Hypnic headache is a rare primary headache. The diagnostic criteria of the International Headache Classification (IHS) for this condition are discussed, as they have been modified in the new edition of the 2013.
Patients and methodsThe clinical characteristics, and fulfilment of the criteria of the IHS classification in a series of 10patients diagnosed in our Headaches Clinic, are analysed.
ResultsThe mean age of onset of symptoms was 52.1years (SD: 13.4; range: 28–69). The pain was reported as oppressive in 60% of the patients, and as sharp in 30%. The headache was described as holocranial in 60% and hemicranial in 40%. They occurred exclusively during night-time sleep in 80% of the patients. The mean duration of headache was 136.5minutes (range: 10–480). The mean number of days per month was 16.4 (range: 3–30), and 50% had less than 15 headache days per month. No patient had autonomic manifestations, 70% had phonophobia, 50% had photophobia, and 50% had both. All of them (100%) had a VAS score equal to or higher than 8.
ConclusionsThe criteria for hypnic headache of the new classification are best suited to the characteristics of these patients. Our results show the major changes in the criteria: pain is not always dull, headache frequency may be less than 15days a month, and it can occur in people under age 50. There may be phonophobia or photophobia only, or both. Although it does not form part of the diagnostic criteria, the pain intensity in our series was higher than described.
La cefalea hípnica es una cefalea primaria poco frecuente. Los criterios diagnósticos de la Clasificación Internacional de Cefaleas (CIC) para esta entidad han sido discutidos, por lo que en la nueva edición de la CIC de 2013 se han modificado.
Pacientes y métodosAnalizamos las características clínicas y la adecuación a los criterios de la CIC de una serie de 10pacientes diagnosticados en nuestra consulta de cefaleas.
ResultadosLa edad media de inicio del cuadro fue 52,1años (DE: 13,4; rango: 28–69). El 60% de nuestros pacientes describían el dolor como opresivo y el 30% como punzante. En el 60% es holocraneal y en el 40% es hemicraneal. Al 80% les ocurre exclusivamente durante el sueño nocturno. La duración media de la cefalea es de 136,5min (rango: 10–480). La media de días al mes es de 16.4 (rango: 3–30) y el 50% presentaron cefalea menos de 15días al mes. Ningún paciente presentó manifestaciones autonómicas, el 70% presentó sonofobia y el 50% fotofobia. El 50% presentó ambas. El 100% puntuó la intensidad en la escala VAS igual o superior a 8.
ConclusionesLos criterios para cefalea hípnica de la nueva CIC se adecuan mejor a las características de estos pacientes. Nuestros resultados reflejan los principales cambios en los criterios: el dolor no siempre es sordo, puede aparecer menos de 15días al mes y en personas de menos de50 años. Puede existir sonofobia y fotofobia y no solo uno de ellos. Aunque no forma parte de los criterios diagnósticos, nos ha llamado la atención que en nuestra serie la intensidad es mayor a la descrita.
Hypnic headache (HH) is a rare primary headache that affects mainly middle-aged or elderly patients. Its main distinguishing characteristic is that it manifests only during sleep and awakens the patient (alarm-clock headache).1 Different published case series report considerable variations in prevalence, ranging from 0.07% to 0.3% in a specialised headache clinic.2,3
HH was first described in 1988 by Raskin,4 who reported a series of 6 patients whose nocturnal sleep was regularly interrupted by a night-time headache, almost always at the same time. None of these cases presented autonomic syndromes. All patients were older than 65 at the time, and their headaches were therefore late-onset syndromes.
In 1997, Goadsby and Lipton5 proposed clinical diagnostic criteria for HH that would include episode frequency of more than 15 days per month during one month and paucity of autonomic features.
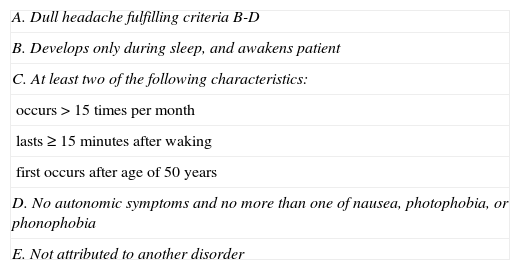
In 2004, the second edition of the International Classification of Headache Disorders (ICHD-2)6 included HH in group 4 (other primary headaches) and established diagnostic criteria for this entity (Table 1).
