During acute stroke, 30% of all patients present dysphagia and 50% of that subgroup will experience bronchoaspiration. Our aim was to compare mortality and bronchoaspiration rates associated with the water test compared to those associated with a 2 volume/3 texture test controlled with pulse oximetry (2v/3t-P test) in our stroke unit.
Patients and methodsOver a 5-year period, we performed a prospective analysis of all consecutive acute ischaemic stroke patients hospitalised in the stroke unit. Dysphagia was evaluated using the water test between 2008 and 2010 (group 0 or G0), and the 2v/3t-P test (group 1 or G1) between 2011 and 2012. We analysed demographic data, vascular risk factors, neurological deficit on the NIHSS, aetiological subtype according to TOAST criteria, clinical subtype according to the Oxfordshire classification, prevalence of dysphagia, percentage of patients with bronchoaspiration, and mortality.
ResultsWe examined 418 patients with acute stroke (G0=275, G1=143). There were significant differences between the 2 groups regarding the percentage of patients with TACI (17% in G0 vs 29% in G1, P=.005) and median NIHSS score (4 points in G0 vs 7 points in G1, P=.003). Since adopting the new swallowing test, we detected a non-significant increase in the percentage of dysphagia (22% in G0 vs 25% in G1, P=.4), lower mortality (1.7% in G0 vs 0.7% in G1, P=.3) and a significant decrease in the bronchoaspiration rate (6.2% in G0 vs 2.1% in G1, P=.05).
ConclusionsCompared to the water test used for dysphagia screening, the new 2v/3t-P test lowered bronchoaspiration rates in acute stroke patients.
En la fase aguda del ictus el 30% de los pacientes presentan disfagia, y de ellos, el 50% experimentarán broncoaspiración. Nuestro objetivo fue evaluar los resultados de mortalidad y broncoaspiración del test del agua comparado con el test 2 volúmenes/3 texturas controlado con pulsioximetría (2v/3t-P) en una unidad de ictus.
Pacientes y métodosDurante 5 años se analizaron de forma prospectiva y consecutiva todos los pacientes con infarto cerebral en la Unidad de Ictus. Del año 2008 al 2010 se utilizó el test del agua (grupo 0 o G0), y del 2011 al 2012, el test 2v/3t-P (grupo 1 o G1). Se recogieron las siguientes variables: demográficas, factores de riesgo vascular, gravedad neurológica con la escala NIHSS, subtipo etiológico según criterios TOAST, subtipo clínico según la clasificación Oxfordshire, prevalencia de disfagia, broncoaspiración y exitus.
ResultadosSe analizaron 418 pacientes con infarto cerebral agudo (G0=275, G1=143). Se detectaron diferencias significativas entre ambos grupos en el porcentaje de pacientes con TACI (17% en G0 vs. 29% en G1, p=0,005) y en la mediana de NIHSS (4 puntos en G0 vs. 7 puntos en G1, p=0,003). Con el test 2v/3t-P se detectó un aumento no significativo en el porcentaje de disfagia (22% en G0 vs. 25% en G1, p=0,4), una menor tasa de mortalidad (1,7% en G0 vs. 0,7% en G1, p=0,3) y una reducción significativa de broncoaspiración (6,2% en G0 vs. 2,1% en G1, p=0,05).
ConclusionesEl nuevo test 2v/3t-P, comparado con el test del agua, mejoró significativamente los resultados de broncoaspiración en los pacientes con infarto cerebral agudo.
