Attention deficit hyperactivity disorder (ADHD) is a neuropsychiatric disorder originating from multiple factors. The aim of this study is to determine the percentage of patients with ADHD out of all patients referred to our clinic for assessment, and to explore the epidemiological and clinical factors linked to this diagnosis.
Patients and methodsRetrospective analytical study of a sample of patients under 15 years old sent to the paediatric neurology clinic for suspected ADHD. DSM-IV criteria were used for diagnosis. We completed a binary logistic regression analysis to determine which risk factors were associated with the diagnosis.
ResultsOf the 280 selected patients, 224 were male (male/female ratio 4:1); mean age (SD) was 8.4 (3.08) years. Almost half (49%) of the patients were referred by their schools and 64.9% were born in the second half of the year, but this tendency was more marked in girls than in boys. Assessment according to DSM-IV criteria resulted in diagnosis of 139 subjects (49.7%). The risk factors linked to diagnosis were male sex, parents with ADHD, associated sleep disorders, tics, and absence of neurodevelopmental delay.
ConclusionOnly half of the children referred for suspected ADHD were diagnosed with that condition, and most were among the youngest in their classes, which suggests that suspected ADHD is overestimated. An exhaustive clinical interview investigating the family's psychological disorders and the patient's sleep disorders and tics is needed to improve the diagnostic process.
El trastorno por déficit de atención e hiperactividad (TDAH) es un trastorno neuropsiquiátrico de origen multifactorial. El objetivo de este estudio es determinar el porcentaje de pacientes que presentan TDAH del global de los enviados a la consulta por este motivo, y explorar los factores epidemiológicos y clínicos asociados al diagnóstico.
Pacientes y métodosEstudio retrospectivo analítico de una muestra de pacientes derivados a la consulta de neuropediatría por sospecha de TDAH, a la que se le aplican los criterios diagnósticos del DSM-IV. Se realiza un análisis de regresión logística para explorar los factores asociados al diagnóstico.
ResultadosDe los 280 pacientes, 224 eran varones (relación niños/niñas 4/1) con una edad media ± desviación estándar de 8,4±3,08 años. El 49% fue remitido desde el ámbito escolar. El 64,9% de ellos nacieron en el segundo semestre del año, fenómeno que es más acusado en las mujeres. Tras la evaluación de los sujetos, un total de 139 casos fueron diagnosticados (49,7%). Los factores asociados a un incremento de diagnósticos de TDAH fueron: el sexo varón, el TDAH parental, trastornos del sueño asociados, la presencia de tics y la ausencia de retraso del desarrollo psicomotor.
ConclusionesSolo la mitad de los niños enviados con sospecha de TDAH fueron diagnosticados del trastorno. La mayoría se encuentra entre los más jóvenes del curso escolar, sugiriendo una sobreestimación de la sospecha. Una entrevista clínica donde se explore la psicopatología parental, los trastornos del sueño y los tics parece necesaria para mejorar el proceso diagnóstico.
The number of patients diagnosed with attention-deficit/hyperactivity disorder (ADHD), and consequently the consumption of medications for the condition, has increased in many countries. At present, ADHD is the most frequent neuropsychiatric disorder among paediatric patients and poses a major public health problem.1 According to the literature, prevalence of ADHD ranges from 2.2% to 17.8%. Such a pronounced variation in prevalence rates may be explained by a number of factors: differences in the sources of information used for diagnosis (parents, teachers, or healthcare professionals), diagnosis based on the presence of behavioural disorders in one or more fields, the study methodology (DSM or ICD criteria), and ethnic and cultural differences in study samples.2 In Spain, studies report prevalence rates of ADHD between 0.2% and 15%. A systematic review and meta-analysis of epidemiological studies conducted in Spain reported an overall pooled prevalence rate of 6.8%.3
The fact that the rates published in the literature are high and vary between studies may indicate misdiagnosis or lack of precision in diagnosis. The aetiology of ADHD is heterogeneous and involves numerous genetic and environmental factors. Knowing the underlying causes of ADHD improves diagnosis. ADHD has been found to have a highly heritable component; this, combined with perinatal (low birthweight, pre-term birth, hypoxia, maternal substance abuse during pregnancy), environmental, and psychosocial factors (poverty, mistreatment, stress), has a considerable impact on a child's neurodevelopment and the pathogenesis of the disease. Several studies have shown that the risk of ADHD diagnosis is higher in young-for-grade children.4–7 According to these studies, children born in the month previous to the cut-off date of birth for starting school are more likely to be diagnosed with ADHD and are more frequently prescribed methylphenidate than those born in the months following the cut-off date.
