Early recanalisation of an occluded vessel is essential for good outcomes in patients with acute stroke.1 When access to the occlusion is impossible, the contralateral carotid artery may be approached via the anterior communicating artery (ACoA). We present the case of a patient with an occlusion in the distal segment of the internal carotid artery (ICA) (carotid-T occlusion) caused by an embolus in a giant aneurysm in the cavernous segment of the ICA which migrated cranially. Intracranial stenting was performed through the contralateral ICA and the ACoA.
IntroductionOcclusion of the cervical ICA resulting from thrombosis of a giant aneurysm in the cavernous segment of the ICA limits the viability of endovascular treatment. Several authors have used microcatheters to reach the emboli through ipsilateral vessels and administer intra-arterial fibrinolytic therapy.2 The literature also reports some cases of anterior-to-posterior circulation approach3 through the contralateral ICA4 using Penumbra devices.
We present the first case of stent placement through the ACoA in a patient with acute stroke due to carotid-T occlusion caused by an embolus from a giant aneurysm in the cavernous segment of the ICA.
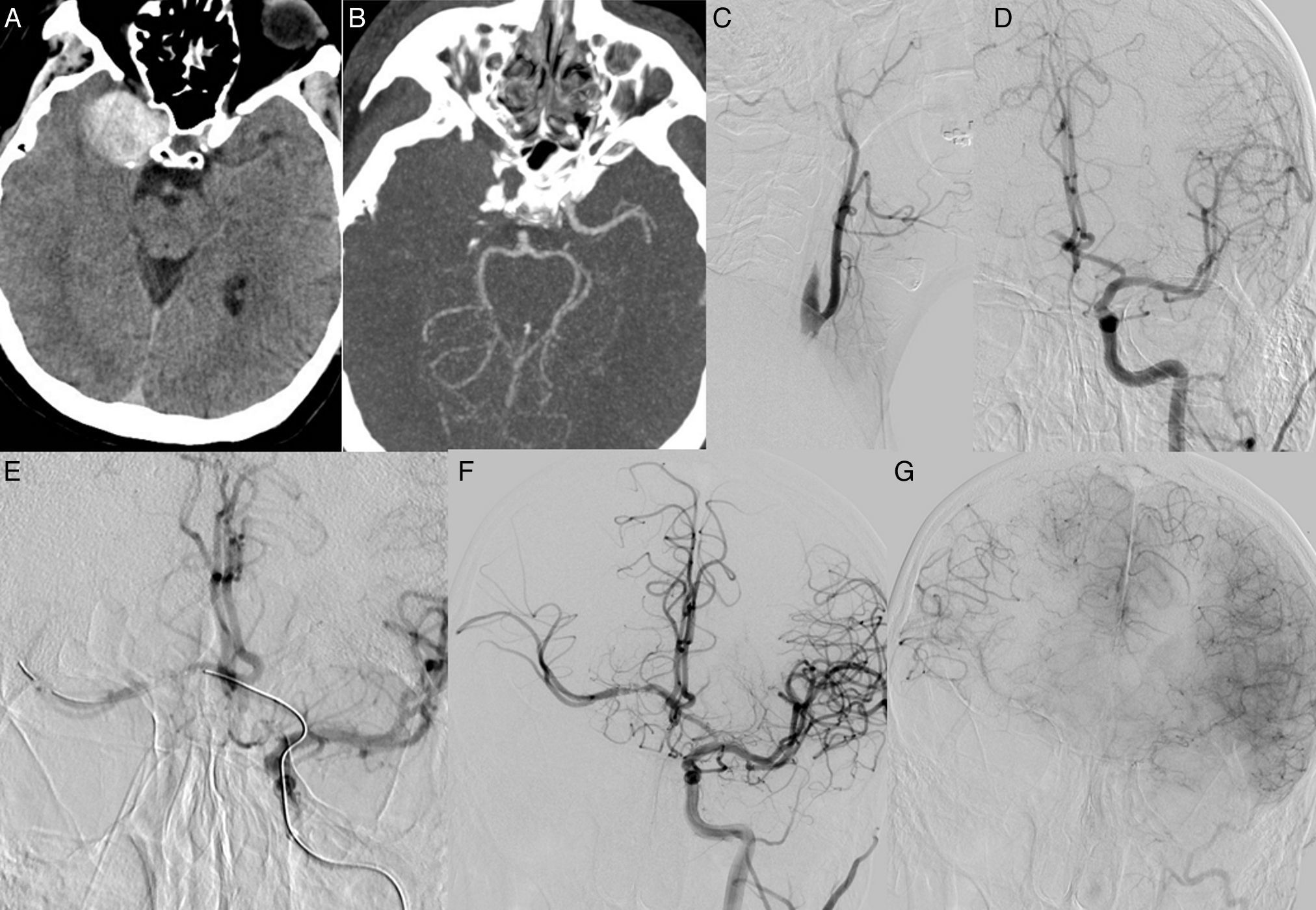
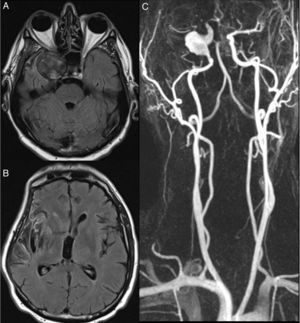
Clinical caseOur patient was a 53-year-old left-handed man with no relevant history who visited our hospital due to sudden loss of consciousness. After the patient recovered consciousness, he displayed severe left-sided hemiplegia, left facial palsy, and dysarthria (NIHSS score of 14). Code stroke was activated upon arrival at the emergency department; time from symptom onset to arrival at the emergency department was 90minutes. A brain CT scan detected an expansive process in the temporal region involving the ICA and early signs of infarction in the territory of the right middle cerebral artery (MCA) (ASPECTS score of 6). CT angiography revealed complete occlusion of the origin of the ICA resulting from thrombosis of a giant aneurysm in the ICA; occlusion extended towards segments A1 and M1 of the anterior cerebral artery (ACA) and MCA, respectively (carotid-T occlusion) (Fig. 1A and B).
