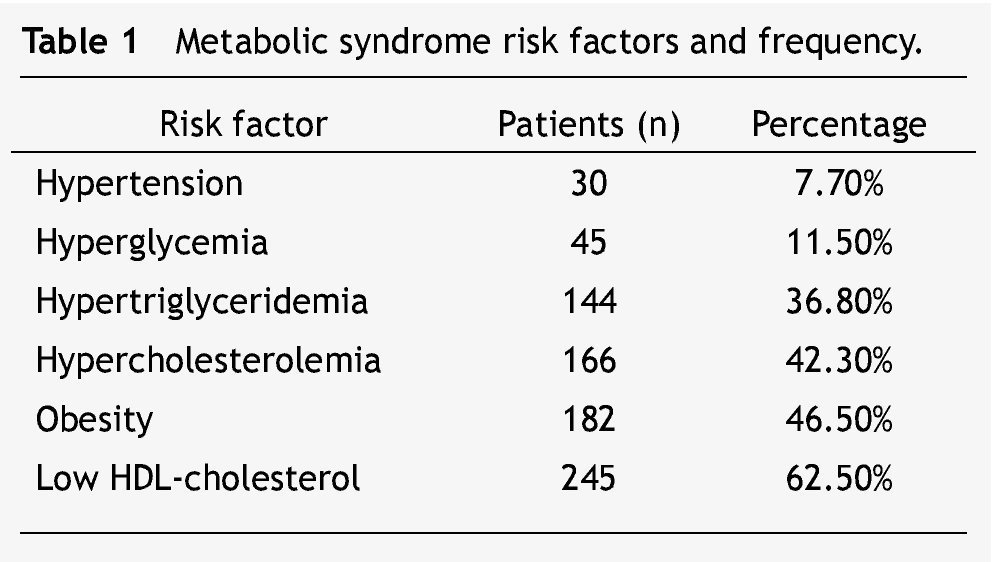
Results: at the end of the study, 391 patients were evaluated. The mean age was 50.1 years. We found a frequency of MS of 38.1%, the risk factor most often found was low HDL-cholesterol (62.5%), followed by obesity (46.5%), hypercholesterolemia (42.3%), hyperglycemia (11.5%), and hypertension (7.7%).
The incidence of natural and surgical menopause was 37.6% vs. 39.2% respectively; however, the result was not statistically significant (p = 0.093).
Conclusions: Patients with menopause are at increased risk of developing MS. It is important to detect MS early in this of patients, when they have one risk factor to avoid complications which may trigger the syndrome. We recommend screening for MS during perimenopause, in order to detect and try to delay it in a timely manner and recommend primary prevention (diet and exercise), or secondary prevention in cases with one or more risk factors.
Introduction
Metabolic syndrome is the coexistence of several pathologies or risk factors in a person. This cluster of conditions increases the risk of heart disease, stroke, and diabetes mellitus. MS has several genetically determined phenotypic variances, as well as being conditioned by environmental factors, cardiovascular disease risk factors and abdominal fat accumulation.1,2
Menopause refers to the last menstruation cycle as a consequence of the loss of activity in the ovaries. It is identified after 12 months of amenorrhea and it only occurs in humans. The follicle-stimulating hormone, which stimulates growth and storage of the ovarian follicles in the ovary, confirms menopause when found in blood greater or equal to 40 mU/dl. As a result of the complete cessation of ovarian activity,3,4 menopause can also be produced artificially following bilateral oophorectomy, after abruptly and completely suppressing the action of the ovaries, causing a sharp estrogen drop and losing the ovarian androgenic capacity.5
Menopause brings both hormonal and metabolic changes that condition an increase in body weight, producing peripheral insulin resistance, rise in blood pressure, and disorders of lipid metabolism; these are the main components of MS. Women between the ages of 17 and 24 and from 25 to 44 have a prevalence of MS of 3.8% and 16.6% respectively, compared to women between the ages of 45 and 64 with menopause, who show a prevalence of 35.8%.6,7
In order to diagnose MS the current consensus is based on criteria by the National Cholesterol Education Program, which indicates that 3 or more of the following risk factors are required in order to make a diagnosis in women: abdominal circumference of 88 cm or body mass index (BMi) of 30 or higher; triglyceride levels higher than 150 mg/dl; blood pressure of 130/85 mmHg; blood sugar levels greater than 110 mg/dl, and HDL-cholesterol < 50 mg/dl.8,9
The objective of our study was to determine the frequency of MS in women with menopause.