The purpose of this study was to determine the percentage of patients referred to the paediatric neurology department with suspected ADHD who are finally diagnosed with ADHD after thorough assessment. Furthermore, we aimed to determine the comorbidities and family and psychosocial factors associated with this condition. Likewise, we analysed whether children diagnosed with ADHD were more frequently born during the second semester, given that the cut-off date for starting school in Spain is 1 January.
Patients and methodsWe conducted a retrospective analysis of a cohort of patients referred to a paediatric neurology department with suspected ADHD and analysed clinical variables associated with diagnosis. We included all patients aged under 15 who were referred to the paediatric neurology department at Hospital de Sagunto, in the region of Valencia, Spain. This is the only hospital in its health district. Consultations were held by the same paediatric neurology specialist during the entire study period. We selected a sample of children with suspected ADHD and classified them in 2 groups: patients diagnosed with ADHD and patients without ADHD. Patients were diagnosed with ADHD if they met the diagnostic criteria for ADHD established in the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV). Our sample was selected by consecutive sampling; we included the last 280 records (December 2012 backwards) given that more recent records provide more detailed information and data on a greater number of variables. The patients selected correspond to a period of 4 years. The main variable was number/percentage of patients diagnosed with ADHD out of the total of patients referred to the paediatric neurology department. In order to analyse the risk of being diagnosed with ADHD, we gathered clinical and demographic variables associated with increased risk of ADHD according to the literature, as well as any other comorbidities that may coexist with the condition. To this end, we conducted a thorough literature review spanning the last 20 years. We gathered the following variables from clinical histories:
- 1.
Age at diagnosis
- 2.
Sex
- 3.
Date of birth
- 4.
Healthcare level referring the patient (primary care, specialised paediatric department, child and adolescent mental health units [CAMHU], school, or parents)
- 5.
Parental history of:
- –
Somatic disorders
- –
Psychiatric diseases
- –
ADHD
- –
- 6.
Family conflicts, violence in the family setting, divorce, loss of loved ones
- 7.
Perinatal complications associated with increased risk of ADHD:
- –
Low birthweight and pre-term birth
- –
Substance abuse during pregnancy: tobacco, heroin, cocaine, other drugs
- –
Those problems involving the separation of mother and infant for more than one day were considered perinatal complications.
- –
- 8.
Hypoxic–ischaemic encephalopathy, head trauma, epilepsy, and some infections (encephalitis); these conditions have been associated with ADHD
- 9.
Delayed psychomotor development (problems in achieving motor or cognitive developmental milestones; diagnosis by a healthcare professional)
- 10.
Mental retardation (according to a normalised intelligence test evaluating IQ and competence in several areas; IQ<70 was classified as mental retardation).
- 11.
Presence of several comorbidities in ADHD patients, including:
- –
Behavioural disorders
- –
Anxiety disorders
- –
Sleep disorders
- –
Language disorders
- –
Learning disorders
- –
Tics
- –
- 12.
Allergies
- 13.
History of child abuse
- 14.
Sensory alterations (visual deficits and/or hypoacusis)
- 15.
Deterioration or malnutrition
- 16.
Epilepsy (diagnosed by a neurologist)
- 17.
Sleep disorders
We determined whether children diagnosed with ADHD were more frequently born in the second semester. To this end, we recoded the variable date of birth into months, trimesters, and semesters.
Categorical variables were expressed as numbers and percentages of patients for each category. Quantitative variables were expressed as measures of central tendency (means) and dispersion (standard deviation).