Diagnostic criteria for hypnic headache according to the second edition of the International Classification of Headache Disorders6
| A. Dull headache fulfilling criteria B-D |
| B. Develops only during sleep, and awakens patient |
| C. At least two of the following characteristics: |
| occurs>15 times per month |
| lasts≥15minutes after waking |
| first occurs after age of 50 years |
| D. No autonomic symptoms and no more than one of nausea, photophobia, or phonophobia |
| E. Not attributed to another disorder |
Approximately 150 cases of HH have been described and published in the literature to date. The increase in the number of reported HH cases has led us to reconsider the suitability of ICHD-2 diagnostic criteria given the clinical characteristics of these patients. This topic is of increasing interest as we can see by reviewing the latest articles on this subject.
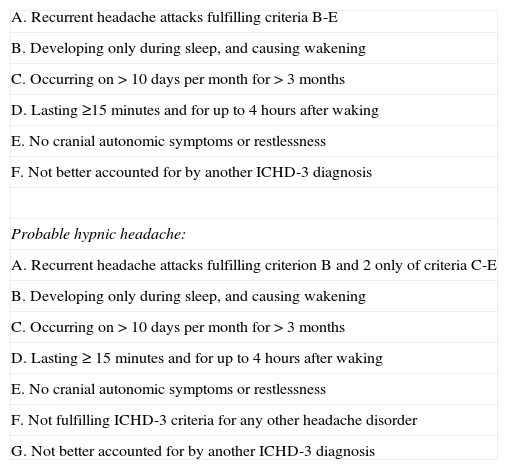
The third edition of the International Classification of Headache Disorders (ICHD-3)7 was published recently. In addition to including modifications in the diagnostic criteria for this entity, it also introduces the concept of ‘probable hypnic headache’, which reflects the difficulty of diagnosing HH in clinical practice due to the variability of its clinical symptoms (Table 2).
Diagnostic criteria for hypnic headache according to the third edition of the International Classification of Headache Disorders7
| A. Recurrent headache attacks fulfilling criteria B-E |
| B. Developing only during sleep, and causing wakening |
| C. Occurring on>10 days per month for>3 months |
| D. Lasting ≥15minutes and for up to 4hours after waking |
| E. No cranial autonomic symptoms or restlessness |
| F. Not better accounted for by another ICHD-3 diagnosis |
| Probable hypnic headache: |
| A. Recurrent headache attacks fulfilling criterion B and 2 only of criteria C-E |
| B. Developing only during sleep, and causing wakening |
| C. Occurring on>10 days per month for>3 months |
| D. Lasting ≥ 15minutes and for up to 4hours after waking |
| E. No cranial autonomic symptoms or restlessness |
| F. Not fulfilling ICHD-3 criteria for any other headache disorder |
| G. Not better accounted for by another ICHD-3 diagnosis |
We report a series of 10 patients diagnosed with HH in a specialised headache clinic at a tertiary hospital between January 2008 and May 2013.
Our main aim is to assess the suitability of the diagnostic criteria listed by the ICHD-2 and the updated ICHD-3 in the context of our patient series.
Patients and methodsWe retrospectively reviewed the database from a specialised headache clinic at a tertiary hospital for the period between January 2008 and May 2013. We performed a descriptive analysis of the patients diagnosed with HH in that period. Diagnosis of HH was first based on the clinical characteristics of this entity, and doctors later confirmed that patients met HH criteria.
Our team conducted personal and telephone interviews by means of a standardised questionnaire including patients’ demographic characteristics (sex, age) and main characteristics of the headache (date of headache onset, pain characteristics, and location). We also documented the time elapsed between sleep onset and the episode, if episodes awakened the patient, headache duration, and headache frequency in days per month. Patients were also asked about any accompanying autonomic symptoms, phonophobia or photophobia, and associated nausea. Pain intensity was quantified on a scale of 0 to 10 using an analogue visual scale (AVS). We also checked for co-presence of insomnia and whether patients received insomnia treatment. All our patients were prescribed indometacin as preventive treatment. We considered positive response to treatment with indometacin as a decrease in episode frequency of 50% or more in one month.
ResultsTen patients out of a total of 720 (1.39%) attending the headache clinic were diagnosed with HH during the study period. All patients underwent neurological examination, and a neuroimaging study (computed tomography or magnetic resonance). Examinations and imaging studies yielded no pathological findings in all cases.