Methods
We carried out an observational, longitudinal, descriptive, retrospective, unblinded study of cases seen at the Menopause Clinic of the University Hospital "Dr. José Eleuterio González" of the Universidad Autónoma de Nuevo León from March 2009 to December 2011. We included patients consulting for the first time, patients who had had amenorrhea for over a year, patients having undergone bilateral oophorectomy, and patients who had not received hormone replacement therapy for at least 3 months prior to the study. We performed lab tests as well as a complete somatometry. We excluded patients who did not wish to participate and those who did not have the required tests. We eliminated patients who abandoned the study or who did not hand in complete lab results. We determined the existence of MS based on the presence of 3 or more criteria of the aTPiii classification.8,9
We created a database with collected information and analyzed it using SPSS® v. 20.0; we applied descriptive statistics to the different variables analyzed with average, median, mode, and ranges. In addition, we analyzed age, occupation, parity, and surgical or artificial menopause. During physical examinations, we assessed blood pressure, weight, height, and BMI, as well as lab tests, specifically lipid profile and fasting serum glucose results. We performed a statistical analysis using Pearson's chi square in order to analyze the frequency of MS in patients with natural vs. surgical menopause. We used convenience sampling. This study was approved by the ethics Committee of "Dr. José Eleuterio González" University Hospital.
Results
Data from 391 patients were evaluated. The mean age was 50.1 years with a minimum of 21 and a maximum of 84. Most patients were multiparous (73.5%, n = 28), housewives (82.4%, n = 322), and had attended the menopause clinic as a result of climacteric symptoms (79.3%, n = 310).
We found a frequency of MS of 38.1% (n = 149).
Only 10% (n = 43) were healthy and 50.8% (n = 199) displayed 1 or 2 criteria for MS, i.e., 1 in every 2 patients with menopause present at the University Hospital has at least 1 MS factor.
Regarding the patients with MS, we found that 92 (23%) displayed 3 criteria, 44 (11.27%) 4, and 17 (4.34%) 5 or more criteria for the syndrome.
The risk factor most often found was low HDL-cholesterol (62.5%, n = 245), followed by obesity (182 [46.5%] and patients who had a BMi greater than 30 kg/m2]. The third most frequent factor found was hypercholesterolemia (42.3%, n = 166), followed by hypertriglyceridemia (38.3%, n = 144). The least frequent factors were hyperglycemia and high blood pressure (11.5% [n = 45] and 7.7% [n = 30], respectively) (Table 1).
Regarding the comparison of the incidence of MS between women with natural and surgical menopause, we found a frequency of 37.6% (n = 49) vs. 39.2% (n = 100), respectively; this result was not statistically significant (p = 0.093).
Metabolic syndrome was more frequent in patients in the fifth decade of their lives; comparing the onset of natural versus surgical menopause we observed in the latter group an onset at a younger age (mean age of 49.2), beginning even in the third decade of their lives (21 years).
Discussion
In recent years, MS has become more and more common throughout the world, occuring in 25% of the population, especially in the US and Latin america where up to one third of the population suffers from obesity.10
We found the syndrome in over a third of our patients (38.1%), which concurs with the literature, where an incidence of 30% to 70% is reported.10,11 results from studies carried out in Latin america are similar to ours. In 2011, Tabares et al. Analyzed the cases of MS in 189 postmenopausal women, finding an incidence of 31%.12 in Brazil, albuquerque evaluated the presence of MS in pre- and postmenopausal women, finding a similar percentage to ours (34.7%),13 being greater in menopausal women than those premenopausal, which concurs with the hypothesis in this study.
When comparing in our study the frequency of MS in natural and surgical menopause, no significant differences were found; however, the percentage was lower in the first group. In 2008, Dorum A et al. carried out a study in Norway finding a higher prevalence of MS in patients who had undergone bilateral oophorectomy before 50, hence a greater risk of heart diseases.14
Conclusion
MS is frequent among postmenopausal women attending the Menopause Clinic of the "Dr. José Eleuterio González" University Hospital. The most frequent criteria for this diagnosis were -in order of importance-: low concentrations of HDL-cholesterol, obesity, and hypercholesterolemia. Only a few patients with menopause did not show any risk factor; on the contrary, 50% showed 1 or 2 factors for this syndrome. It can be infered that these women are prone to suffer some chronic disease; therefore, early detection and action to reverse this condition are essential. We did not find a difference between MS frequencies in patients with natural vs. surgical menopause; however, analysis of age groups showed that patients who had undergone bilateral oophorectomy were younger than those with natural menopause. We recommend screening for MS during perimenopause, to detect and try to delay it in a timely manner, having as an advantage the fact that this prevention is low-cost and easy to perform.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
No financial support was provided.
Received: February 2013;
accepted: October 2013
* Corresponding author:
Domingo Gayoso 240, Centro, Z.P.
64000, Monterrey, N. L., México.
Telephone: (81) 1066 1243, (81) 1516 4865.
E-mail address: Thamar84@hotmail.com (M. Cervantes-Flores).