A bivariate analysis of data was conducted using the main and secondary variables gathered from our literature review to determine the factors associated with ADHD. We used the chi-square test with statistical significance set at P<.05. The Fisher exact test was used when the data set for a variable was too small. The t test for independent samples was used for age (quantitative variable); P-values <.05 were considered statistically significant. We subsequently conducted a multivariate analysis using binary logistic regression; the model included all those variables which had shown a significant association with ADHD in the bivariate analysis, as well as those which were marginally significant yet clinically relevant. Associations between variables were also analysed.
Sample size was calculated using the GRANMO freeware.8 The prevalence of ADHD in the region of Valencia is estimated at 5%. A random sample of 270 patients was therefore necessary to estimate a sample proportion of 60% with a 95% confidence level and a 5% margin of error. We sampled without replacement. According to Spain's National Statistics Institute, the health district of Sagunto includes 20000 paediatric patients (below the age of 15).9
Data were analysed using SPSS statistical software version 21.0.
Our study complies with the international laws regulating epidemiological studies included in the International Guidelines for Ethical Review of Epidemiological Studies (Council for the International Organizations of Medical Sciences, Geneva, 1991) and the recommendations published by the Spanish Society of Epidemiology on the ethical review of epidemiological research. This study was approved by the ethics committee at Hospital de Sagunto in October 2013.
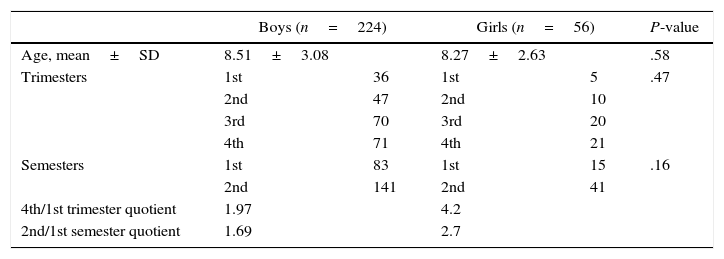
ResultsOur sample included 280 paediatric patients, 224 of whom were boys (male/female ratio of 4:1). Mean age at the time of consultation was 8.4±3.08 years. Table 1 summarises patients’ sociodemographic characteristics. No statistically significant differences were observed in mean age between boys and girls (t(276)=0.54; P=.58). More than half of the patients were born in the second semester, as shown in Table 1. This difference is more marked among girls: the number of girls born in the last trimester of the year is 4 times higher than that of girls born in the first trimester.
Sociodemographic characteristics of our sample (N=280).
| Boys (n=224) | Girls (n=56) | P-value | |||
|---|---|---|---|---|---|
| Age, mean±SD | 8.51±3.08 | 8.27±2.63 | .58 | ||
| Trimesters | 1st | 36 | 1st | 5 | .47 |
| 2nd | 47 | 2nd | 10 | ||
| 3rd | 70 | 3rd | 20 | ||
| 4th | 71 | 4th | 21 | ||
| Semesters | 1st | 83 | 1st | 15 | .16 |
| 2nd | 141 | 2nd | 41 | ||
| 4th/1st trimester quotient | 1.97 | 4.2 | |||
| 2nd/1st semester quotient | 1.69 | 2.7 | |||
Around 49% of the patients visited the paediatric neurology department at their school's request, whereas 33% were referred by primary care doctors, 8% by CAMHU, and 8% visited the paediatric neurology department due to parental concern.
