Carbon monoxide (CO) poisoning is one of the most common causes of morbidity and mortality by poisoning. This type of toxicity results from tissue hypoxia and CO-mediated damage at the cellular level. Neurological sequelae constitute the principal cause of associated morbidity. The development of acute hydrocephalus is an extremely rare complication. We present a case of CO poisoning in an adult male who developed acute obstructive hydrocephalus secondary to bilateral cerebellar oedema.
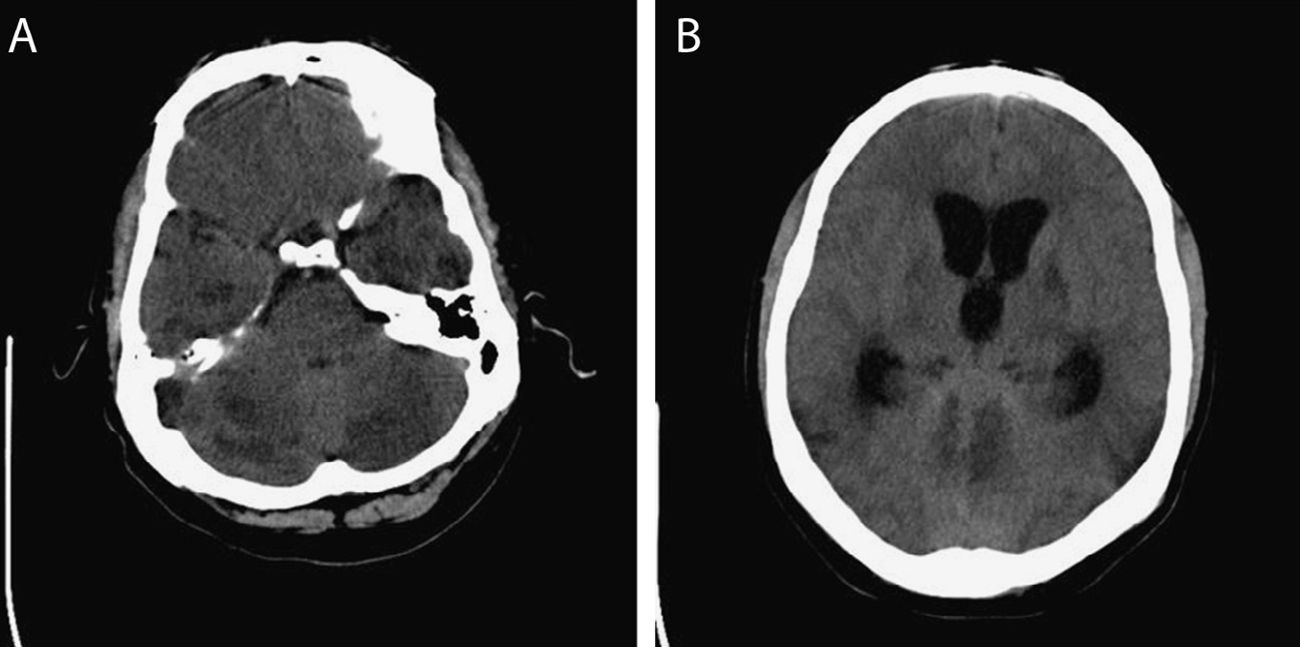
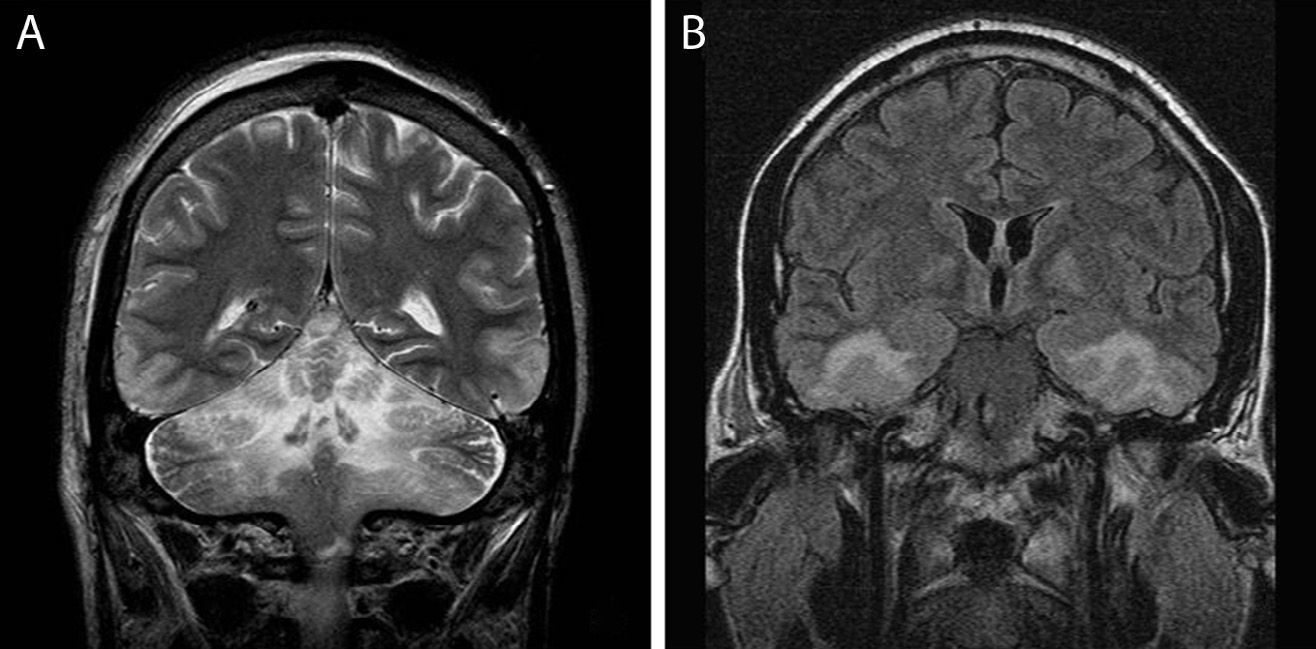
The patient was a 38-year-old man with a medical history hypothyroidism treated with thyroid hormone replacement therapy. He also presented personality disorder and had attempted suicide several times. He was found unconscious inside a car inhaling exhaust gases, and beside him were 2 empty blister packs of benzodiazepines. Upon arrival at the emergency department, the patient had a low level of consciousness (Glasgow Coma Scale=3) and mid-dilated miotic pupils which were poorly reactive; as a result, he underwent orotracheal intubation. A cranial CT (Fig. 1) revealed diffuse hypodensities in both cerebellar hemispheres, basal temporal white matter bilaterally, both internal capsules, and the globus pallidus. The patient was admitted to the intensive care unit (ICU). A urine toxicology test revealed benzodiazepine and methadone, while CO-oximetry showed carboxyhaemoglobin levels of 23.6%. The patient was therefore mechanically ventilated with 100% oxygen until his carboxyhaemoglobin levels decreased to 0.9%, approximately 6hours later. In the 48hours after being admitted to the ICU, the patient's neurological symptoms improved to the point where he was able to obey simple instructions, although he remained drowsy. However, 72hours after admission to the ICU, the patient's state of consciousness deteriorated suddenly. An additional cranial CT (Fig. 1) revealed severe hydrocephalus affecting the lateral ventricles and third ventricle, resulting in a significant mass effect. The patient underwent emergency surgery: first, an external ventricular drain was put in place, from which exuded a clear liquid under high pressure, and then, a decompressive craniectomy of the posterior fossa was performed to relieve cerebellar herniation. After surgery, the patient remained in coma for the next 5 days (flexion–extension of both upper limbs was the only response to painful stimuli). A follow-up cranial MRI scan performed 4 days after surgery (Fig. 2) showed multiple cerebral infarcts in an early subacute stage, extensively affecting the limbic system, hippocampus, fornix, and basal temporal area bilaterally. Patchy areas of small bilateral cortical infarcts could also be observed in the frontal and parietal lobes, as well as extensive infarcts in both cerebellar hemispheres, with the most damage occurring in the territory of the superior and anterior inferior cerebellar arteries; no signs of hydrocephalus were seen. Taken as a whole, these findings suggest multiple anoxic-ischaemic encephalic lesions secondary to CO poisoning. As of the fifth day after surgery, our patient's neurological symptoms had improved progressively, reaching an adequate level of consciousness and showing no focal neurological signs. Three days later, hydrocephalus resolved and the external ventricular drain was removed after remaining closed for 48hours without visible neurological deterioration.