(A) Hyperdense lesion in the region of the cavernous segment of the right ICA corresponding to a thrombosed giant aneurysm. (B) CT-angiography of the circle of Willis revealing no blood flow in the right MCA territory. (C) Digital subtraction angiography with contrast injection into the right CCA revealed no blood flow in the right ICA. (D) Angiography of the left CCA (intracranial projection) showing no abnormalities in the ACoA, adequate filling of the distal portion of right A1, right ACA elevation, and T occlusion in the terminal segment of the right ICA. (E) Selective catheterisation of the right ACA and MCA via the ACoA. (F) Use of Enterprise® stents between the right MCA and the right carotid artery. (G) Angiography (parenchymal phase) showing recanalisation type 2b according to the mTICI scale, associated with delayed venous drainage compared to the left hemisphere.
Angiography was performed with the Seldinger technique; we studied right intracranial circulation through the left ICA. Contrast injected into the left carotid artery was observed to flow into the ACoA towards the right A2 segment (Fig. 1C and D); we therefore decided to use a microcatheter to navigate through the ACoA in order to place a stent between right A1 and M1 to open the right distal ICA occlusion. To this end, we placed a 7F sheath introducer measuring 80cm (Super Arrow-Flex®) in the left common carotid artery (CCA); the left cervical ICA was catheterised using a Navien microcatheter of 0.072″ inner diameter (Covidien®). After administering 10mg abciximab intravenously, we placed 2 stents (Codman® Enterprise vascular reconstruction device) using a PROWLER SELECT Plus microcatheter (Codman®) and a Synchro-14 guidewire (Stryker®). An angiography (parenchymal phase) performed at the end of the procedure showed contrast passing through the branches of the right MCA (Fig. 1E-G). Recanalisation was achieved at 420minutes after symptom onset. Following our hospital's protocol, our patient began dual antiplatelet therapy (clopidogrel 75mg plus acetylsalicylic acid 100mg orally every 24hours).