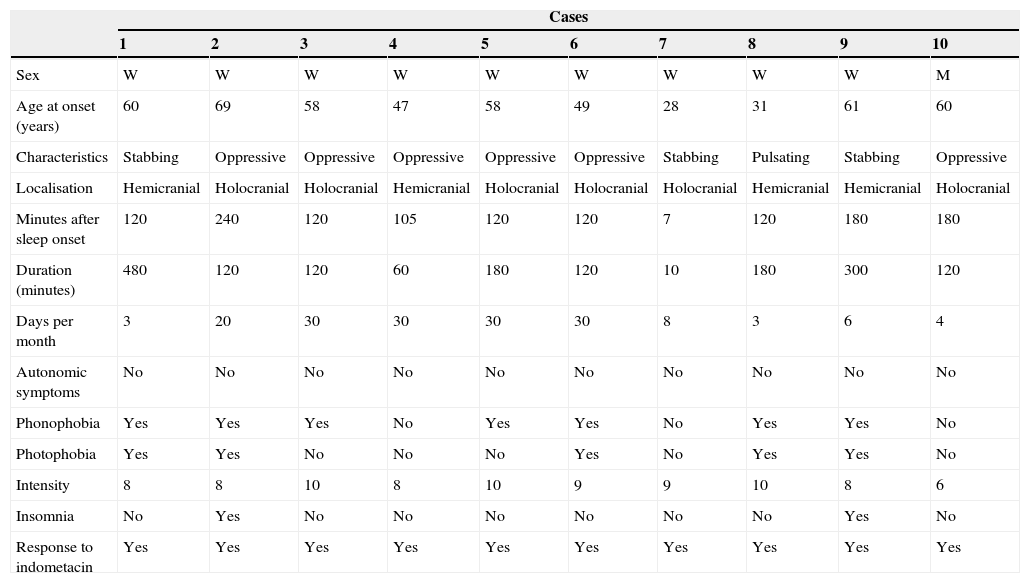
The patients’ main characteristics are listed in Table 3.
Characteristics of our patients with hypnic headache
| Cases | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
| Sex | W | W | W | W | W | W | W | W | W | M |
| Age at onset (years) | 60 | 69 | 58 | 47 | 58 | 49 | 28 | 31 | 61 | 60 |
| Characteristics | Stabbing | Oppressive | Oppressive | Oppressive | Oppressive | Oppressive | Stabbing | Pulsating | Stabbing | Oppressive |
| Localisation | Hemicranial | Holocranial | Holocranial | Hemicranial | Holocranial | Holocranial | Holocranial | Hemicranial | Hemicranial | Holocranial |
| Minutes after sleep onset | 120 | 240 | 120 | 105 | 120 | 120 | 7 | 120 | 180 | 180 |
| Duration (minutes) | 480 | 120 | 120 | 60 | 180 | 120 | 10 | 180 | 300 | 120 |
| Days per month | 3 | 20 | 30 | 30 | 30 | 30 | 8 | 3 | 6 | 4 |
| Autonomic symptoms | No | No | No | No | No | No | No | No | No | No |
| Phonophobia | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes | No |
| Photophobia | Yes | Yes | No | No | No | Yes | No | Yes | Yes | No |
| Intensity | 8 | 8 | 10 | 8 | 10 | 9 | 9 | 10 | 8 | 6 |
| Insomnia | No | Yes | No | No | No | No | No | No | Yes | No |
| Response to indometacin | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
Nine of the 10 patients with a final diagnosis of HH were women. Mean age of onset was 52.1±13.42 years (range, 28-69 years).
Regarding pain characteristics, 6 patients (60%) described the pain as dull and oppressive, 3 patients as stabbing (30%), and one patient as pulsating (10%). Headache location was holocranial in 6 cases (60%) and hemicranial in 4 cases (40%).
Eight of the 10 patients reported that headache manifested exclusively during nocturnal sleep, while 2 patients also reported similar headache episodes during daytime naps. In all cases, patients were awakened by headaches.
The mean number of days with headache per month was 16.4 (range, 3-30). Five of our patients (50%) reported a frequency of HH episodes lower than 15 days per month and 3 patients (30%) reported a frequency inferior to 10 days per month.
Mean duration of headache episodes was 169minutes (range, 10-480minutes). None of our patients presented autonomic symptoms associated with headache episodes. However, 7 patients (70%) presented associated phonophobia and 5 (50%) reported photophobia during episodes. Five patients from our series (50%) presented associated phonophobia and photophobia simultaneously. No accompanying nausea was reported by any of the patients.
In all 10 cases, headaches were not attributed to any other disorders, and arterial hypertension and obstructive sleep apnoea syndrome were ruled out as possible causes.