(A) Diffuse hypodensity in both cerebellar hemispheres, basal temporal white matter bilaterally, both internal capsules, and the globus pallidus. (B) Severe dilation of the lateral ventricles and third ventricle (the fourth ventricle was normal), which results in severe mass effect leading to effacement of the convexity sulci and a decrease in the size of the basal cisterns.
The clinical presentation and radiological findings of CO poisoning vary greatly. There are 3 mechanisms by which CO damages the central nervous system. Firstly, CO directly causes diffuse hypoxic-ischaemic encephalopathy, which predominantly affects grey matter. Second, although to a lesser extent, it may also cause focal lesions to the cerebral cortex, especially the hippocampus and temporal lobes. Cortical damage may manifest as transient vasogenic oedema or as a necrosis with infarct areas in the absence of cerebral artery occlusion. Third, it may cause white matter demyelination. This finding, normally undetectable in the acute phase of intoxication, is considered the cause of late-onset neuropsychiatric syndrome. This syndrome generally develops after a lucid interval, and the most common symptoms are mental deterioration (amnesia, cognitive dysfunction), emotional disorders (depression, anxiety, mutism), urinary and faecal incontinence, and motor disorders (gait alterations, parkinsonian symptoms). The globus pallidus is the structure most frequently affected by CO poisoning; damage is usually immediate, bilateral, and predominantly affects the anterior 2 thirds of this structure. Occasionally the rest of the basal ganglia are affected (putamen, caudate nucleus, thalamus); in this case, the lesions are typically asymmetrical. The brainstem and the cerebellum are less frequently affected; thus, damage to these areas reflects more severe poisoning as these posterior structures are more resistant to hypoxia.1
Acute hydrocephalus is an extremely infrequent complication of CO poisoning which has previously been described in only 2 paediatric patients2,3 and one adult.4 In every case, the patients experienced an initial clinical improvement followed by rapid neurological deterioration after 24 to 72hours. All neuroimaging tests revealed obstructive hydrocephalus secondary to bilateral cerebellar oedema with compression of the fourth ventricle. In the case of the adult patient, hydrocephalus resolved spontaneously and was accompanied by the recovery of an adequate level of consciousness within the next 72hours, while in the paediatric patients progression was slow, leading to death in one of them, despite aggressive surgical treatment with ventriculostomy. These cases along with the current one suggest that, in addition to the structures most typically injured, there are others at the level of the brainstem and cerebellum which are highly susceptible to oedema caused by the cytotoxic effects of CO.
In conclusion, although the mechanism of the development of acute obstructive hydrocephalus is well known, this case is unusual by reason of being secondary to CO poisoning. Therefore, hydrocephalus should be suspected when acute neurological deterioration is observed in the days following CO exposure.
Please cite this article as: Martín A, Tejerina E, de la Cal MA, Ramírez L. Hidrocefalia aguda secundaria a intoxicación por monóxido de carbono. Neurología. 2016;31:353–355.