Within the following 24-48hours, our patient showed a decreased level of consciousness; a brain CT scan revealed extensive oedema in the infarcted area and uncal and subfalcine herniation requiring decompressive craniectomy. Our patient was discharged after 30 days of hospital stay; he progressed favourably and experienced no complications. He scored 1 on the mRS. Mild distal paresis of the left arm and mild postural tremor persisted.
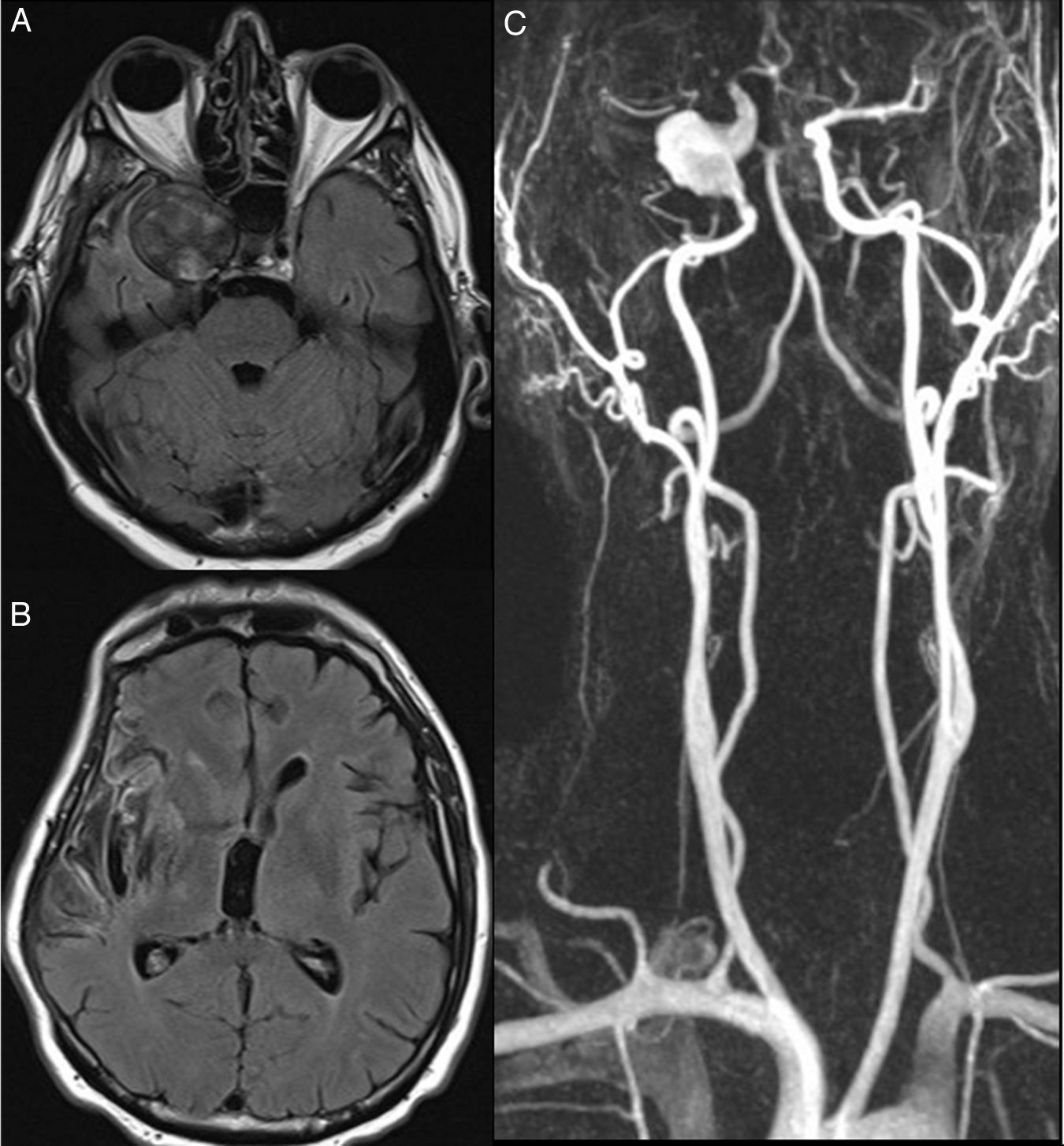
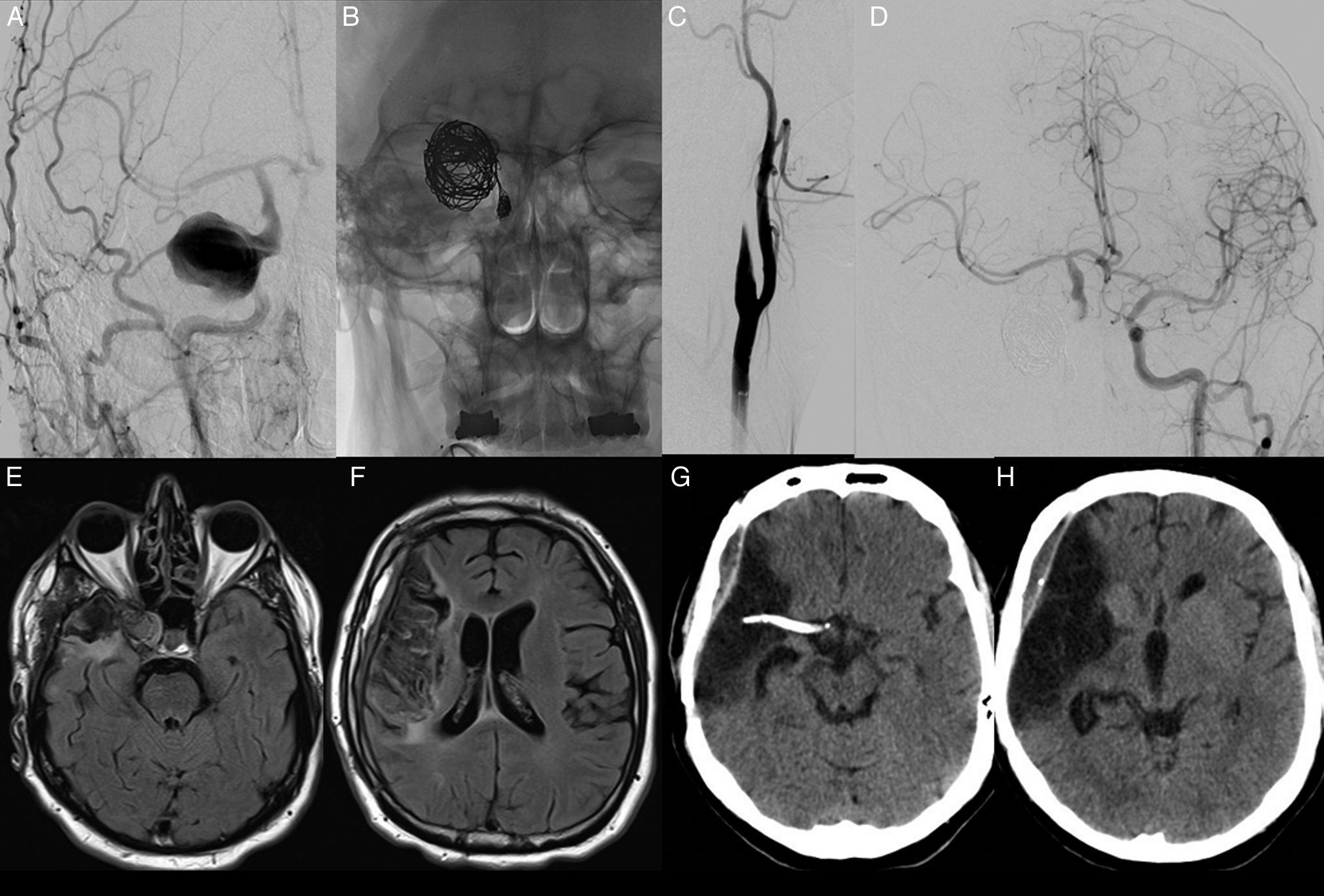
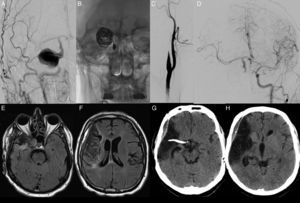
Four months later, our patient visited our department due to fronto-orbital oppressive headache, tearing, and conjunctival chemosis, suggesting cavernous sinus involvement. An MRI scan and MR angiography confirmed recanalisation of the right carotid artery and the giant aneurysm (Fig. 2). The case was discussed in a meeting of all members of our multidisciplinary team; a decision was made to perform endovascular occlusion of the aneurysm (Fig. 3).