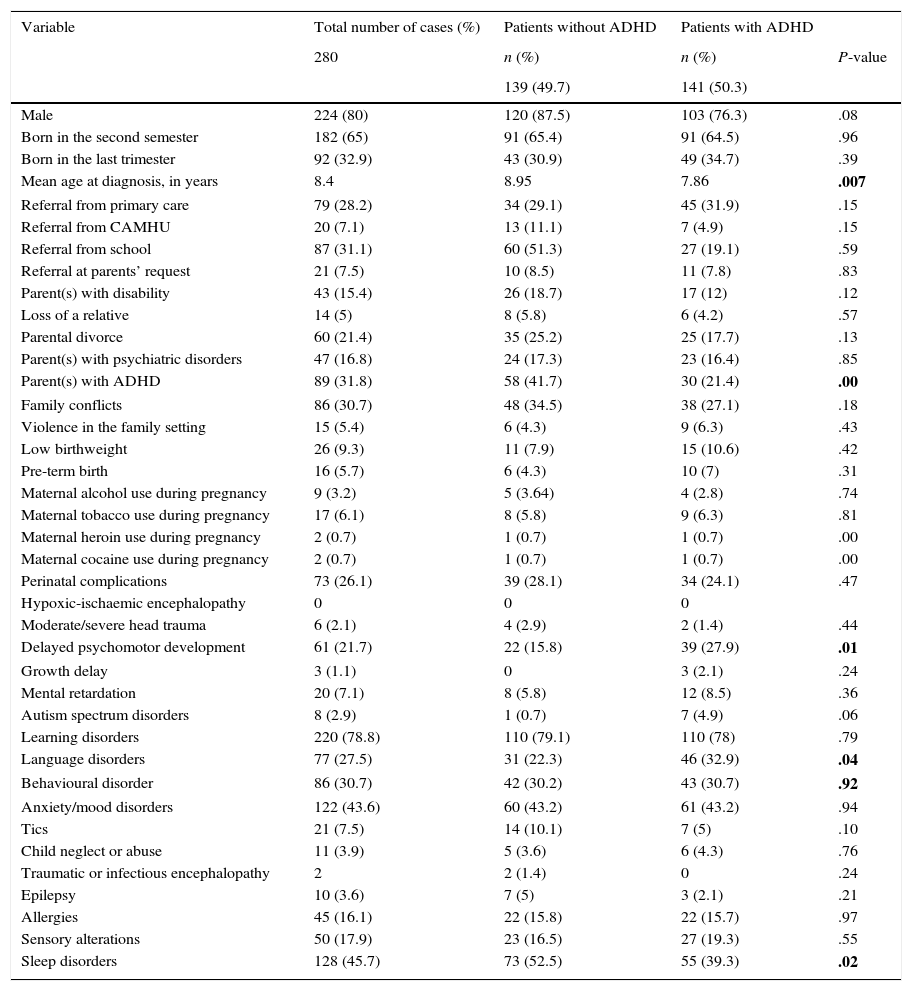
We gathered clinical and demographic data corresponding to the 38 variables analysed (Table 2).
Variables potentially associated with ADHD in our sample.
| Variable | Total number of cases (%) | Patients without ADHD | Patients with ADHD | |
|---|---|---|---|---|
| 280 | n (%) | n (%) | P-value | |
| 139 (49.7) | 141 (50.3) | |||
| Male | 224 (80) | 120 (87.5) | 103 (76.3) | .08 |
| Born in the second semester | 182 (65) | 91 (65.4) | 91 (64.5) | .96 |
| Born in the last trimester | 92 (32.9) | 43 (30.9) | 49 (34.7) | .39 |
| Mean age at diagnosis, in years | 8.4 | 8.95 | 7.86 | .007 |
| Referral from primary care | 79 (28.2) | 34 (29.1) | 45 (31.9) | .15 |
| Referral from CAMHU | 20 (7.1) | 13 (11.1) | 7 (4.9) | .15 |
| Referral from school | 87 (31.1) | 60 (51.3) | 27 (19.1) | .59 |
| Referral at parents’ request | 21 (7.5) | 10 (8.5) | 11 (7.8) | .83 |
| Parent(s) with disability | 43 (15.4) | 26 (18.7) | 17 (12) | .12 |
| Loss of a relative | 14 (5) | 8 (5.8) | 6 (4.2) | .57 |
| Parental divorce | 60 (21.4) | 35 (25.2) | 25 (17.7) | .13 |
| Parent(s) with psychiatric disorders | 47 (16.8) | 24 (17.3) | 23 (16.4) | .85 |
| Parent(s) with ADHD | 89 (31.8) | 58 (41.7) | 30 (21.4) | .00 |
| Family conflicts | 86 (30.7) | 48 (34.5) | 38 (27.1) | .18 |
| Violence in the family setting | 15 (5.4) | 6 (4.3) | 9 (6.3) | .43 |
| Low birthweight | 26 (9.3) | 11 (7.9) | 15 (10.6) | .42 |
| Pre-term birth | 16 (5.7) | 6 (4.3) | 10 (7) | .31 |
| Maternal alcohol use during pregnancy | 9 (3.2) | 5 (3.64) | 4 (2.8) | .74 |
| Maternal tobacco use during pregnancy | 17 (6.1) | 8 (5.8) | 9 (6.3) | .81 |
| Maternal heroin use during pregnancy | 2 (0.7) | 1 (0.7) | 1 (0.7) | .00 |