Dysphagia, a frequent complication of stroke, is associated with increased risk of bronchoaspiration. Between 19% and 81% of stroke patients have dysphagia,1–3 and half of them experience bronchoaspiration within the first week of stroke onset.4,5 Dysphagia is an important predictor of poor outcome: it leads to poor functional status at discharge2 and increases the number of respiratory complications,6 the length of hospital stays, hospitalisation rates, and mortality.7 Furthermore, presence of dysphagia entails a three-fold increase in the risk of pneumonia,2 which in turn leads to a three-fold increase in the risk of mortality at 30 days.1
Scientific evidence suggests that early diagnosis and treatment of dysphagia in stroke patients reduces not only respiratory complications but also the length of hospital stay and health-related costs.8
The 3-oz water swallow test9 is one of the most widely used tests for dysphagia screening. However, this test uses a large volume of water (which has a low viscosity) and it regards coughing as the sole indicator of aspiration, although this reflex is absent in nearly 40% of all patients with cerebrovascular diseases.10 Silent aspiration may be detected with pulse oximetry: a drop of more than 2% in oxygen saturation compared to baseline values is regarded as a sign of bronchoaspiration.11,12
At present, videofluoroscopy and fibreoptic endoscopy are the main validated techniques used to assess swallowing function and determine the most suitable treatment.13–16 However, as these techniques are not readily accessible, we need a swallowing test which is both easy to use and sensitive for detecting dysphagia.
The Spanish Society of Neurology's current treatment guidelines for stroke recommend using the 2 volume/3 texture dysphagia screening test to study dysphagia in stroke patients (www.ictussen.org). Combining the 2 volume/3 texture test with pulse oximetry may improve detection of silent aspiration and reduce the percentage of patients experiencing bronchoaspiration.
Our purpose was to compare bronchoaspiration and mortality rates associated with the new 2 volume/3 texture test with pulse oximetry (2v/3t-P test) to those associated with the 3-oz water swallow test in patients with acute cerebral infarction admitted to the stroke unit (SU).
Patients and methodsWe conducted a prospective study of consecutive stroke patients admitted to the SU at our hospital during a 5-year period.
Between 2008 and 2010, the 3-oz water swallow test9 was used to screen for dysphagia (group 0 [G0]). In contrast, dysphagia screening between 2011 and 2012 consisted of the 2v/3t test plus assessment of 2 additional clinical signs of dysphagia that are not evaluated by this test (drooling at the lip commissure and dyspnoea) and pulse oximetry to monitor oxygen saturation. Group 1 [G1] consisted of patients who had undergone this procedure (2v/3t-P).
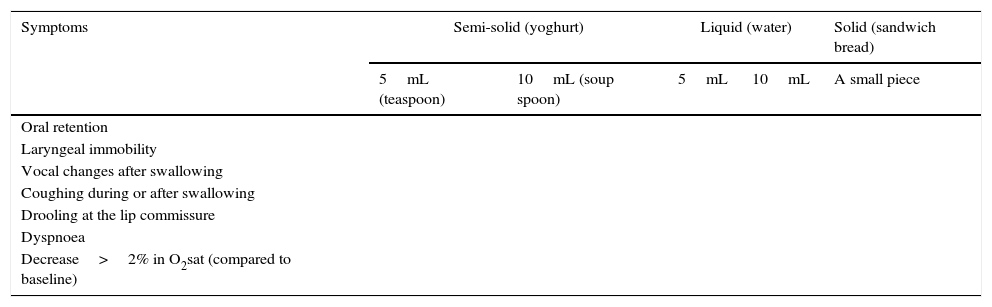
During the 2v/3t-P test, the patient is administered 5mL (a teaspoon) of semi-solid food (yoghurt); if this amount is well tolerated, the patient will then be given 10mL (a soup spoon) of the same food. If the patient tolerates this texture, the same procedure is repeated with water, starting with 5mL and subsequently increasing the volume to 10mL if the patient safely tolerates the initial amount. The third texture is solid food, such as sandwich bread (Table 1). The test evaluates 7 parameters of dysphagia (oral retention, laryngeal immobility, vocal changes after swallowing, coughing during or after swallowing, drooling at the lip commissure, dyspnoea, and a drop of more than 2% in oxygen saturation). The test ends when swallowing alterations are detected.
2 volume/3 texture test with pulse oximetry.
| Symptoms | Semi-solid (yoghurt) | Liquid (water) | Solid (sandwich bread) | ||
|---|---|---|---|---|---|
| 5mL (teaspoon) | 10mL (soup spoon) | 5mL | 10mL | A small piece | |
| Oral retention | |||||
| Laryngeal immobility | |||||
| Vocal changes after swallowing | |||||
| Coughing during or after swallowing | |||||
| Drooling at the lip commissure | |||||
| Dyspnoea | |||||
| Decrease>2% in O2sat (compared to baseline) | |||||
O2sat: oxygen saturation.