All our patients scored pain intensity as 8 points or higher on the AVS.
All patients began treatment with indometacin at 100mg per day divided into 2 doses, and they reported a decrease in episode frequency during the first treatment cycle.
Regarding associated insomnia, 2 patients (20%) reported difficulty falling asleep, and both were prescribed benzodiazepines as occasional treatment.
DiscussionThere is a complex and bidirectional relationship between headache and sleep, although the exact pathophysiology remains unknown.
The associations between headache and sleep can be classified as follows:
- -
Headache as a result of a sleep disorder (obstructive apnoea syndrome, insomnia, etc.).
- -
Headache as a cause of a sleep disorder (chronic tension-type headache and chronic migraine).
- -
Intrinsic relationship between headache and sleep. HH pertains to this latter group as a headache manifesting exclusively during sleep, whereas migraine, cluster headache, and hemicrania continua may manifest during sleep or wakefulness.8
Many published studies have suggested different hypotheses to explain HH pathophysiology.
In most published series of patients who have undergone polysomnography (PSG), onset of episodes occurred most frequently during REM sleep.9–12
This information may lead us to believe that the structures involved in pain processing are activated during REM sleep. In REM sleep, the dorsal raphe nucleus and locus coeruleus show no activity. These nuclei, together with periaqueductal grey, are essential parts of the antinociceptive system. Dysfunction of these areas of the brainstem may therefore explain the pathophysiology underlying HH. However, patients with migraine or autonomic trigeminal cephalalgias who underwent PSG also presented headache with onset during REM sleep, so this finding is not specific to HH.
Some authors also hypothesise that HH may be a chronobiological disorder. The main structure involved in the maintenance of the endogenous circadian rhythms is the suprachiasmatic nucleus (SCN), which in turn is connected to the periaqueductal grey by means of afferent and efferent fibres. The function of the hypothalamic-pineal axis, and of the SCN in particular, is diminished in elderly individuals, and melatonin secretion also decreases.13
Holle et al.14 used voxel-based morphometry in nuclear magnetic resonance imaging studies to detect loss of grey-matter volume in the posterior hypothalamus of HH patients compared to age- and sex-matched healthy controls.
As mentioned previously, the posterior hypothalamus, especially the SCN, is involved in sleep regulation and pain control. Therefore, these findings can confirm hypothalamic dysfunction as the main headache mechanism in patients diagnosed with HH.
Utility of diagnostic criteriaSeveral recently published HH patient series have questioned the utility of the ICHD diagnostic criteria for this entity.2,3,15
In our series, only 3 out of our 10 patients with a final diagnosis of HH (30%) meet the ICHD-2 criteria, whereas 5 patients (50%) meet ICHD-3 criteria. Furthermore, the new classification includes the concept ‘probable hypnic headache’, which is likely to apply to 2 more patients in our series. Three patients do not meet criteria for either HH or probable HH because their episode frequency is less than 10 per month; also, one of these patients has an episode duration of less than 15minutes, vs more than 4hours in the other 2 patients.
We were surprised to find that 9 of the 10 patients in our series were women (90%). HH is a headache with female predominance; the female-to-male ratio is 1.6:1 according to the published series.3,14–16
We will now review the utility of the ICHD-2 diagnostic criteria.
Regarding headache characteristics (criterion A), ICHD-2 defines HH as a dull headache. However, 4 patients in our series (40%) described pain as stabbing or pulsating. These findings are similar to those reported in other published series, in which headache is described as stabbing or pulsating in up to 30% of all cases.17
ICHD-2 criterion B establishes that headaches must develop only during sleep, and necessarily awaken the patient. This criterion, met by 100% of our patients, is the distinguishing feature of this entity.
We will now review the sections included in criterion C. Criterion C establishes a headache frequency of more than 15 days per month. Headache frequency was below this threshold in 5 of our patients (50%). Previously published series report more variability in this criterion; percentages of patients whose headache frequency was below 15 days per month range from 5% to 50%. Regarding the proposed minimum duration (15minutes), only one case in our series (10%) reported a duration of less than 15minutes (10minutes). We therefore believe that the minimum duration of 15minutes is appropriate for distinguishing this syndrome from other paroxysmal disorders of shorter duration. Regarding age of onset, 6 patients meet the criterion, since they were aged 50 or older when headaches started, leaving 4 patients who were younger than 50 years at time of diagnosis. Age of onset younger than 50 years does not rule out the diagnosis of HH, although, as previously mentioned, this entity manifests in elderly individuals with decreased SCN activity that affects the circadian pacemaker. Another factor to consider is that in HH, the time elapsed between pain onset and diagnosis may stretch to years, which can also explain why patients tend to be older.
