In-hospital consultation (IHC) is a service that some medical specialties provide to others with the aim of resolving complications in patients admitted to different hospital units. The aim of this study is to perform a descriptive analysis and longitudinal study of IHCs received in our department during the last 5 years.
MethodA retrospective study was conducted on the IHCs made within the period 2005–2009. The data analysed were as follows: department of origin of the IHC, reason for consulting, date, priority of care, definitive diagnosis, need for follow-up, need for transfer, and the demographic data of the patients.
ResultsThere were a total of 1458 IHCs in the period studied. The mean age of the patients was 58.2±19.10 years, and 837 (57.6%) were males. The number of IHCs per year was: 2005: 263; 2006: 226; 2007: 239; 2007: 239; 2008: 329 and 2009: 401. The majority (86.8%) had normal priority, 8.5% high priority, and 4.7% were urgent. The Emergency Department (12%), Cardiology (10.9%), General Medicine (9.8%) and Psychiatry (8.9%) were the services with the highest demand. The most frequent reasons for consulting were loss of consciousness and epileptic seizures (24.6%), cerebral vascular disease (21.1%), and confusional states and cognitive impairment (13.4%). Over one-third (36.8%) were resolved in the first consultation, and the remainder (63.8%) required follow up. Of all the cases assessed, 8.4% required transfer to Neurology.
ConclusionsIHC is a complex activity that may not resolve all questions in a single visit. It involves a health care burden which is increasing annually. The increasing diagnostic complexity of the neurology, as well as the increasingly more specific treatments are the factors that lead to this higher demand.
Las interconsultas hospitalarias (ICh) constituyen un servicio que se ofrece de unas especialidades médicas a otras con la función de ayudar a resolver las complicaciones de los pacientes ingresados en las distintas unidades del hospital. El objetivo de este trabajo es analizar descriptivamente y con carácter temporal las ICh recibidas en nuestro servicio durante el último quinquenio.
MétodoEstudio retrospectivo de las ICh realizadas. Periodo: 2005-2009. Los datos analizados son: servicio de origen de la interconsulta, motivo de consulta, fecha, prioridad en la atención, diagnóstico definitivo, necesidad de seguimiento, necesidad de traslado y datos demográficos de los pacientes.
Resultadosn=1458 ICh. Edad media 58,2±19,10. Varones: 837 (57,6%). Por año el número de ICh fue: 2005: 263; 2006: 226; 2007: 239; 2007: 239, 2008: 329 y 2009: 401. El 86,8% tenían prioridad normal, 8,5% preferente y 4,7% urgentes. Urgencias (12%), Cardiología (10,9%), Medicina Interna (9,8%) y Psiquiatría (8,9%) fueron los servicios con mayor demanda. Los motivos de consulta más frecuente fueron: pérdidas de conciencia y crisis epilépticas (24,6%), patología vascular cerebral (21,1%) y cuadros confusionales y deterioro cognitivo (13,4%). El 36,8% se resolvieron en la primera consulta y el resto (63,8%) precisaron de seguimiento. Precisaron traslado a Neurología el 8,4% de los casos valorados.
ConclusionesLa ICh es una actividad compleja que no se resuelve en una única visita. Provoca una carga asistencial que crece cada año. La creciente complejidad diagnóstica de la neurología y los tratamientos cada vez más específicos son los factores que condicionan este aumento de la demanda.
An in-hospital consultation (IHC) is an activity in which different medical specialties work together to determine the diagnostic and therapeutic approaches for patients admitted to different hospital units.1,2 Typical reasons for requesting an IHC may include acute neurological problems, an exacerbation of a pre-existing neurological condition, or needing to resume a patient's previous drug treatment.
Characteristics of neurological care offered through IHC are not homogeneous in all hospitals. This type of care is often overlooked, despite being a potentially complex activity that consumes a great deal of the consulting doctor's time and a considerable amount of hospital resources.3 Although IHCs provide valuable information about the workings of both the department called for a consult and the hospital itself, there are very few published studies on this topic, whether for neurology4–7 or for other medical specialties.3,7–11 No other study published to date addresses how IHCs have evolved over prolonged periods of time.