At our hospital, nurses administer the swallowing test to all stroke patients at 24 hours from symptom onset (when the level of consciousness allows it), before patients begin any type of oral intake. When dysphagia is detected, a diet is designed based on the volume and texture the patient can tolerate. A speech therapist will then assess swallowing function and provide suitable treatment.
We analysed demographic data, vascular risk factors, neurological status (NIHSS), aetiological subtype (TOAST criteria), clinical subtype (Oxfordshire Community Stroke Project classification), percentage of dysphagia, bronchoaspiration, deaths, and cause of death.
Bronchoaspiration was defined as presence of respiratory crackle on auscultation plus at least one of the following findings: temperature >38°C, positive chest radiography, or purulent sputum requiring antibiotic treatment during hospitalisation at the SU.17
Statistical analysisWe compared mortality and bronchoaspiration rates between G0 and G1 and analysed the independent predictors of each of these events. Qualitative variables were analysed with contingency tables and the chi-square test. The Fisher exact test was used when the expected frequency of any of the cells was less than 5. Quantitative variables were analysed with the t test. The multivariate analysis included those variables with P-values <.1 in the univariate analysis. Statistical significance was set at P<.05.
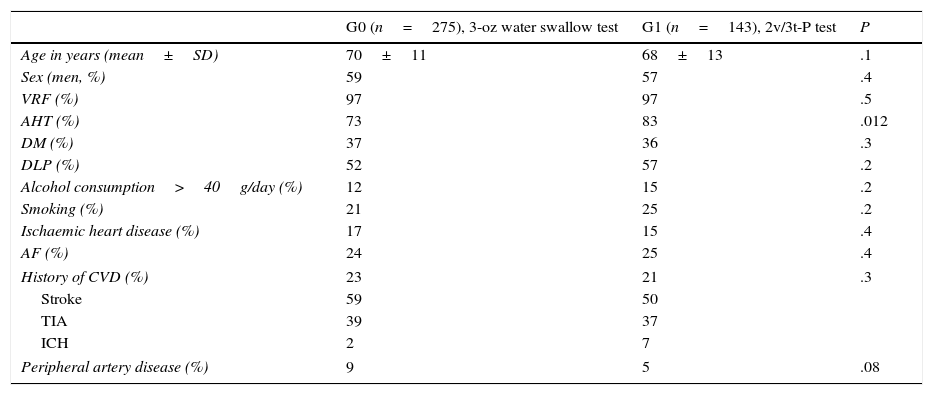
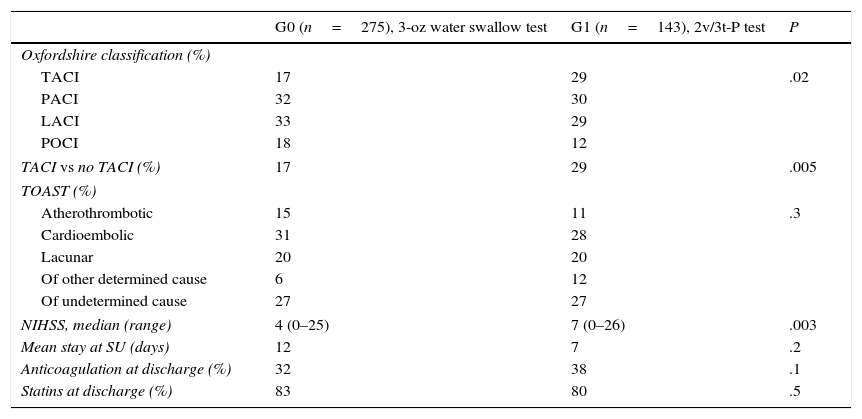
ResultsDuring the study period (5 years), we evaluated 418 patients with acute cerebral infarction who were attended at the SU; 275 were in G0 and 143 in G1. Tables 2 and 3 summarise the demographic characteristics, vascular risk factors, and subtypes of cerebral ischaemia of our sample.
