Retrograde venous air embolism (RVAE) occurs when air is introduced into the venous system as a result of a negative pressure gradient, moving in the opposite direction to the normal flow of venous blood, and ultimately reaching the cerebral venous system. It may be secondary to surgery, barotrauma, or invasive procedures such as venous catheterisation, typically central but occasionally through a peripheral intravenous line (PIV). This disorder is underdiagnosed and has an undetermined prevalence and incidence, given that only anecdotal cases have been reported.1–7 Neurological findings include confusion, amnesia, epileptic seizures, cerebral ischaemic vasculopathy, and/or coma. A cranial CT scan and oxygen therapy (concentrations around 100%) are crucial for the diagnosis and treatment of this complication.7–9 We present the first reported case of a patient who unexpectedly went into a coma after experiencing an RVAE due to the accidental removal of a PIV.
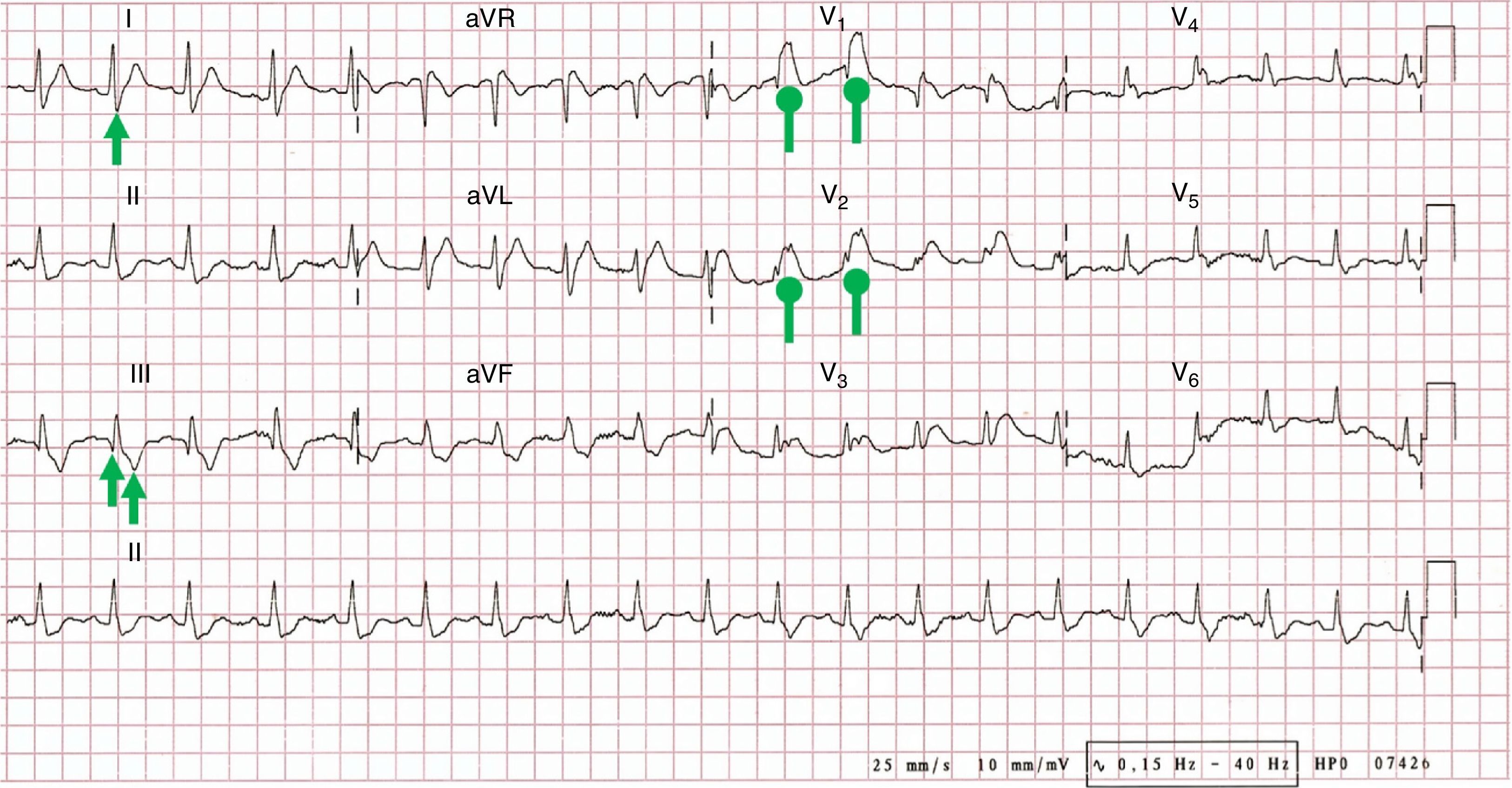