The purpose of our article is to provide a descriptive and retrospective analysis of IHC requests received by our department in the last 5 years.
Materials and methodsRetrospective study of IHCs was carried out during 5 full years between 1 January 2005 and 31 December 2009. The study was performed in the neurology department at Hospital Universitario Infanta Cristina, Badajoz, Spain. This tertiary hospital contains 890 beds (24 in the neurology department) and provides service to an area with 270317 inhabitants. As of when this study was prepared, there was no available continuous care form for the neurology department.
IHCs are requested by filling out one of the hospital's standard forms with the following information: name, medical record number, date of birth, sex, bed upon admission, specialty requesting the consultation, consulting specialty, priority, date requested, date provided, reason for the request, report by the consulting specialty, and doctor answering the request. We analysed the following data: specialty requesting consultation, reason for the request, date, priority, definitive diagnosis, need for follow-up, need for transfer, and patients’ demographic data.
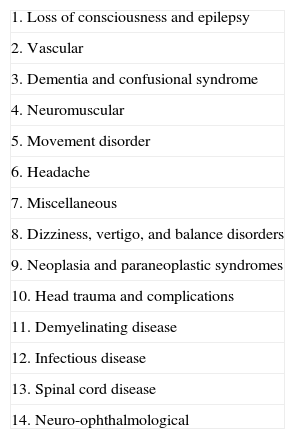
For purposes of this analysis, reasons for consultation have been categorised in different diagnostic groups according to the neurologist's medical opinion (Table 1). In order to facilitate analysis over time, the requesting specialties have been grouped into 4 major areas: outpatient care, internal medicine and infectious diseases, intensive care/emergency department, and the surgical area. The IHC index was calculated using the formula ‘number of consultations per year/number of hospital beds’. We also calculated an index that shows the potential impact of this activity on daily practice using the formula ‘number of consultations per year/number of working days per year in the study’.
Diagnostic group according to the report issued by the neurologist.
| 1. Loss of consciousness and epilepsy |
| 2. Vascular |
| 3. Dementia and confusional syndrome |
| 4. Neuromuscular |
| 5. Movement disorder |
| 6. Headache |
| 7. Miscellaneous |
| 8. Dizziness, vertigo, and balance disorders |
| 9. Neoplasia and paraneoplastic syndromes |
| 10. Head trauma and complications |
| 11. Demyelinating disease |
| 12. Infectious disease |
| 13. Spinal cord disease |
| 14. Neuro-ophthalmological |
We used an adapted data collection form and recorded information in a database which allowed us to process data using SPSS version 14.0. Qualitative results are expressed as percentages and quantitative results are expressed as mean (SD). Using the raw data from a longitudinal study of IHCs over a 5-year period, we completed a projection for the following 5 years using a linear regression estimate. We used the Mantel-Haenszel chi-square test to evaluate increases or decreases for the following variables: requests by area, priority, need for follow-up, and need for transfer to the neurology department during the study period.