Demographic data and vascular risk factors of our sample.
| G0 (n=275), 3-oz water swallow test | G1 (n=143), 2v/3t-P test | P | |
|---|---|---|---|
| Age in years (mean±SD) | 70±11 | 68±13 | .1 |
| Sex (men, %) | 59 | 57 | .4 |
| VRF (%) | 97 | 97 | .5 |
| AHT (%) | 73 | 83 | .012 |
| DM (%) | 37 | 36 | .3 |
| DLP (%) | 52 | 57 | .2 |
| Alcohol consumption>40g/day (%) | 12 | 15 | .2 |
| Smoking (%) | 21 | 25 | .2 |
| Ischaemic heart disease (%) | 17 | 15 | .4 |
| AF (%) | 24 | 25 | .4 |
| History of CVD (%) | 23 | 21 | .3 |
| Stroke | 59 | 50 | |
| TIA | 39 | 37 | |
| ICH | 2 | 7 | |
| Peripheral artery disease (%) | 9 | 5 | .08 |
TIA: transient ischaemic attack; SD: standard deviation; DLP: dyslipidaemia; DM: diabetes mellitus; CVD: cardiovascular disease; AF: atrial fibrillation; VRF: vascular risk factor; ICH: intracranial haemorrhage; AHT: arterial hypertension.
Characteristics of stroke and hospital stay in both groups.
| G0 (n=275), 3-oz water swallow test | G1 (n=143), 2v/3t-P test | P | |
|---|---|---|---|
| Oxfordshire classification (%) | |||
| TACI | 17 | 29 | .02 |
| PACI | 32 | 30 | |
| LACI | 33 | 29 | |
| POCI | 18 | 12 | |
| TACI vs no TACI (%) | 17 | 29 | .005 |
| TOAST (%) | |||
| Atherothrombotic | 15 | 11 | .3 |
| Cardioembolic | 31 | 28 | |
| Lacunar | 20 | 20 | |
| Of other determined cause | 6 | 12 | |
| Of undetermined cause | 27 | 27 | |
| NIHSS, median (range) | 4 (0–25) | 7 (0–26) | .003 |
| Mean stay at SU (days) | 12 | 7 | .2 |
| Anticoagulation at discharge (%) | 32 | 38 | .1 |
| Statins at discharge (%) | 83 | 80 | .5 |
AHT: arterial hypertension; NIHSS: National Institute of Health Stroke Scale; SU: stroke unit.
No significant differences were seen between groups regarding most vascular risk factors, aetiological subtype, length of hospital stay, and neurological status. The only significant differences were found in the percentages of patients with AHT and the TACI clinical subtype, which were higher in G1.
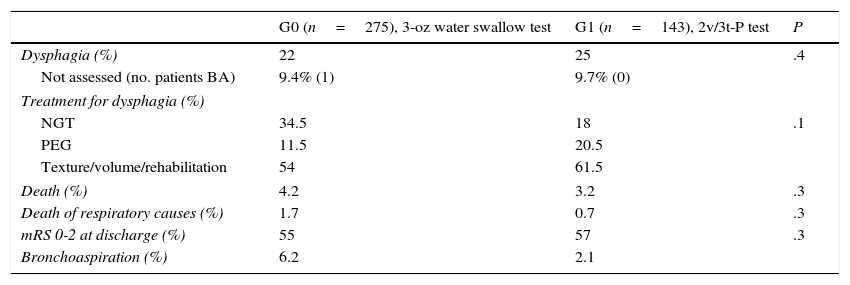
Prevalence of dysphagia was similar in both groups (22% in G0 vs 25% in G1; P=.4); however, the rates of bronchoaspiration (6.2% vs 2.1%; P=.05) and mortality due to respiratory causes (1.7% vs 0.7%; P=.3) were significantly higher in G0 (Table 4).