| Maternal cocaine use during pregnancy | 2 (0.7) | 1 (0.7) | 1 (0.7) | .00 |
| Perinatal complications | 73 (26.1) | 39 (28.1) | 34 (24.1) | .47 |
| Hypoxic-ischaemic encephalopathy | 0 | 0 | 0 | |
| Moderate/severe head trauma | 6 (2.1) | 4 (2.9) | 2 (1.4) | .44 |
| Delayed psychomotor development | 61 (21.7) | 22 (15.8) | 39 (27.9) | .01 |
| Growth delay | 3 (1.1) | 0 | 3 (2.1) | .24 |
| Mental retardation | 20 (7.1) | 8 (5.8) | 12 (8.5) | .36 |
| Autism spectrum disorders | 8 (2.9) | 1 (0.7) | 7 (4.9) | .06 |
| Learning disorders | 220 (78.8) | 110 (79.1) | 110 (78) | .79 |
| Language disorders | 77 (27.5) | 31 (22.3) | 46 (32.9) | .04 |
| Behavioural disorder | 86 (30.7) | 42 (30.2) | 43 (30.7) | .92 |
| Anxiety/mood disorders | 122 (43.6) | 60 (43.2) | 61 (43.2) | .94 |
| Tics | 21 (7.5) | 14 (10.1) | 7 (5) | .10 |
| Child neglect or abuse | 11 (3.9) | 5 (3.6) | 6 (4.3) | .76 |
| Traumatic or infectious encephalopathy | 2 | 2 (1.4) | 0 | .24 |
| Epilepsy | 10 (3.6) | 7 (5) | 3 (2.1) | .21 |
| Allergies | 45 (16.1) | 22 (15.8) | 22 (15.7) | .97 |
| Sensory alterations | 50 (17.9) | 23 (16.5) | 27 (19.3) | .55 |
| Sleep disorders | 128 (45.7) | 73 (52.5) | 55 (39.3) | .02 |
Statistically significant values are shown in bold.
After assessment, 49.7% of the patients (n=139) were diagnosed with ADHD. The remaining patients were either diagnosed with other conditions or found not to have ADHD at the time of assessment.
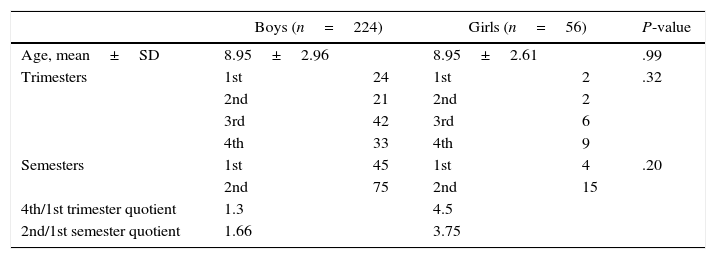
Inter-sex differences were more marked and patients were older in the ADHD group; 87.5% were boys, with a mean age of 8.95±2.96 years. The male/female ratio in the ADHD group is 6:1. The sociodemographic characteristics of our sample are shown in Table 3.