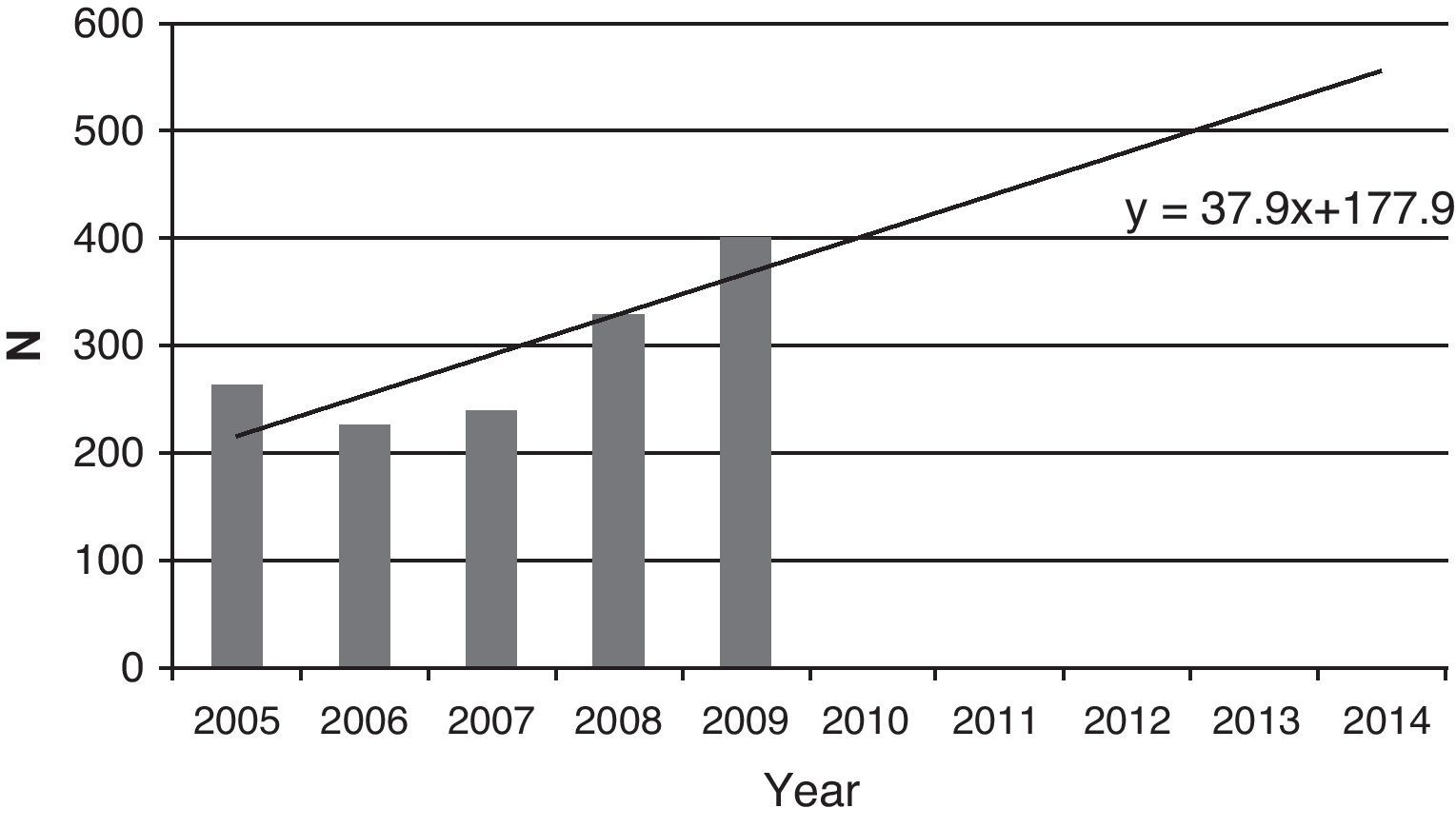
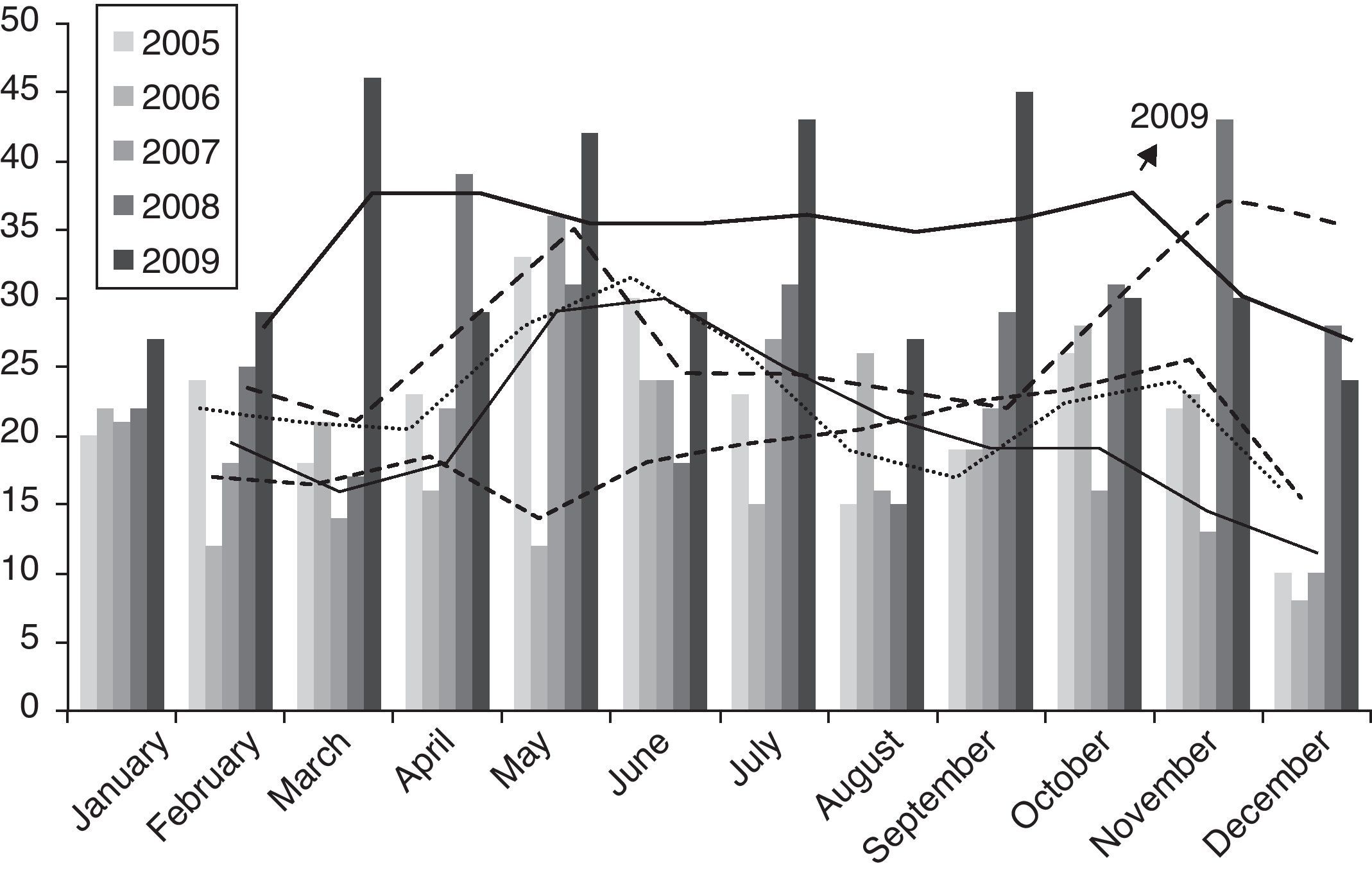
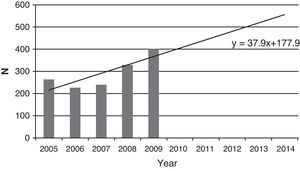
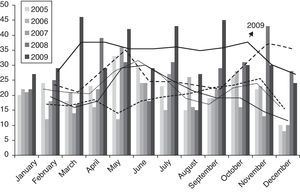
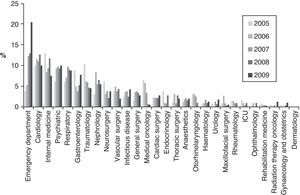
ResultsDuring the study period, doctors requested 1458 IHCs corresponding to 1458 patients (double or triple consultations for the same process were counted only once). Mean age of patients was 58.2 (19.10) years. Males accounted for 57.6% of the total (n=837). The number of IHCs per year was as follows: 263 in 2005; 226 in 2006; 239 in 2007; 329 in 2008; and 401 in 2009 (Fig. 1). The IHC index ranged from 0.29 in the first year of the study to 0.45 in 2009. In the first 4 years, we observed seasonal variability in the number of requests for consultations, which decreased during holiday periods between June and September and again in December. However, this variability was not present throughout 2009, which saw a more regular flow of activity throughout the year (Fig. 2).