Prevalence of dysphagia, bronchoaspiration, and mortality in our sample.
| G0 (n=275), 3-oz water swallow test | G1 (n=143), 2v/3t-P test | P | |
|---|---|---|---|
| Dysphagia (%) | 22 | 25 | .4 |
| Not assessed (no. patients BA) | 9.4% (1) | 9.7% (0) | |
| Treatment for dysphagia (%) | |||
| NGT | 34.5 | 18 | .1 |
| PEG | 11.5 | 20.5 | |
| Texture/volume/rehabilitation | 54 | 61.5 | |
| Death (%) | 4.2 | 3.2 | .3 |
| Death of respiratory causes (%) | 1.7 | 0.7 | .3 |
| mRS 0-2 at discharge (%) | 55 | 57 | .3 |
| Bronchoaspiration (%) | 6.2 | 2.1 | |
BA: bronchoaspiration; NGT: nasogastric tube; PEG: percutaneous endoscopic gastrostomy.
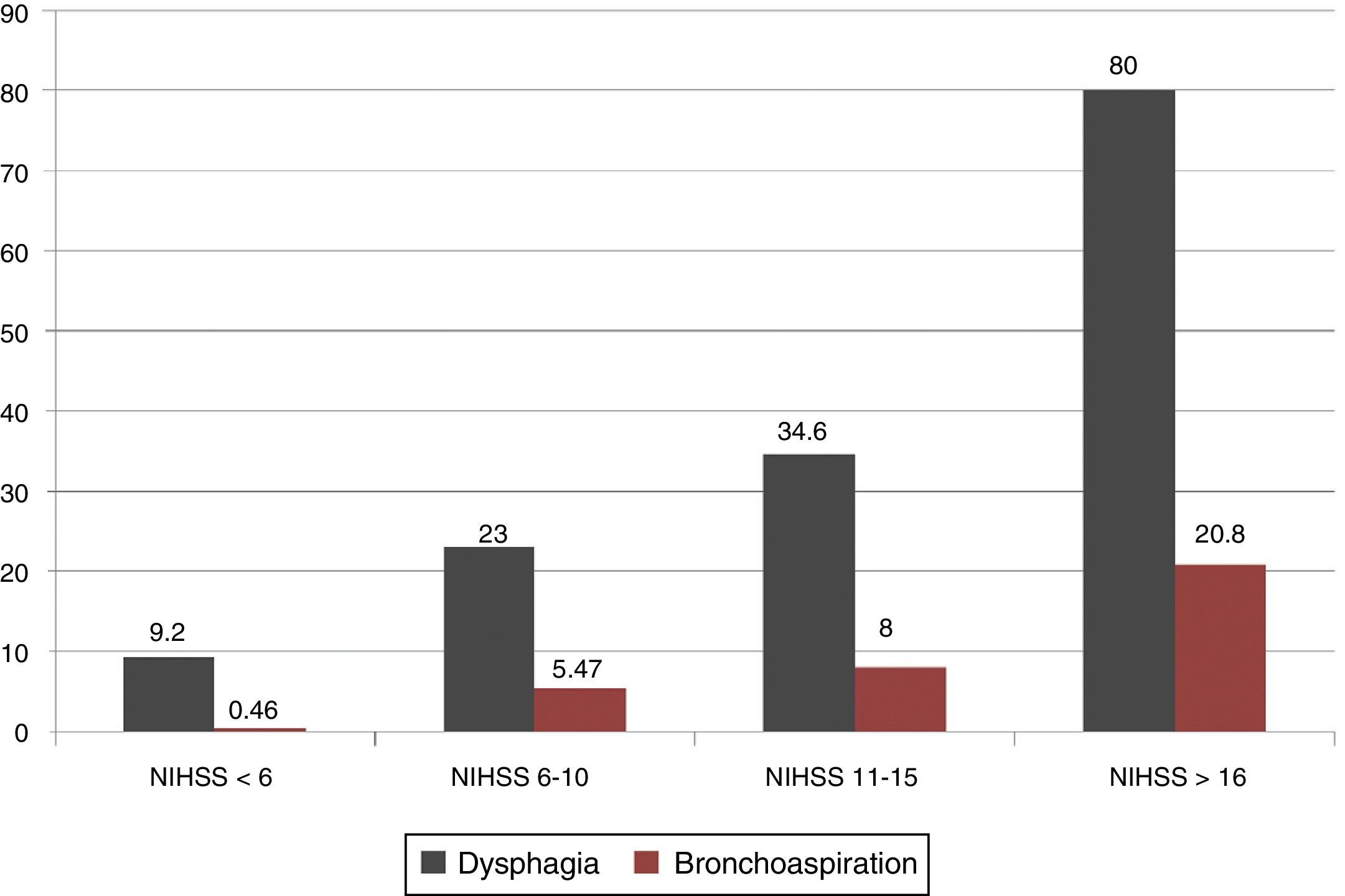
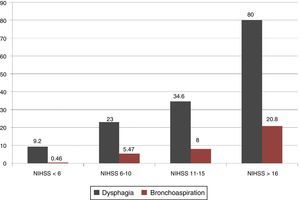
Greater neurological severity according to the NIHSS was associated with a significant increase in dysphagia and bronchoaspiration rates: 80% and 20.8% of the patients with NIHSS scores >16 experienced dysphagia and bronchoaspiration, respectively (Fig. 1).