Sociodemographic characteristics of our sample.
| Boys (n=224) | Girls (n=56) | P-value | |||
|---|---|---|---|---|---|
| Age, mean±SD | 8.95±2.96 | 8.95±2.61 | .99 | ||
| Trimesters | 1st | 24 | 1st | 2 | .32 |
| 2nd | 21 | 2nd | 2 | ||
| 3rd | 42 | 3rd | 6 | ||
| 4th | 33 | 4th | 9 | ||
| Semesters | 1st | 45 | 1st | 4 | .20 |
| 2nd | 75 | 2nd | 15 | ||
| 4th/1st trimester quotient | 1.3 | 4.5 | |||
| 2nd/1st semester quotient | 1.66 | 3.75 | |||
Sixty-five percent of the patients in the ADHD group were born in the second semester (65%). In our sample, patients with ADHD were more frequently born in the last months of the year; differences between the first and the second semester of the year were particularly marked in girls. However, date of birth had no discriminant ability for ADHD, given that differences between patients with and without a diagnosis of ADHD were not statistically significant either for semesters or trimesters.
Patients without ADHD had a lower mean age than those with ADHD (7.86 vs 8.95 years). The difference of means (DM) was statistically significant (DM=1.09 [95% CI, 0.37-1.80], P=.03).
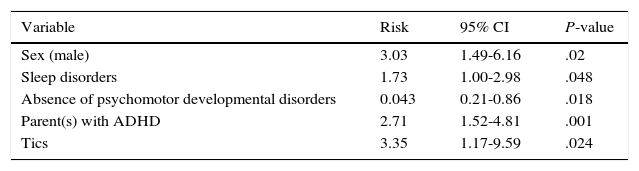
The multivariate analysis of the factors associated with ADHD diagnosis included the following variables: sex, parent(s) with ADHD, delayed psychomotor development, autism spectrum disorders (ASD), learning disorders, language disorders, parent(s) with disability, parent(s) with psychiatric disorders, parental divorce, tics, and sleep disorders. The following factors were found to have a significant association with ADHD rather than any other disorder: male sex, parent(s) with ADHD, sleep disorders, absence of psychomotor developmental disorders, and tics. Results are detailed in Table 4.
The variables parents with psychiatric disorders (OR 2.25; 95% CI, 0.94-5.4) and parental divorce (OR 1.94; 95% CI, 0.92-4.06) nearly reached statistical significance.
DiscussionAccording to our results, less than half of the patients referred to the paediatric neurology department with suspected ADHD are eventually diagnosed with ADHD. Though apparently low, this figure is significantly higher than those reported in other studies conducted in Spanish populations; according to these studies, only 20% of patients with suspected ADHD are diagnosed with the disorder.10,11 In these studies, diagnosis of suspected ADHD by primary care doctors behaved as a screening test; less than 25% of these patients were finally diagnosed with ADHD by mental health specialists. The above suggests that there is a high level of suspicion of ADHD in all settings, probably due to parental and school concern about the disease, extensive information available on the Internet, and the increasing demand for primary care consultations.11 In light of these data, diagnosis by primary care doctors may serve as a screening tool, whereas child and adolescent mental health specialists or paediatric neurologists should provide the definitive diagnosis. A limitation to this study is the fact that primary care paediatricians may refer patients with suspected ADHD to the paediatric neurology department or the psychiatrist at the CAMHU. Therefore, we do not know whether patients attending CAMHUs show similar results, given that their medical histories are not recorded in the hospital's database. Furthermore, the DSM criteria are less restrictive than those of the ICD-10; if we had used the latter, the number of patients with a definitive diagnosis of ADHD would have been lower.
Our results point to an association between date of birth and ADHD, both in the entire sample of patients with suspected ADHD and in the subgroup of patients with a diagnosis of ADHD. This phenomenon had not previously been reported in Spain. Likewise, seasonality was more marked in girls, with a 2nd/1st semester quotient of 3.75. This quotient value is considerably high, although we must be mindful of the small number of girls diagnosed with ADHD in our sample (19). However, this finding has been reported in previous studies and is therefore consistent with the literature.6 A possible explanation for this phenomenon is that attention is a developmental process. Attention as a cognitive function develops progressively from infancy and is greatly influenced by a child's interaction with his or her mother/carer and multiple environmental stimuli. Inattentive type ADHD is more frequent in girls. We hypothesise that inattention in younger and cognitively immature girls leads to more consultations with healthcare professionals than in the case of boys.