Of the total IHCs performed, 86.8% were rated normal priority, 8.5% high priority, and 4.7% as urgent. In 36.8% of the cases, the questions were resolved with the first consultation; the other 63.8% required follow-up visits, and 8.4% of the cases were referred to the neurology department. The outpatient area requested the most IHCs (694, 47.9%), followed by the surgical area (191, 13.2%), internal medicine and infectious diseases (380, 26.2%), and the emergency department/intensive care unit (185, 12.8%). During the study period, we observed a significant increase in requests by the emergency/intensive care area and a decrease in requests by the surgical area (XMH2=7.040; P=.008). Demographic variables (age and sex) remained stable over the 5-year study period. No changes were observed in the priority levels assigned to consultation requests. We observed an increase in the percentage of follow-up studies after an initial consultation request for a patient, and the differences were significant (XMH2=71.442; P<.0001). In addition, the number of patients needing referrals to the neurology department increased progressively (XMH2=12.206; P<.0001). Table 2 presents a summary of these data.
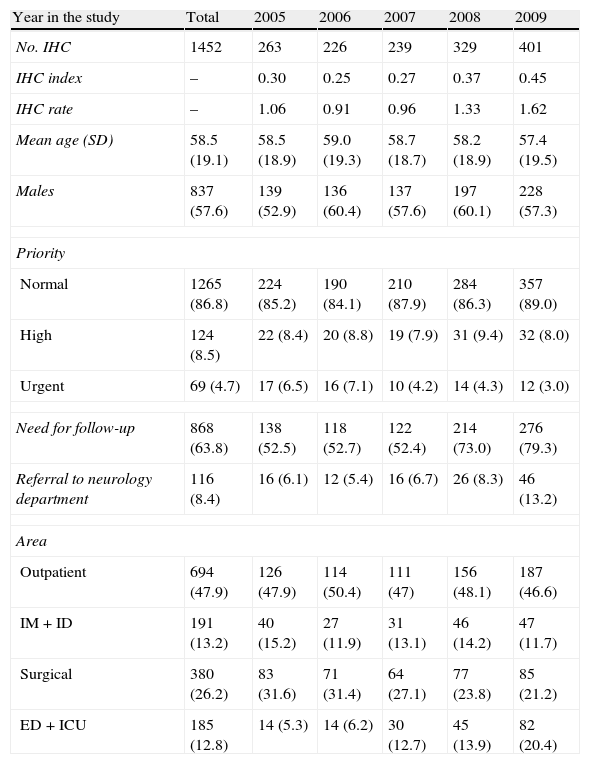
Changes in consultations over time.
| Year in the study | Total | 2005 | 2006 | 2007 | 2008 | 2009 |
| No. IHC | 1452 | 263 | 226 | 239 | 329 | 401 |
| IHC index | – | 0.30 | 0.25 | 0.27 | 0.37 | 0.45 |
| IHC rate | – | 1.06 | 0.91 | 0.96 | 1.33 | 1.62 |
| Mean age (SD) | 58.5 (19.1) | 58.5 (18.9) | 59.0 (19.3) | 58.7 (18.7) | 58.2 (18.9) | 57.4 (19.5) |
| Males | 837 (57.6) | 139 (52.9) | 136 (60.4) | 137 (57.6) | 197 (60.1) | 228 (57.3) |
| Priority | ||||||
| Normal | 1265 (86.8) | 224 (85.2) | 190 (84.1) | 210 (87.9) | 284 (86.3) | 357 (89.0) |
| High | 124 (8.5) | 22 (8.4) | 20 (8.8) | 19 (7.9) | 31 (9.4) | 32 (8.0) |
| Urgent | 69 (4.7) | 17 (6.5) | 16 (7.1) | 10 (4.2) | 14 (4.3) | 12 (3.0) |
| Need for follow-up | 868 (63.8) | 138 (52.5) | 118 (52.7) | 122 (52.4) | 214 (73.0) | 276 (79.3) |
| Referral to neurology department | 116 (8.4) | 16 (6.1) | 12 (5.4) | 16 (6.7) | 26 (8.3) | 46 (13.2) |
| Area | ||||||
| Outpatient | 694 (47.9) | 126 (47.9) | 114 (50.4) | 111 (47) | 156 (48.1) | 187 (46.6) |
| IM+ID | 191 (13.2) | 40 (15.2) | 27 (11.9) | 31 (13.1) | 46 (14.2) | 47 (11.7) |
| Surgical | 380 (26.2) | 83 (31.6) | 71 (31.4) | 64 (27.1) | 77 (23.8) | 85 (21.2) |
| ED+ICU | 185 (12.8) | 14 (5.3) | 14 (6.2) | 30 (12.7) | 45 (13.9) | 82 (20.4) |
SD: standard deviation; IHC: in-hospital consultation; IHC index: number of consultations per year/number of hospital beds; IM: internal medicine; No.: number; IHC rate: number of consultations per year/working days per year; ICU: intensive care unit; ID: infectious disease; ED: emergency department.