Prevalence of dysphagia by clinical subtype was distributed as follows: TACI, 60%; PACI, 14%; LACI, 8%; and POCI, 18% (P=.001). Although neurological severity was similar in patients with PACI, LACI, and POCI subtypes (median NIHSS scores of 3, 4, and 3, respectively), dysphagia was more frequent in patients with posterior circulation infarcts.
The rate of bronchoaspiration was higher in patients with TACI and POCI (TACI, 10%; PACI, 4%; LACI, 2%; POCI, 6%; P=.002).
Dysphagia and bronchoaspiration rates according to the screening test usedOf the total sample, 282 patients showed no dysphagia (185 in G0 and 97 in G1); however, one patient without dysphagia from G0 did experience bronchoaspiration, vs none from G1.
Dysphagia was detected in 96 patients (60 in G0 and 36 in G1), 18 of whom (19%) experienced bronchoaspiration; this event was significantly more frequent in G0 (15 patients, 25%) than in G1 (3 patients, 8%) (P=.04). Therefore, presence of dysphagia increased bronchoaspiration rates by 20%; none of the patients with no dysphagia and evaluated with the 2v/3t-P test experienced bronchoaspiration.
Of the subset of patients with dysphagia, 26.6% required a nasogastric tube, 16% underwent gastrostomy feeding tube placement due to dysphagia predicted to last for more than 6 weeks, and the remaining 57.4% followed a personalised diet and received rehabilitation.
Swallowing function was not assessed in 40 patients (9.4% in G0 vs 9.7% in G1); bronchoaspiration rates were similar for both groups (1 patient in G0 vs none in G1) (Table 4).
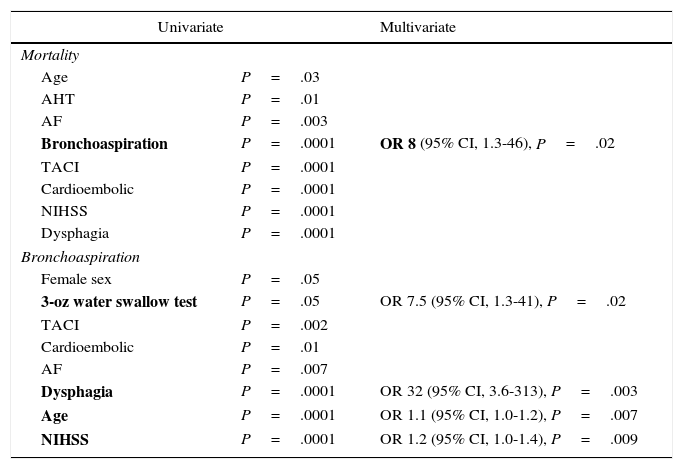
Predictors of mortality and bronchoaspirationThe following variables were found to act as predictors of mortality in the univariate analysis: age, AHT, atrial fibrillation, bronchoaspiration, TACI clinical subtype, cardioembolic aetiological subtype, NIHSS score, and presence of dysphagia. However, the multivariate analysis of these factors found that only presence of bronchoaspiration continued to display a statistically significant association with mortality, with an OR of 8 (95% CI, 1.3-46; P=.02).
