Superficial siderosis of the nervous system is a clinical syndrome arising from the deposition of haemosiderin on the surface of the pia mater and adjacent central nervous system cells. Its harmful effect destroys superficial neurons, especially those in the cerebellum, brain stem and medulla, which leads to gliosis and fibrosis.1 There may be a number of clinical manifestations, but the most common are hearing loss, ataxia and exaggerated deep tendon reflexes.2 Other symptoms are only present in less than half of all cases.3
Superficial siderosis of the nervous syndrome is a rare disease. As of 1999, only 95 cases had been described in the medical literature.3 The age of diagnosis ranges from 14 to 77years, with death occurring between 1 and 38years after diagnosis.2
Aetiology is never determined in many cases. In cases in which the source of the haemorrhage is identified, the most frequent causes are disease of the dura mater (47%), pseudomeningocele and tumours (35%). Cases have also been described in which surgical procedures, especially hemispherectomy and brain tumour excision, caused the syndrome.4
We present the clinical case of male aged 47years who 21years earlier had undergone surgery for intraspinal meningioma at the T4–T5 spinal level (discharged in July 1988). A year after surgery, he began experiencing severe stabbing headaches with significant psychomotor agitation but no rhinorrhoea, lacrimation or ptosis.
His headaches became increasingly frequent, resulting in his being unable to work by late 2004. Triptans were ineffective, as was prophylaxis with propranolol and amitriptyline. We prescribed prophylactic treatment with methysergide and flunarizine, which resulted in shorter, more sporadic and less intense headache episodes. Methysergide was discontinued in March 2008.
Radiology images (chest and abdomen) and peripheral vascular system assessments were consistently normal.
In January 2009, the patient came to the emergency department due to an intense headache episode that had begun 2days prior. Findings from the neurological examination were normal, with no meningeal signs. Prednisolone 40mg was administered intravenously every 12h. Pain subsided 12h after beginning treatment.
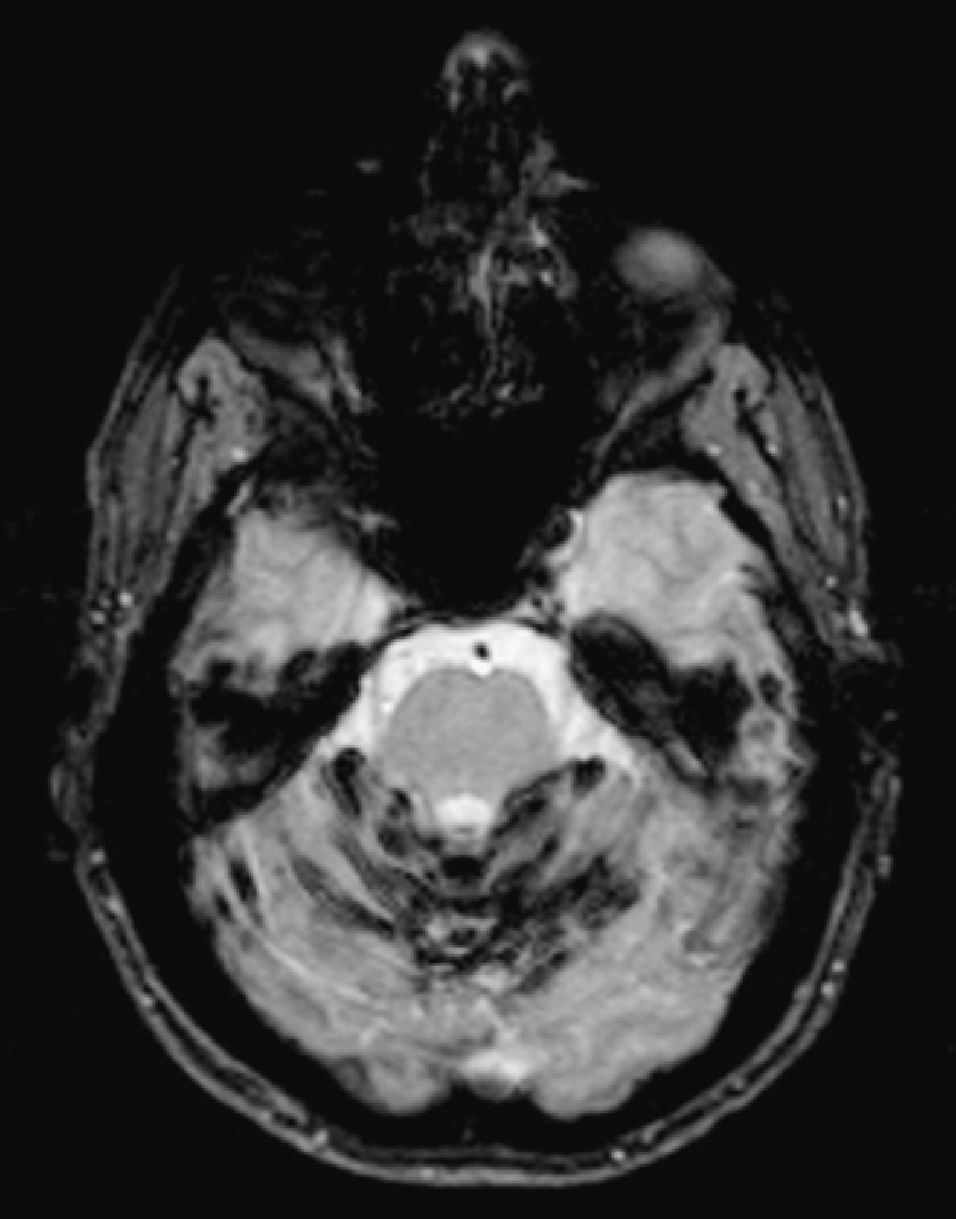
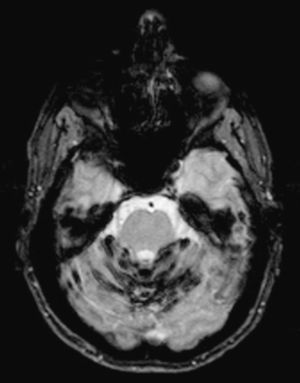
Cerebral magnetic resonance imaging (MRI) (Philips Intera 1.5T) showed an obvious linear hypointense band along the leptomeningeal surface of the cerebellar vermis, and to a lesser extent, along the cerebral leptomeningeal surfaces. This was compatible with superficial siderosis due to the deposition of blood breakdown products. Superior cerebellar vermis fissures were slightly widened due to focal atrophy. These findings were more evident in T2-weighted GE sequences (Fig. 1).