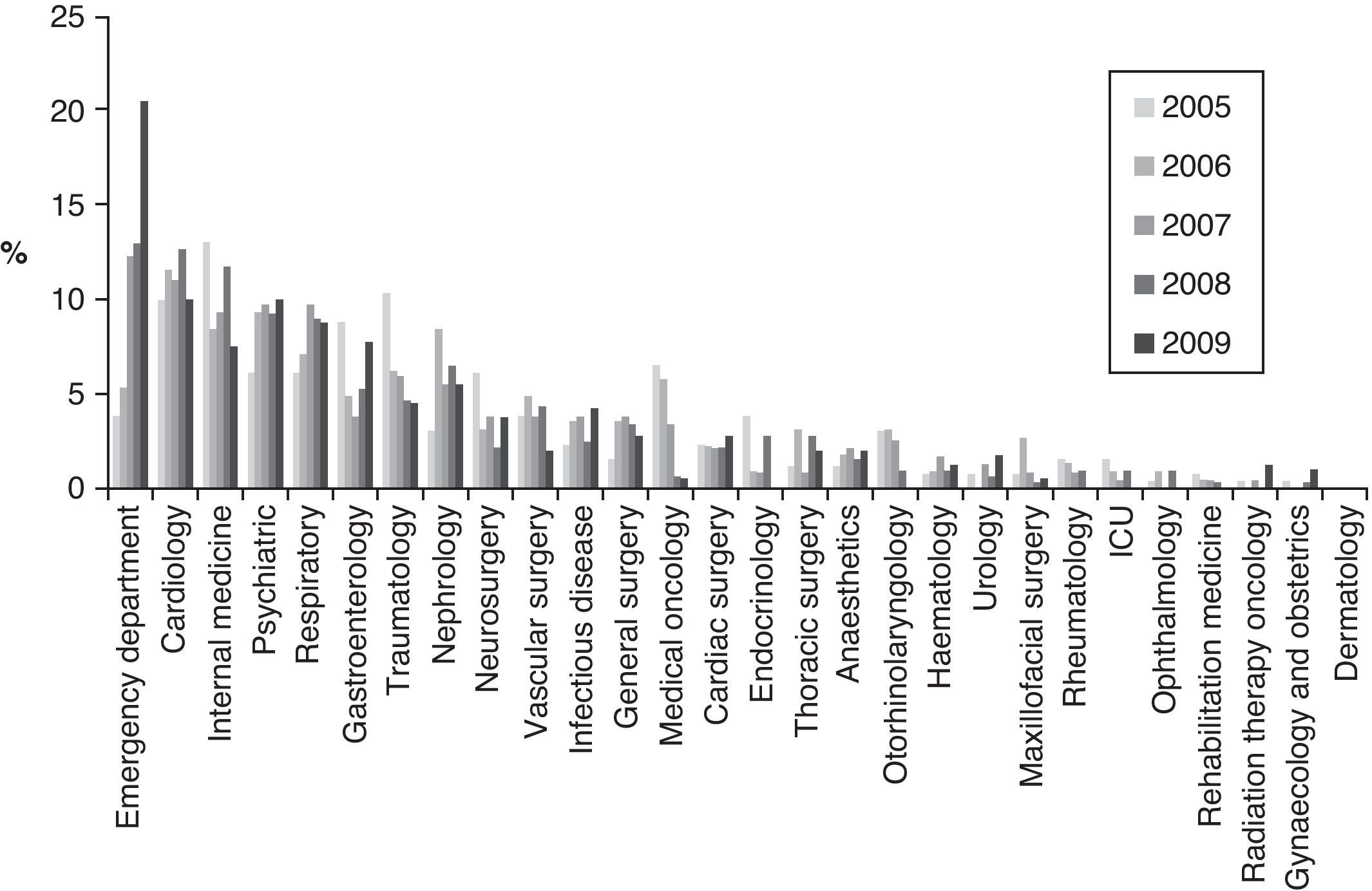
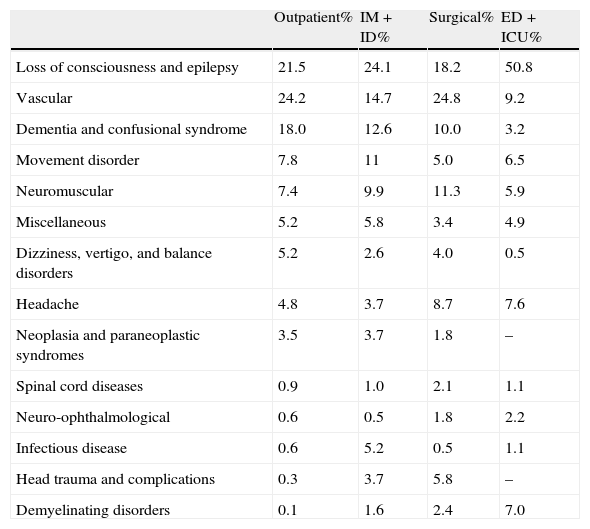
Overall, the specialties with the most need for neurological care were the emergency department (12.0%), cardiology (10.9%), internal medicine (9.8%), and psychiatry. These percentages remained stable over the years except for the marked increase in IHCs requested by the emergency department (Fig. 3). The most frequent motives for requesting consultation were as follows: loss of consciousness/epileptic attack (24.6%), cerebrovascular disease (21.1%) and confusional syndrome/cognitive decline (13.4%). Percentages remained stable over the 5-year study period. Table 3 displays motives for requesting consultation grouped by area.
Disease groups requiring the most consultations per specialty area.
| Outpatient% | IM+ID% | Surgical% | ED+ICU% | |
| Loss of consciousness and epilepsy | 21.5 | 24.1 | 18.2 | 50.8 |
| Vascular | 24.2 | 14.7 | 24.8 | 9.2 |
| Dementia and confusional syndrome | 18.0 | 12.6 | 10.0 | 3.2 |
| Movement disorder | 7.8 | 11 | 5.0 | 6.5 |
| Neuromuscular | 7.4 | 9.9 | 11.3 | 5.9 |
| Miscellaneous | 5.2 | 5.8 | 3.4 | 4.9 |
| Dizziness, vertigo, and balance disorders | 5.2 | 2.6 | 4.0 | 0.5 |
| Headache | 4.8 | 3.7 | 8.7 | 7.6 |
| Neoplasia and paraneoplastic syndromes | 3.5 | 3.7 | 1.8 | – |
| Spinal cord diseases | 0.9 | 1.0 | 2.1 | 1.1 |
| Neuro-ophthalmological | 0.6 | 0.5 | 1.8 | 2.2 |
| Infectious disease | 0.6 | 5.2 | 0.5 | 1.1 |
| Head trauma and complications | 0.3 | 3.7 | 5.8 | – |
| Demyelinating disorders | 0.1 | 1.6 | 2.4 | 7.0 |
IHCs are unscheduled, discontinuous tasks that are not accounted for in hospital planning activities. No special emphasis is placed on this type of work, which can often be problematic.3 The medical literature from Spain includes only 4 published studies addressing IHCs with a neurology department.4–7 This highlights the low level of interest in an activity which, in any case, takes place on a daily basis in clinical practice, and also consumes resources. In order for clinical units to function properly, there must be a record of each type of care task so that available human and material resources may be managed appropriately according to the characteristics of the department and the hospital itself.1,2 Efficient, quality care provided by means of IHCs will improve management of neurological patients who are admitted for different reasons. It will also limit unnecessary referrals to other departments and increase trust in the service being requested.12