According to the univariate analysis, the following factors were found to act as predictors of bronchoaspiration: female sex, using only the 3-oz water swallow test, TACI clinical subtype, cardioembolic aetiological subtype, atrial fibrillation, dysphagia, age, and NIHSS score. In the multivariate analysis, using the 3-oz water swallow test (OR 7.5, 95% CI, 1.3-41; P=.02), dysphagia (OR 32, 95% CI, 3.6-313; P=.003), age (OR 1.1, 95% CI, 1.0-1.2; P=.007), and NIHSS scores (OR 1.2, 95% CI, 1.0-1.4; P=.009) continued to display a statistically significant association with bronchoaspiration (Table 5).
Analysis of the independent predictors of bronchoaspiration and mortality.
| Univariate | Multivariate | |
|---|---|---|
| Mortality | ||
| Age | P=.03 | |
| AHT | P=.01 | |
| AF | P=.003 | |
| Bronchoaspiration | P=.0001 | OR 8 (95% CI, 1.3-46), P=.02 |
| TACI | P=.0001 | |
| Cardioembolic | P=.0001 | |
| NIHSS | P=.0001 | |
| Dysphagia | P=.0001 | |
| Bronchoaspiration | ||
| Female sex | P=.05 | |
| 3-oz water swallow test | P=.05 | OR 7.5 (95% CI, 1.3-41), P=.02 |
| TACI | P=.002 | |
| Cardioembolic | P=.01 | |
| AF | P=.007 | |
| Dysphagia | P=.0001 | OR 32 (95% CI, 3.6-313), P=.003 |
| Age | P=.0001 | OR 1.1 (95% CI, 1.0-1.2), P=.007 |
| NIHSS | P=.0001 | OR 1.2 (95% CI, 1.0-1.4), P=.009 |
AF: atrial fibrillation; AHT: arterial hypertension; 95% CI: 95% confidence interval; NIHSS: National Institute of Health Stroke Scale; OR: odds ratio.
In our study, 23% of the patients with acute cerebral infarction presented dysphagia; rates were higher among patients with a more severe neurological status and those with posterior circulation infarcts.
Bronchoaspiration was found in 5% of the total sample; the main independent predictor of risk for bronchoaspiration was presence of dysphagia (OR 32), followed by use of the 3-oz water swallow test (OR 7.5). In patients with dysphagia, the new 2v/3t-P test managed to reduce bronchoaspiration by 17% compared to the 3-oz water swallow test; none of the patients without dysphagia (as assessed by the 2v/3t-P test) experienced bronchoaspiration.
Aspiration is the entry of material into the larynx below the vocal cords; this phenomenon is especially frequent when swallowing liquids.15 Detecting aspiration based on clinical signs at bedside is an imprecise method. According to several studies, positive predictive values for detection of aspiration using bedside swallow testing range between 50% and 75% compared to videofluoroscopy13; detection capacity of these tests should therefore be improved. A recent study11 evaluated changes in oxygen desaturation with pulse oximetry during videofluoroscopy. This study showed that a decrease >2% of baseline oxygen saturation was correlated with aspiration, with a sensitivity of 87%.
According to the literature, between 19%18 and 81%1,3 of stroke patients have dysphagia. Differences in dysphagia incidence rates may be explained by variations in screening methods, time after stroke, and lesion localisation.2 Prevalence of dysphagia ranges between 30% and 55% in studies using more exhaustive swallowing tests2; the studies including patients with hemispheric lesions usually report lower rates (39%-40%) than those also including patients with brainstem lesions (51%-55%).2
Dysphagia rates in our sample were lower than those reported in previous studies. This finding may reflect the inclusion of patients with acute cerebral ischaemia but not of patients with cerebral haemorrhages or those admitted to rehabilitation centres. Overall, neurological status in our sample was not severe (median NIHSS score of 5; range 0-38), which may also explain these differences.
