Adequate diagnosis and treatment of penetrating cardiac injury (PCI) represents a great challenge for the surgeon in the emergency department (ED) because of its high mortality. It is estimated that more than 90% of mortality happens before the patient reaches the hospital and only 15–50% of those will receive appropriate medical treatment.
Case reportA 42-year-old hemodynamically stable male is brought to the ED with a protruding nail in his thorax. He is taken to the operating room (OR) where a medial sternotomy is performed and an injury is found in the left ventricle. Cardiac muscle repair is performed with pericardial patch.
DiscussionPCI from a suicide attempt secondary to a nail hammered into the chest is very rare and no previous reports were found by the author.
ConclusionThe objects that penetrate cardiac structures must be removed in a proper OR with capable personnel and the resources available to perform procedures like an urgent thoracotomy or sternotomy.
Proper diagnosis and treatment of penetrating cardiac injuries (PCI) are a great challenge for the surgeon at the emergency unit due to its high mortality rate. Estimations suggest that patients with a PCI have a 90% mortality rate before reaching the hospital and only between 15% and 50% of them will receive proper medical attention.1–3 Even though these injuries are common in military conflicts, incidence amongst civilians has risen worldwide, not only related to violence but also in industrial accidents and suicide attempts. Within this last aspect, previous reports have shown the danger of nail guns, which can cause injuries to any organ.4 PCIs secondary to this are rare; even rarer are the penetrating injuries by suicide attempt with a nail hammered by themselves. This case is presented to discuss PCI management in stable patients.
Case reportA 42-year-old male with a history of alcohol and cocaine abuse was taken to the ER by his relatives after finding him disoriented on the floor. The patient was stable at his arrival, with a heart rate of 115, blood pressure 120/70, and respiratory frequency of 18. During physical examination, the doctor became aware of the presence of three periareolar injuries and another injury in the 4th intercostal space over the mid-clavicular line, all of them on the left hemithorax. A nail's head was visible protruding from the thorax, with a pulsating movement. The patient did not have active bleeding. However, he presented abnormal heart sounds and jugular vein distention.
A thoracic X-ray showed the presence of a nail inside the cardiac incision, without pneumothorax or hemothorax data (Fig. 1). The transthoracic echocardiogram (TTE) showed the presence of a sharp body inside the left ventricle, with data of moderate pericardial liquid.
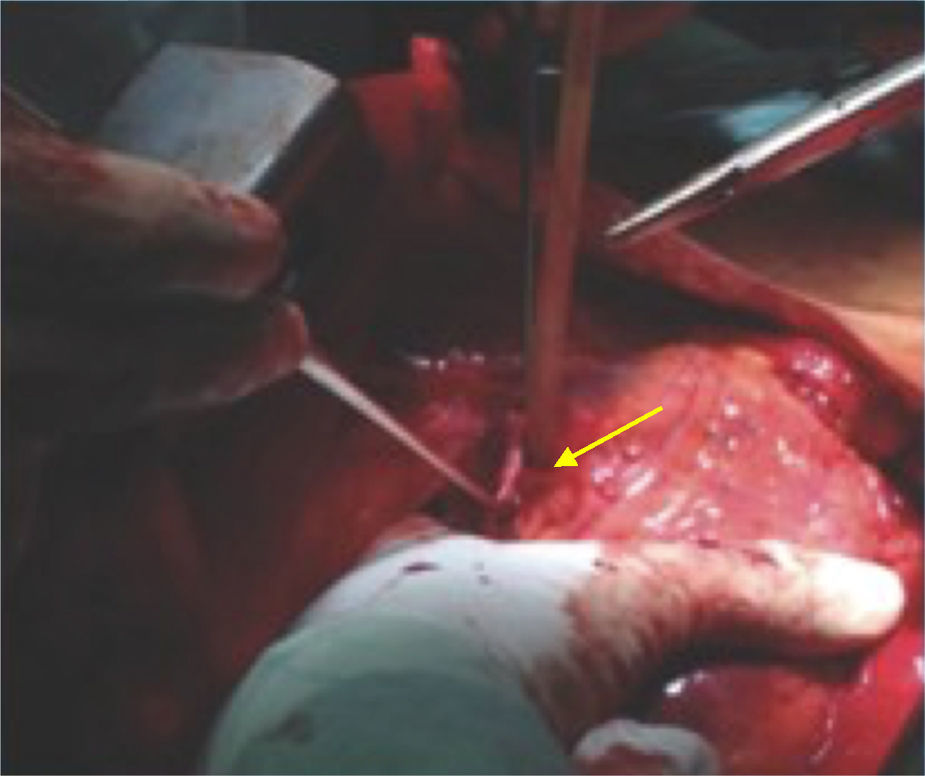
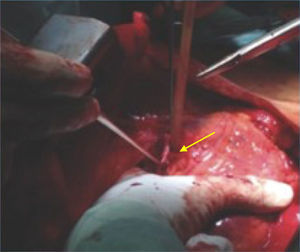
The patient was immediately transferred to the OR where he underwent a median sternotomy. The pericardium was opened, obtaining 100ml of blood. It was evacuated and active bleeding around the nail was observed. The 11.5cm nail was removed under direct view, and a #18 Foley catheter was placed in the defect for bleeding control. The heart and its adjacent structures were checked and additional injuries were ruled out. The ventricular defect was repaired with 3-0 Prolene and a pericardial patch was performed (Fig. 2). The area was irrigated profusely with isotonic solution and mediastinal drainage was placed.
Post-operative care evolved without complications; under direct interview, the patient revealed he attempted suicide. Subsequent to psychiatric intervention, the patient was discharged and admitted into the local psychiatric hospital.
DiscussionDirect injuries to the cardiac muscle may be successfully treated through surgery if the patient is taken to and treated at a center with technical capabilities for heart surgery. The presented case is a clear example of this. There are two commonly involved mechanisms in PCI: gunshot wounds (GSW) or wounds with a sharp object (WSO), with a survival rate of GSW victims of 16% versus 65% for WSO victims.5 In our patient's case, his injury was self-inflicted using a nail (WSO), resulting in injuries with a better chance of being repaired than those caused by a gunshot. PCIs are emergencies that put the patient's life at risk and require immediate diagnosis and treatment. There are two suggested methods for evaluation.
Subxiphoid window (SW) and non-invasive studies, such as ultrasound and echocardiography (EC). SW remains the gold standard for diagnosis in high-volume hospitals with limited capacity for diagnostic ultrasounds: SW's sensitivity and specificity are 56%, versus the 96% of EC. Hence, EC has become a standard in the care of stable patients with IPC, becoming the first option in the emergency room.
In case the patient is unstable, with tamponade or hemodynamic instability, he/she must be taken to the OR to perform an emergency thoracotomy or a median sternotomy. Myocardial injury caused by a nail is a rare event, one which has been reviewed.6 On the other hand, a suicide attempt secondary to a nail injury is even rarer; there are no previous reports found by the authors. Our hypothesis regarding the several previous injuries is the sense that they were unsuccessful attempts to hammer the nail into his heart. This is explained by the complex situation from the psychiatric point of view and in the addictions in which the patient was immersed.
In conclusion, objects that penetrate cardiac structures must be removed in a proper OR with capable personnel and the resources available to perform procedures like an emergency thoracotomy or sternotomy.
Conflict of interestThe authors have no conflicts of interest to declare.