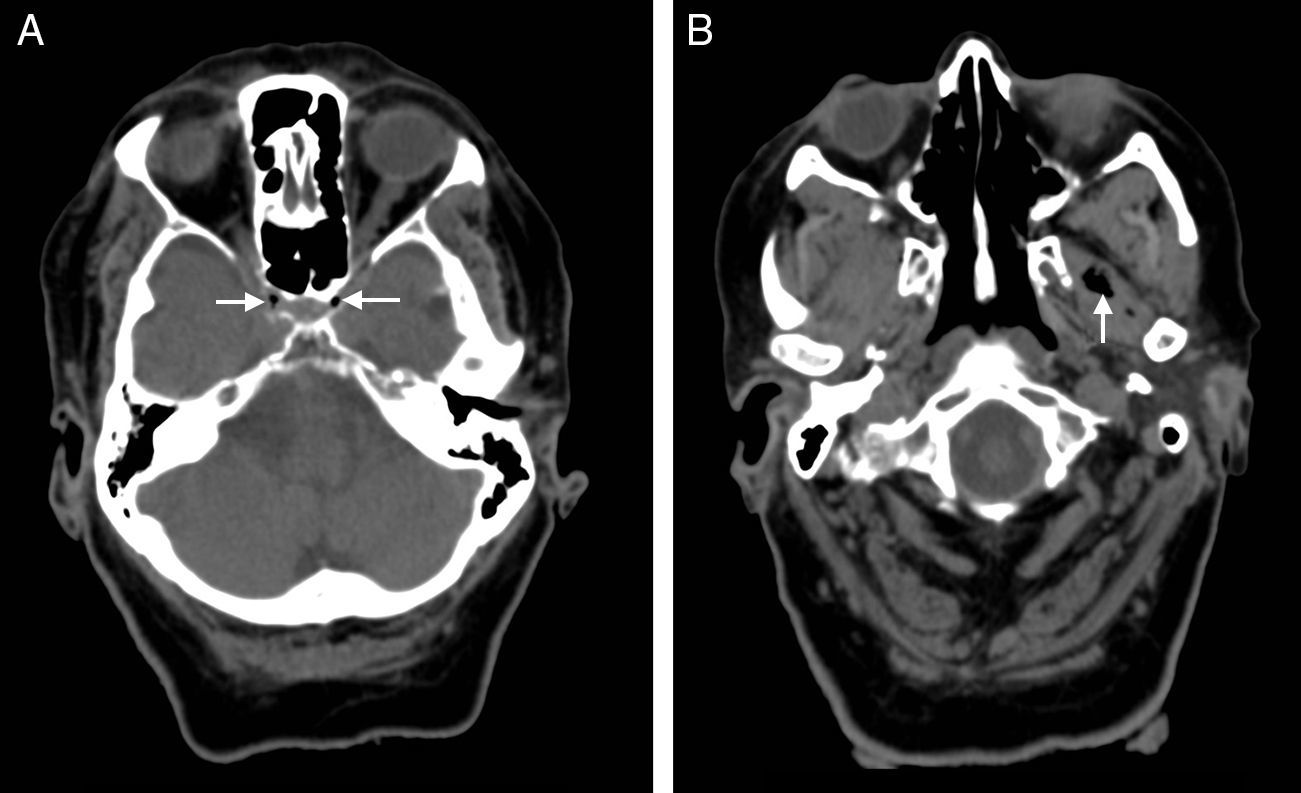
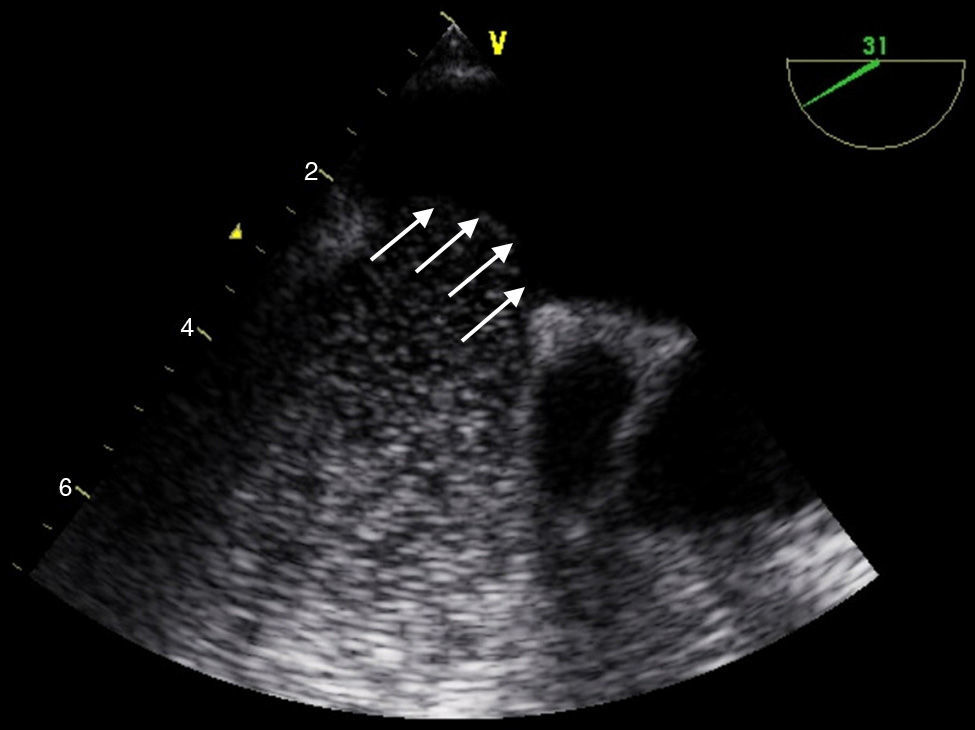
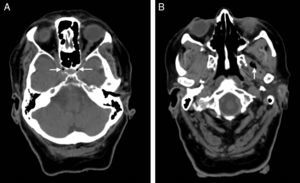
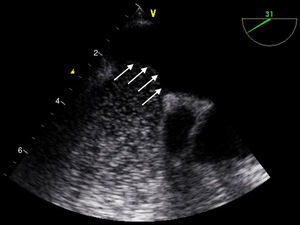
Our patient was a 79-year-old woman with no relevant medical history who was admitted due to lower limb cellulitis. While hospitalised, she removed her PIV accidentally when she was getting out of bed; as a result, she experienced a sudden drop in arterial blood pressure, tachypnoea, and a decrease in the level of consciousness. During the examination, the patient spoke unintelligibly, did not open her eyes, and showed no withdrawal reflex to nociceptive stimulation (Glasgow Coma Scale 4: E1/V2/M1) and a subcutaneous emphysema in the antebrachial region. The patient was admitted to the intensive care unit where she received intravenous fluid and high-flow oxygen (15L/min) using a Venturi mask with a reservoir bag. The results of a blood analysis revealed respiratory acidosis, a temporary increase of biomarkers for myocardial necrosis, and d-dimer levels within normal ranges. An ECG showed acute right ventricular overload and pulmonary hypertension (PH) (Fig. 1), while a thoracic radiography revealed incipient signs of heart failure. A cranial CT scan disclosed air bubbles in both cavernous sinuses (Fig. 2A) and in the left infratemporal fossa (Fig. 2B). We ruled out toxic, metabolic, and infectious causes. Within 24-48hours the patient underwent a helical CT angiography (ruling out pulmonary thromboembolism), transoesophageal echocardiography (ruling out an atrial septal defect) (Fig. 3), right cardiac catheterisation (obtaining a mean pulmonary arterial pressure of 46mmHg, indicating moderate PH), and a cranial MRI scan (which showed leukoaraiosis and age-dependent cortico-subcortical atrophy). The patient was diagnosed with coma secondary to a cardiogenic shock brought on by RVAE. Our patient progressed favourably and showed an excellent response to oxygen and saline therapy; in 3 months, she had recovered ad integrum.