Our study follows changes in IHC use during a 5-year period. This type of longitudinal analysis is not found in other prior articles. We recorded a clear linear increase in the demand for IHCs over the 5-year period. The IHC rate increased steadily and the workload these tasks represented rose by more than 50% between the first year of the study and the last year. Furthermore, there were no seasonal variations in the last year; the number of consultations requested monthly remained stable. Projections for this activity point to an increasing care burden that will require the dedication of additional resources. The largest part of the increase in workload may be due to the growing diagnostic complexity of the specialty of neurology and the increasingly specific treatments it requires, in addition to more rigorous standards for patient care. Other factors support this argument, such as the increasing difficulty of resolving an IHC in a single session. Doctors frequently need to run complementary tests and follow-up studies, and there is also a progressive rise in patient referrals to the neurology department for further study or for specific treatments. As a result, IHC has become an additional channel by which patients reach a department, and this should be considered in the hospital planning process. Proper organisation of IHCs leads to marked improvement of results. The request form should be as simple as possible, and ideally it would be planned with a reliable and motivated expert consultant.13
Our demographic data, the most common motives for requesting a consultation, and the specialties with the most requests for neurological care are similar to those in other studies carried out in Spain.4–7 We observed that the area with the sharpest increase in IHC referrals was the emergency department. This is one of the reasons explaining why urgent-priority IHCs and referrals to the neurology department were so numerous in our study compared to other studies. It is true that hospital emergency departments have not traditionally been considered in analyses of IHCs, and the fact that we opted to include them may explain differences between our study and those published by other Spanish hospitals. However, we believe that they should be included; in our care system, the emergency department acts as a powerful consultant on neurological diseases, which is not the case for diseases that clearly require hospitalisation. The ED may freely handle