Epilepsia partialis continua (EPC) is characterised by spontaneous regular or irregular clonic movements of a specific part of the body and affecting facial muscles or distal muscles of the limbs especially, although they may also affect the chest or abdomen. These movements may be continuous or appear in recurrent intervals of a few seconds for at least 1hour and up to several days or weeks, and they may be aggravated by activity or external stimuli.1,2 Jerking movements affect agonist and antagonist muscles simultaneously. Although patients usually remain conscious, they often display marked postictal weakness. Epileptic activity in EPC is generated in the motor cortex or adjacent areas.3,4
In children, the most frequent cause of EPC is Rasmussen encephalitis; other causes include tumours, vascular lesions, infections, and metabolic disorders. In the past years, the number of patients with EPC due to cortical dysplasia (CD) has increased.5,6 We present a case of focal CD manifesting as EPC.
Clinical caseMedical history and prodromeOur patient was a 3-year-old boy with no medical history of interest except for non-isoimmune neonatal jaundice, which required no phototherapy. He displayed normal psychomotor development. According to his parents, 3 weeks before symptom onset, our patient had displayed behavioural changes (irritability with no apparent cause) and slept more hours than usual. One week before symptom onset he showed symptoms of viral infection and common cold and experienced nausea but was afebrile.
SymptomsHe was brought to hospital due to an episode of right-sided deviation of head and eyes and head nodding lasting a few seconds. On the same day, he experienced a similar episode while awake and another while asleep. During this last episode, he sat up with his upper limbs in flexion and displayed right-sided deviation of head and eyes and head clonus, which resolved spontaneously after a few seconds. After this episode, our patient fell onto his back and was drowsy. The frequency of these episodes increased in the following days.
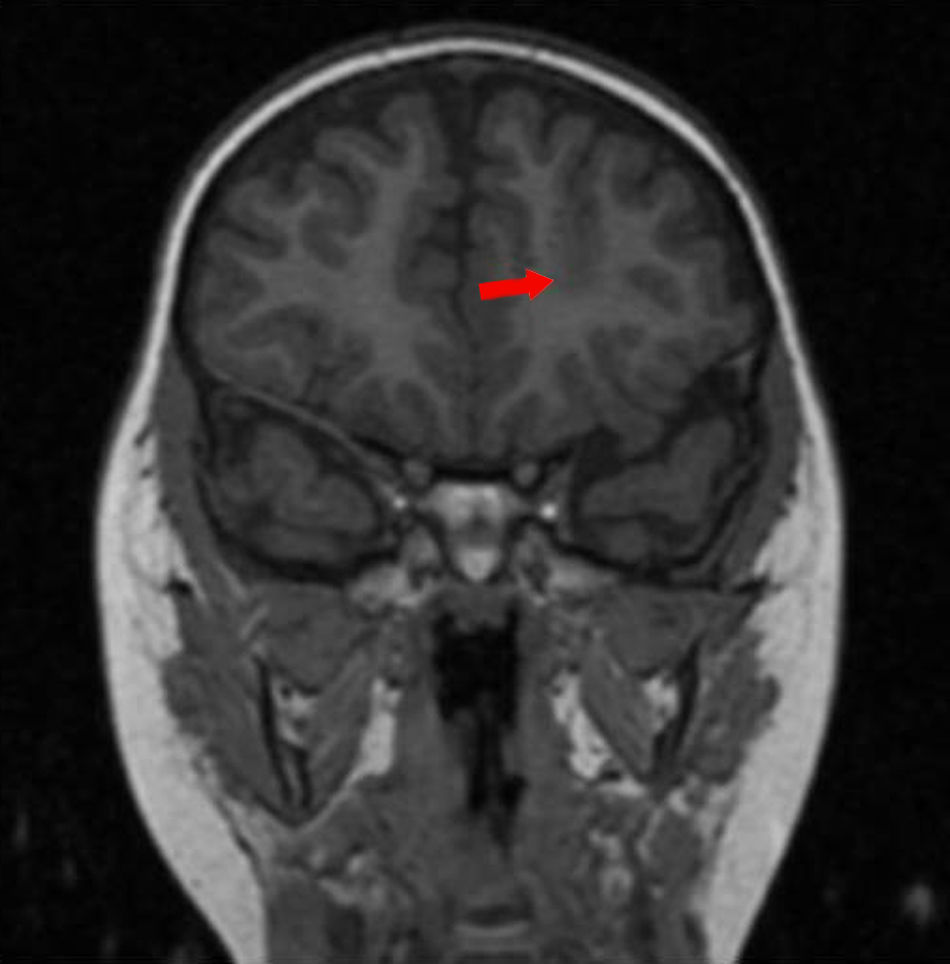
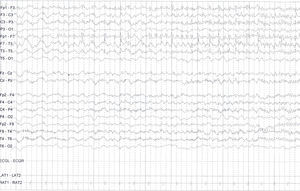
Treatment and progressionWe started treatment with valproic acid and subsequently added intravenous levetiracetam and phenytoin. However, seizures increased and became continuous. At this point, our patient received midazolam infusion and was put into a barbiturate-induced coma for seizure control. In addition to these measures, our patient began a ketogenic diet. He also received intravenous lacosamide, which led to a decrease in the number of seizures. The video-EEG trace, however, revealed epileptiform activity which was nearly continuous in the frontal region of the left hemisphere and maximal in the frontopolar region; signs of focal motor status epilepticus were seen in the oro-lingual-facial region and the right hand. These findings were compatible with EPC (Fig. 1). We conducted several complementary tests to determine the cause of EPC (serology test, tests for neurotropic viruses and oligoclonal bands in CSF, test for serum and CSF NMDA-receptor antibodies, metabolic study, karyotyping, and MRI on 2 occasions); test results were all normal. A subsequent 3-T MRI scan revealed findings suggestive of focal dysplasia at the bottom of the left superior frontal sulcus; the PET scan displayed hypermetabolism in that area (Fig. 2).
Given that our patient had drug-resistant epilepsy, we opted for emergency surgery. We performed left frontal lobectomy to remove the area displaying CD. The anatomical pathology study confirmed the presence of type IIa focal CD.
A follow-up MRI scan performed 6 months after surgery revealed no remnants of dysplastic tissue. The patient was seizure-free. At our most recent follow-up consultation, he was receiving a single antiepileptic agent.
DiscussionImprovements in neuroimaging and the development of 3-T MRI have opened up new possibilities for diagnosing some lesions, such as CD, which cannot be detected using conventional MRI.
As demonstrated by our patient, surgery during the acute phase may be an effective treatment approach in cases of drug-resistant epilepsy secondary to localised lesions.
Please cite this article as: Castaño de la Mota C, Conejo Moreno D, García Fernández M, García Peñas JJ. Displasia cortical focal en paciente de 3 años con epilepsia parcial continua. Neurología. 2017;32:478–480.
Clinical case presented in a moderated poster session at the 35th Annual Meeting of the Spanish Society of Paediatric Neurology, held in Granada, Spain.