Criterion D establishes that no accompanying autonomic symptoms should be present and patients must present only one of the following: nausea, photophobia, or phonophobia. In some published series, up to 15% of the patients presented autonomic symptoms together with headache.2
None of our patients reported nausea with the headache. Five of our patients (50%) reported associated phonophobia and photophobia. Published series report percentages greater than 25%; we believe that criterion D is very strict, and we suggest that phonophobia and photophobia may present with these headaches.
Lastly, criterion E establishes that headache is not attributed to another disorder. In case of night-time headache, we must check for arterial hypertension or obstructive sleep apnoea syndrome since these entities may cause headache. Our patients’ medical records indicated no history of arterial hypertension or of obstructive sleep apnoea syndrome.
The principal modifications to the definition of HH in the ICHD-3 have amended the criteria leading to the most controversy for our series: headache is no longer described as necessarily dull pain, so pulsating or stabbing headaches are now recognised in these patients. Episodes may also be less frequent than 15 days per month. The limit currently stands at 10 days per month for 3 months and headache episodes may last up to 4hours. However, as our series demonstrates, these are probably the most variable parameters. Age is no longer listed among the diagnostic criteria. Age younger than 50 years is no longer a reason for ruling out diagnosis of HH, although, as we mentioned before, HH is more frequent among elderly patients due to its underlying pathophysiology. According to the new criteria, nausea, phonophobia, and photophobia may be associated with the syndrome, and this is a better reflection of our patients’ characteristics.
Regarding HH treatment, there are no randomised clinical trials since the syndrome is quite rare. Many symptomatic treatment options have been tried, including anti-inflammatory drugs and caffeine; this latter is more effective for treating pain episodes. In one of the latest series published, triptanes, which were never considered effective for these headaches, proved their efficacy in the 4 patients who were treated with the drug. Other alternatives, such as high-flow oxygen or opioid analgesics, have not been effective in the cases described.
There are also several options for preventive treatment, although no controlled clinical trials have assessed the efficacy of the different drugs.
Lithium has been used prophylactically since this entity was first described, but its results are controversial. One of the hypotheses for how the drug might be effective is that lithium indirectly increases melatonin secretion. However, the difficulty of managing this drug, its adverse effects, and the launch of new treatment options have relegated lithium to a secondary position at present.
Indometacin, which is effective against other primary headaches including paroxysmal hemicrania and hemicrania continua, is also reported to be effective for preventing HH. Improvement is particularly frequent in patients experiencing unilateral headache.18
Indometacin dosed at 100mg a day was the drug of choice in our series, and it decreased episode frequency by≥50%. Although this drug is effective, it is poorly tolerated by the stomach and can cause headache during daytime. Because of this and other adverse effects, this treatment is administered in cycles and it has to be withdrawn in many patients despite providing headache relief.
Some series and isolated anecdotal cases have used other drugs for HH prophylaxis, such as flunarizine, verapamil, amitriptyline, and topiramate. Data on the efficacy of these treatments is variable.19
This study presents some limitations. Our patient series is small, but as mentioned before, HH is a rare primary headache. We performed a prospective review of our database, and therefore data are merely descriptive. Data from some patients were collected by telephone interview since it was not possible for them to come to check-ups. This strategy allowed us to include all patients diagnosed with HH in our clinic.
In conclusion, we present a series of 10 patients with HH and determine whether their clinical characteristics correspond with the ICHD-2 and ICHD-3 criteria.
The ICHD-2 criteria are too strict to reflect this entity. The most controversial criteria, according to features of our patient series, are age of onset older than 50 years, the pain location and characteristics, and permitting only 2 of the following 3 associated symptoms: nausea, phonophobia, or photophobia.
Changes to HH criteria in the ICHD-3 are related to the requirements listed above, and we therefore believe that these changes were necessary. These new criteria are more consistent with our series and with other reported series.
Regarding treatment, we feel that randomised clinical trials should be performed to establish standard symptomatic and preventive treatment regimens. Indometacin can provide effective treatment for these patients.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Escudero Martínez I, González-Oria C, Bernal Sánchez-Arjona M, Jiménez Hernández MD. Descripción de una serie de 10 pacientes con cefalea hípnica: discusión de criterios diagnósticos. Neurología. 2015;30:195–200.