cases without first consulting with departments that lack on-call staff. The emergency department requests formal IHCs, using the form used by the rest of the hospital, when faced with diseases with difficult therapeutic or treatment approaches. The rising demand for IHCs by the emergency department and the numerous urgent IHCs and patient referrals may be explained by the lack of an on-call neurologist. Implementation of continuous care may resolve the situation.14,15 However, if we were to exclude the emergency department as other studies did, we would still agree that most requests for IHCs come from the cardiology, internal medicine, and psychiatric departments. The high percentage of IHCs requested by the psychiatric department could be explained by its close cooperation with the neurology department, as other studies have also indicated.7 In the analysis broken down by area, we find that requests from the surgical area have decreased in recent years. An explanation that may explain this change is that certain units, such as traumatology and general surgery, have been offered the support of a consulting internist. This is a helpful resource for surgical departments whenever patient volume and characteristics so permit, and adding an internist to the team has been shown to be fruitful and cost-effective.16,17
Our study's main limitations are its retrospective approach and the datasheets used as the source of information. These datasheets result in an inevitable loss of data and reduce the number of study variables.
In conclusion, IHC is a complex activity that is usually not limited to a single visit and consumes neurology department resources. This should be taken into consideration when planning activities. IHCs contribute to a care burden that grows year by year in proportion to the increases in diagnostic and therapeutic complexity in the specialty of neurology. IHC is a channel for direct cooperation with other medical specialties. It contributes to the department's image within the hospital and should therefore be handled with dedication and care.
Conflicts of interestThe authors have no conflicts of interest to declare.
Presented at the 62nd Annual Meeting of the Spanish Society of Neurology, 16–20 November 2010, Barcelona, Spain.
Please cite this article as: Ramírez-Moreno JM, et al. Evolución temporal de las interconsultas hospitalarias dirigidas a Neurología en un hospital terciario. Una actividad asistencial en crecimiento. Neurología. 2013;28:9–14.