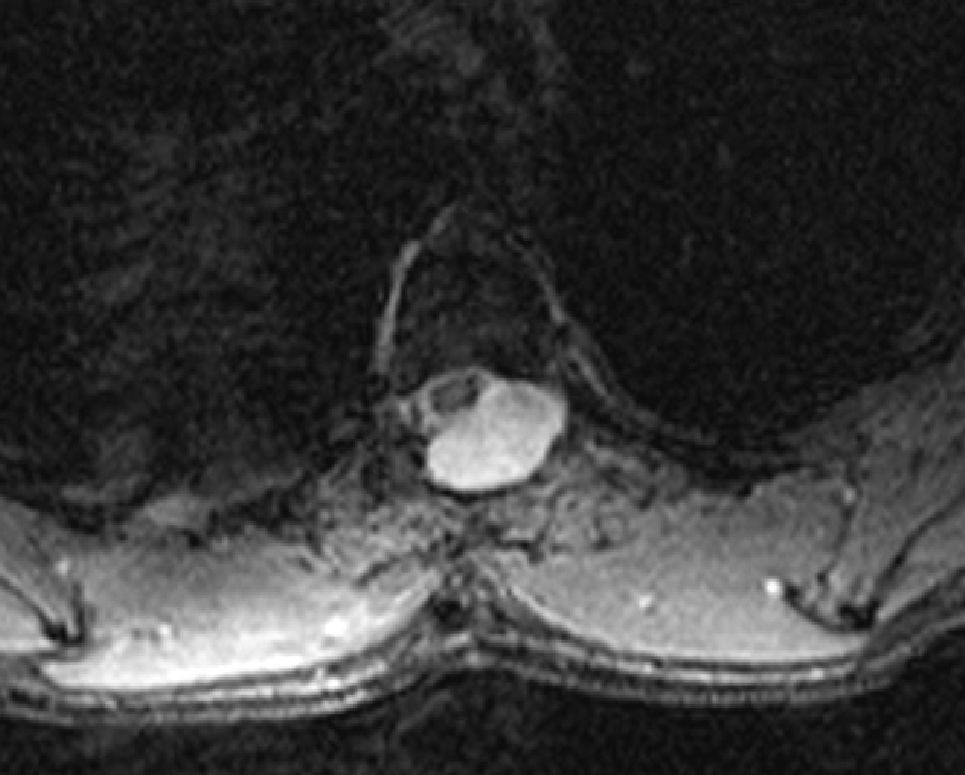
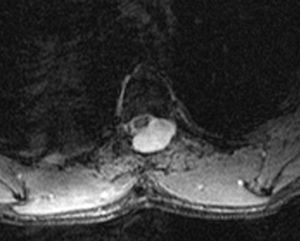
Spinal MRI showed dorsal surgical alterations with resection of posterior structures and a large left posterolateral pseudomeningocele at the T4–T5 level, where the tumour had been resected, which was displacing the spinal cord and remodelling adjacent spinal structures. We observed no significant abnormalities in the spinal MR image except for a faint peripheral halo in GE sequences at the surgical location. This probably also corresponded to mild meningeal siderosis (Fig. 2).
Cerebrospinal fluid (CSF) had a slightly xanthochromic appearance and contained 12 red blood cells per mm3, with low monocyte, lymphocyte and neutrophil counts. The protein level was 0.5/l.
Neurological examinations did not reveal cerebellar syndrome, ataxia, or hypoacusia, which are all common manifestations of superficial siderosis.2,5–7 The patient presented hyperreflexia of the lower extremities as a result of spinal cord compression caused by the tumour removed in 1988. Compression may have continued due to the action of the pseudomeningocele during surgery. No deterioration of higher functions was observed.
The cerebral MRI taken upon the patient's most recent hospital admission led to the diagnosis by revealing siderosis, especially in the cerebellum (Fig. 1). Meticulous examination of the cerebral MRI scans taken in 1989 and 2000 revealed the presence of small siderin deposits on the cerebellar hemispheres and vermis which were not assessed at the time. MRI is so sensitive to haemosiderin and ferritin deposits that it may permit diagnosis of superficial siderosis in the presymptomatic period, which may last up to 30years. This might explain why some of the syndrome's more typical clinical manifestations were absent in this patient.
The case is similar to those described by Kumar et al,5 Anderson et al4 and Kole et al,6 in that a post-surgical pseudomeningocele was present and probably related to chronic haemorrhaging. The surgical procedure for the bleeding pseudomeningocele performed by Kole et al6 seems to be the only case of successful treatment. At present, due to his symptoms having improved, the patient has declined a surgical examination to determine the source of the bleeding that caused the syndrome. The cause of the headaches remains unidentified, but they may have been secondary to episodes of subarachnoid bleeding with meningeal irritation or CSF leak syndromes related to the pseudomeningocele.
Please cite this article as: Balcells Riba M, Grivé Isern E. Siderosis meníngea. Estudio de un caso y revisión de la literatura médica. Neurología. 2012; 27(4):247–8.