All types of stroke, regardless of localisation, may cause dysphagia.2 Hemispheric lesions affect voluntary control of mastication and bolus transport during the oral phase,19,20 whereas cortical lesions affecting the precentral gyrus alter contralateral facial, lip, and tongue motor control as well as reducing contralateral pharyngeal peristalsis.21 Brainstem infarctions are less frequent than hemispheric infarctions, but they lead to more severe swallowing impairment since they result in sensory dysfunction of the mouth, tongue, and cheeks; impaired cough reflex; reduced elevation of the larynx; reduced laryngeal closure; and cricopharyngeal dysfunction.21,22 In our study, patients with posterior circulation infarcts presented dysphagia and bronchoaspiration more frequently than those with other clinical subtypes of stroke despite having a similar neurological status; these findings agree with those reported in the literature.
The 3-oz water swallow test9 is one of the most widely used screening tests for dysphagia. However, this test uses a large amount of a low-viscosity liquid (water) and regards coughing as the sole indicator of aspiration, although this reflex is absent in up to 40% of the patients with cerebrovascular diseases.10 Another important limitation of this test is the fact that it does not evaluate swallowing effectiveness and cannot therefore be used to analyse whether other textures or volumes are well tolerated by patients. We may therefore conclude that the 3-oz water swallow test is associated with a high risk for patients for 2 main reasons: it may erroneously detect which patients may safely resume oral intake and it does not assess swallowing effectiveness.
In our hospital, we have designed a simple test which uses 2 volumes and 3 different textures to evaluate 7 parameters of dysphagia, including oxygen desaturation. This test has achieved lower rates of bronchoaspiration and mortality than the 3-oz water swallow test in our hospital's SU since it assesses swallowing more thoroughly and helps us adapt diet to each patient's needs.
Previous studies have shown that dysphagia is an important predictor of poor outcome. Some 50% of all patients with dysphagia will experience bronchoaspiration, and one third of these will develop pneumonia, a factor associated with a three-fold increase in the risk of in-hospital mortality at 30 days.1,2,5 In our study, the risk of mortality due to bronchoaspiration was higher than that cited in previous studies; according to our data, bronchoaspiration leads to an eight-fold increase in the risk of mortality. Preventing bronchoaspiration is therefore essential to reduce mortality. The main predictors of bronchoaspiration were dysphagia (OR 32) and using the 3-oz water swallow test (OR 7), findings which underscore the importance of detecting dysphagia correctly.
Our study has a number of limitations.
- 1)
The results of the 2v/3t-P test may stem from increasing awareness in recent years of the need to treat dysphagia. However, the incidence of dysphagia in our study was similar in both groups; therefore, our results may not be due to increased detection of dysphagia but rather to better assessment of swallowing function provided by the new test. A randomised study should be conducted to avoid this bias and evaluate the real benefits of the 2v/3t-P test.
- 2)
This test, which evaluates more clinical parameters of dysphagia (including oxygen saturation), is a new version of an existing test and has not been validated. However, a validation study using fibreoptic endoscopy as the gold standard is currently underway in our centre.
- 3)
Our results were drawn from an SU with specialised nursing staff and a very different nurse-to-patient ratio from those of other units; therefore, our results may not be extrapolated to the general population.
Dysphagia, a very frequent complication among stroke patients, increases the risk of poor functional prognosis and mortality. Multiple studies have shown the importance of early diagnosis and treatment of dysphagia cases, which results in decreased morbidity and mortality rates, shorter hospital stay times, and lower healthcare costs.5,8,23 To date, no standard tool has been validated as a screening tool for swallowing dysfunction. The 2v/3t-P test is a simple tool that can be used by nursing staff at bedside. According to our study, it improves assessment of swallowing function and decreases bronchoaspiration rates compared to using the 3-oz water swallow test. Future studies should be carried out to validate our findings and this screening tool.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Cocho D, Sagales M, Cobo M, Homs I, Serra J, Pou M, et al. Reducción de la tasa de broncoaspiración con el test 2 volúmenes/3 texturas con pulsioximetría en una unidad de ictus. Neurología. 2017;32:22–28.
This study was presented orally at the 64th Annual Meeting of the Spanish Society of Neurology (Neurología. 2012;27 Suppl C:57).