This finding is in line with the literature: according to several studies in North American and Northern European populations,5,6,12 hyperactivity and inattention are more frequent in children who are biologically more immature. As a result, young-for-grade children are more likely to be diagnosed with suspected ADHD. Schools play an essential role in diagnosing ADHD, given that poor school performance and dysfunctional behaviour in class are key aspects in suspecting ADHD. No biological factors have been found to explain the greater number of births of children with ADHD during a specific period of the year.
Regarding the factors associated with ADHD diagnosis, genetics seems to play an essential role: according to our results, the risk of ADHD increases considerably when at least one of the parents has been diagnosed with the disorder. This finding is consistent with the results of other studies analysing the heritability of ADHD, which has been estimated to reach almost 80%.13 Gathering the patient's clinical history and data on the parents’ psychological disorders is therefore essential. Little is currently known about ADHD in adulthood; as a result, a large percentage of parents may have not been diagnosed with the disorder. According to a recent study in the European population, very few adults are diagnosed with and consequently receive treatment for ADHD.14 On many occasions, the multiple comorbidities these patients present may interfere with ADHD diagnosis and proper management.14,15 Gathering data on school performance, impulsivity, potential substance addiction, and presence of clear symptoms of ADHD during childhood is therefore highly recommended. ADHD is currently being studied in adult populations, which has resulted in an increase in the number of adults diagnosed with the condition. For example, numerous cases of ADHD are being detected among adults diagnosed with substance use disorders (40%, according to a recent international study16). This is also the case with eating disorders; a study in the Spanish population, including 191 women with eating disorders, found a high prevalence of symptoms of ADHD, especially in those women with more severe eating disorders.17 Presence of psychiatric disorders in a child's parents may help in diagnosis, given that a family history of ADHD leads to a two-fold increase in the risk of ADHD.
According to our results, a parental history of ADHD and male sex are the variables with the greatest predictive ability for ADHD. ADHD is widely recognised to be more frequent in boys than in girls, with sex ratios ranging from 2.5:1 to 5.6:1.18 Symptoms also vary between sexes: combined-type ADHD is more common in boys whereas girls tend to display inattentive-type ADHD more frequently (impulsivity and hyperactivity may be less marked in these patients).
The high rate of divorce in families with children with ADHD is interesting to note (25% vs 17% in children without ADHD); nevertheless, differences between children with and without ADHD were not statistically significant. According to Spain's National Statistics Institute, 3 out of every 4 marriages end in divorce in Spain. However, the number of divorces has decreased since 2010, probably due to the economic crisis.19,20 In light of these data, we cannot state that the rate of parental divorce in the ADHD group is higher than that of the general population; however, rates were considerably different between groups. Regarding this variable, we may speculate about the impact of family relationships on the origin of certain behaviours in children, and even in their parents (adults with ADHD tend to have more conflictive relationships). The high rate of conflicts among families of patients with ADHD is noteworthy (nearly 34%). This rate, however, may be even higher, since the family conflicts variable was recorded as positive only when patients’ histories explicitly reported poor family relationships for a sustained period of time; this constitutes another limitation of our study.
It would have been interesting to gather data on the parents’ education level, economic status, and employment status to analyse the potential impact of these variables on the presence of ADHD. In fact, social adversity has been suggested to be a predisposing factor for ADHD.21 However, these data are not systematically included in patients’ medical histories.