(A) T1-weighted MRI sequence showing an aneurysm in the cavernous segment of the right ICA, which was recanalised, and turbulent blood flow. (B) T1-weighted MRI sequence displaying infarction in the right insular cortex and right temporal operculum. (C) MR-angiography of the supra-aortic trunks revealing a fusiform aneurysm in the right ICA which becomes saccular in the cavernous segment. Artefact caused by a stent between the ACA and the MCA, which makes it difficult to assess the lumen of these arteries.
(A) Angiography of the right CCA showing recanalisation of the right ICA and the aneurysm, which were previously thrombosed. (B) Skull radiography (anteroposterior projection) showing multiple coils inside the aneurysm and in the petrous segment of the right distal ICA. (C) Angiography study of the right CCA. Right ICA occlusion. (D) Angiography study of the left CCA displaying good contrast flow into the right MCA via the communicating artery and no intra-stent stenosis. (E and F) A follow-up FLAIR MRI scan performed 3 months after ICA occlusion revealed a decrease in the size of the thrombosed aneurysm and no additional ischaemic lesions. (G and H) Follow-up cranial CT scan showing a stent between the right ACA and MCA. Infarction in the right insular cortex, right temporal operculum, and right frontal operculum.
Our patient progressed favourably and symptoms associated with cavernous sinus compression by the aneurysm resolved. At 6 months, another craniectomy was performed and dual antiplatelet therapy was continued. At one year, our patient scored 1 on the mRS; he displayed disempathy and mild hemiparesis of the left arm, which was treated with rehabilitation.
DiscussionStroke due to acute ICA occlusion accounts for 15% to 25% of all cases of acute stroke.5 Prognosis in these patients is poor1; the recanalisation rate after intravenous thrombolysis barely reaches 10%.6 Although recanalisation has traditionally been a controversial treatment in cases of acute ICA occlusion, several studies and randomised trials present it as a technically viable and clinically effective treatment alternative for these patients.7,8
Moret et al.9 were the first authors to use an alternative pathway to access an occluded vessel; these authors used the posterior communicating artery. Based on this approach, Hui et al.10 treated a patient with acute stroke secondary to MCA occlusion using intraarterial thrombolysis and thrombectomy. These authors intended to navigate through the posterior communicating artery with a Penumbra device.
However, as the posterior communicating artery could not be accessed, they used the ACoA. Padalino and Deshaies4 reported 2 cases of stroke secondary to ICA dissection which were treated with a contralateral approach. In our case, the diameter of the ACoA did not allow us to use a Stentriever® for thrombous extraction; we therefore decided on stenting.
ConclusionIn cases of non-recanalisable ipsilateral ICA, endovascular treatment of MCA occlusion may be performed via the contralateral carotid artery when the anatomical configuration of the ACoAs and ACAs is favourable.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Pérez Montilla ME, Bravo Rey IM, Bautista Rodríguez MD, Alvarado SV, Bravo-Rodríguez FA, Delgado Acosta F. Oclusión aguda de aneurisma gigante de arteria carótida interna: Recanalización de la arteria cerebral media a través de la arteria carótida contralateral. Neurología. 2017;32:480–484.