A simple axial CT scan performed 50minutes after symptom onset revealed air bubbles (arrow heads) inside both cavernous sinuses in the parasellar region (A) and at the level of the left lateral pterygoid muscle (B), adjacent to the trajectory of both internal carotid arteries, which exhibit signs of intracavernous atheromatous calcification.
A transoesophageal echocardiogram was performed 24hours after symptom onset. Spontaneous echo contrast was not seen even during the Valsalva manoeuvre. The image reveals a protrusion of the interatrial septum (indicative of increased pressure in the right cardiac cavities; arrows), but no interatrial connection or air bubbles (probably dissolved in the systemic circulation).
The physiopathological mechanism of developing RVAE involves the gas entering the right heart cavities (via the superior vena cava) and the pulmonary circulation (via the pulmonary artery). This affects ventilation/perfusion, promotes right-to-left intrapulmonary shunting, and increases alveolar dead space. In addition, if the volume of air embolism is high, it can also cause PH, right ventricular overload, decreased cardiac output, and eventually low cerebral perfusion pressure and coma.10–12 Recently, it was experimentally demonstrated that there is greater likelihood of air reaching the brainstem after PIV manipulation, during Valsalva manoeuvres, and in hypovolaemia (which leads to a decrease in central venous pressure), and particularly when elevating the thorax (angles≥45° above horizontal), and air flow rates≥0.2L/min.13–15
Diagnosis of RVAE, made by exclusion, is based on a high level of clinical suspicion, the presence of intracranial air in neuroimaging (before it is absorbed by the systemic circulation), and the absence of a right-to-left cardiac shunt in an echocardiogram. Treatment includes: an occlusive dressing over the area to prevent more air entering, the Durant manoeuvre (placing the patient in the left lateral decubitus position and the Trendelenburg position), support measures (volume expansion), inotropes, antiepileptics, and oxygen (100%) (which reduces the size of the air embolism by increasing the output gradient of nitrogen inside the air bubbles), and hyperbaric oxygen therapy, if available, in more severe cases.13,16,17
Ours is the first reported case of coma secondary to RVAE caused by PIV use and shows the pathophysiological mechanism of RVAE. Because RVAE can occur as a result of procedures carried out in nearly all medical specialities, it is important that clinicians remain alert and informed regarding this atypical but potentially devastating complication. Late diagnosis and treatment of RVAE may result in irreversible sequelae. Therefore, this entity should be included in the differential diagnosis of patients with PIV lines in certain clinical contexts who display cardiopulmonary and neurological symptoms not explained by other causes.
We would like to thank Drs Laura Izquierdo Esteban, Laura Araceli Lozano García-Caro, Pablo Nieto González, Victoria Galán Sánchez-Seco, José Tejeiro Martínez, Francisco Cabrera Valdivia, Carla Sonsireé Abdelnour Ruiz, María Molina Sánchez, and María Henedina Torregrosa Martínez.
Please cite this article as: León Ruiz M, Benito-León J, García-Soldevilla MA, Arranz Caso JA, García-Albea Ristol E. Primer caso descrito de coma desencadenado por embolismo aéreo venoso retrógrado: una situación excepcional pero potencialmente letal. Neurología. 2016;31:350–353.