There is evidence to support the association between maternal substance abuse during pregnancy (tobacco and other substances) and presence of ADHD in children.22,23 Our study, however, failed to demonstrate this association, due to methodological limitations inherent to its retrospective design. At present, maternal substance abuse during pregnancy is not systematically recorded. Likewise, special emphasis should be placed on smoking cessation during pregnancy due to the widespread consumption of tobacco. In a prospective cohort study conducted in the region of Valencia in 2004, aiming to determine the causes of early weaning, 30% of the mothers included were smokers.24 Based on the above, the rate of patients whose mothers smoked during pregnancy may be underestimated in our sample (6.1%). Scientific evidence suggests that prenatal exposure to nicotine is one of the most important risk factors for ADHD and other learning disorders.25
Likewise, the low prevalence of pre-term birth, low birthweight, head trauma, and hypoxic-ischaemic encephalopathy in our sample did not allow us to analyse the association between these variables and ADHD. A much larger sample size would be necessary to demonstrate this association, which has been widely reported in the literature.26–28
In our study, tics and sleep disorders, 2 known comorbidities of ADHD, were found to be associated with the condition. According to our statistical analysis, sleep disorders had only a weak correlation with ADHD; this association, however, has previously been reported in the literature, which supports our results. Children with ADHD are 2-3 times more likely to experience sleep disorders than healthy children. Furthermore, sleep disorders in these patients may be aggravated by treatment with stimulants, although this effect is yet to be confirmed. In fact, a recent study of a sample of 114 Spanish children with ADHD treated with methylphenidate reported improvements in enuresis, somnambulism, and night waking at 6 months.29 ADHD has a negative impact on children and their families; these children usually display bedtime resistance and daytime fatigue and somnolence.30 Assessing sleep patterns and treating insomnia and comorbidities in these patients is essential; relaxation techniques and stricter bedtime schedules are especially useful for this purpose. These findings are in line with our own: binary logistic regression analysis found an association between sleep disorders and anxiety/depression.
Evaluating these children's sleep habits and their families’ coping strategies is necessary to gain a better understanding of the disorder and to manage each case accordingly. Presence of anxiety symptoms, behaviour problems, and depression should also be assessed, since these seem to be closely linked to ADHD.
The same is true for tics. Multiple studies have found an association between tics and ADHD, even in adulthood. In our study, 10.1% of the children with ADHD experienced tics. This variable is less precise, as it is associated with a wide confidence interval. However, our results seem to be reliable, given that tics have also been associated with ADHD in previous studies, with prevalence rates around 10.9%.31
The high level of comorbidity of learning disorders in our sample is noteworthy (79%); this percentage is higher than those reported in other studies, with rates ranging from 8% to 39% for reading disorders and around 30% for dyscalculia.23 The prevalence rate of language disorders in our sample (22.3%) was in turn lower than those reported by other studies.23 These differences may be due to the size and characteristics of our sample. Learning and language disorders were not found to have discriminant ability for differentiating between patients with and without ADHD; however, the high prevalence of these disorders in ADHD patients is relevant in that these conditions may worsen school performance and family relationships.
In our study, children without ADHD were more likely to display psychomotor developmental disorders, especially delayed motor coordination and delayed acquisition of developmental milestones within the first 2 years. Children with psychomotor developmental disorders may present a condition other than ADHD; presence of these disorders may therefore indicate that the patient does not have ADHD.
It would have been interesting to analyse the impact of culture on children's behaviour. One of the limitations of our study is that we did not gather data about the country of origin or cultural background of patients in our sample. Culture has a major impact on a child's development and plays an important role in the pathogenesis of numerous psychological disorders. Expectations about a child's performance and normal behaviour vary between countries.32
Our study underscores the need for a multidisciplinary approach to these patients in order to avoid misdiagnosis. We should be aware that young-for-grade children may display more learning difficulties than their peers and are therefore more likely to be referred for assessment of suspected ADHD. This is linked to a high level of comorbidity of learning and language disorders, behavioural problems, and sleep disorders. We also recommend analysing the child's parental history of psychiatric disorders, especially ADHD, given that this condition is highly heritable. ADHD has occasionally been associated with family problems; therefore, the family setting is a fundamental pillar in ADHD management in terms of both diagnosis and treatment.
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to thank Diana Aspas, Sergio Fernández, and Marta Aguar for their help in data collection, data analysis, and statistical analysis, respectively.
Please cite this article as: Rivas-Juesas C, de Dios JG, Benac-Prefaci M, Colomer-Revuelta J. Análisis de los factores ligados al diagnóstico del trastorno por déficit de atención e hiperactividad en la infancia. Neurología. 2017;32:431–439.