Percutaneous transluminal angioplasty of the carotid with endovascular stent placement is an interventional therapeutic procedure indicated for atherosclerotic stenosis in selected patients,1 as an alternative to carotid endarterectomy. However, there are no standard guidelines for its use in acute carotid thrombosis.
Mechanical thrombectomy using a Merci retriever (mechanical embolus removal in cerebral ischaemia) is an intracranial arterial recanalisation procedure that extracts the thrombus by mechanical means.2 This technique is indicated in patients with intracranial occlusion of medium-sized arteries, usually the M1 segment of the middle cerebral artery (MCA) or the basilar artery. It may be used as a therapeutic option following failure of intravenous or intra-arterial thrombolysis, or as a primary recanalisation procedure performed during the first 8 hours.2
Fresh carotid thrombi caused by acute intracranial embolism are uncommon, and treating them is generally challenging, as in the case we describe here.
Male patient aged 45 years was admitted with a personal history of adenoid cystic carcinoma in the right submandibular gland. Cancer was treated with radiotherapy and chemotherapy, and is currently in full remission. The patient had no history of vascular risk factors. A routine CT angiography of the supra-aortic arteries ordered as part of an oncology consult revealed dilation of the right carotid bulb with a small laminar mural thrombus. Two months after this scan, the patient came to the emergency room due to sudden onset of weakness in the left extremities, loss of left facial and brachiocrural sensitivity, right facial droop and difficulty articulating words; his NIHSS score was 16.
Laboratory analyses and an emergency electrocardiogram and chest radiography did not reveal any relevant results. The cerebral CT showed indirect signs of acute cerebral ischaemia in the vascular territory of the right MCA (RMCA). The patient was admitted to the stroke unit and began receiving treatment with intravenous rtPA 4h after symptom onset. His NIHSS score was 14 at 2 hours after beginning fibrinolytic treatment.
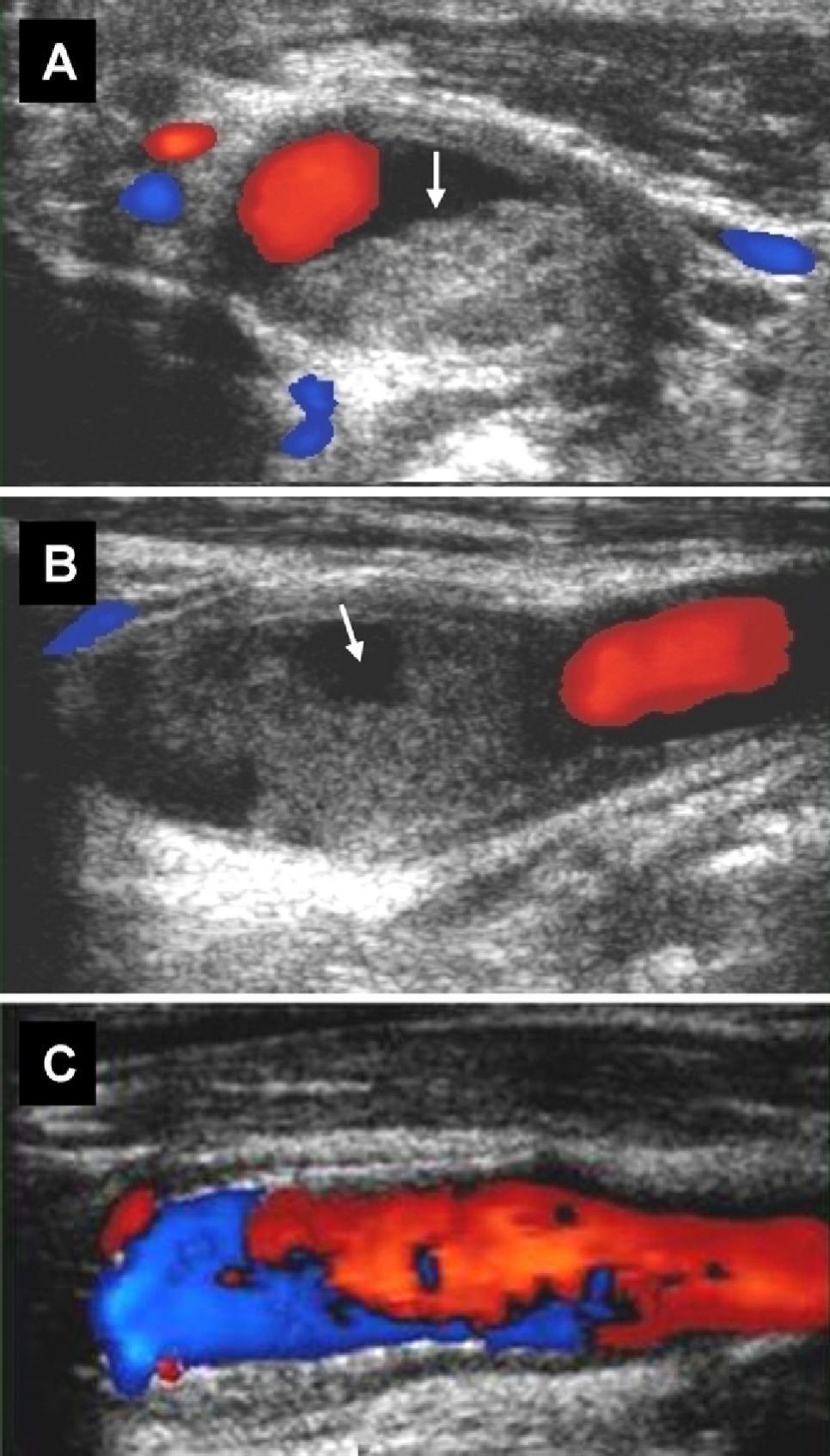
An emergency transcranial Doppler scan taken during administration of rtPA showed occlusion of the RMCA from its M1 segment. Carotid duplex showed a very large fresh thrombus originating in the distal end of the right common carotid artery and stretching to the carotid bifurcation. The surface of the thrombus showed signs of a recent break, and the thrombus was not causing haemodynamically significant stenosis (Fig. 1). Ultrasound findings were confirmed by CT angiography of the cerebral and supra-aortic arteries.
Carotid duplex scan. Image A shows a transverse image of the right carotid bifurcation containing a thrombus (arrow). It can also be seen in the longitudinal view (B), which shows the artery's ulcerated surface (arrow). Blood flow velocities around the thrombus are not indicative of haemodynamically significant stenosis. Image C shows the carotid bifurcation after placement of the stent.
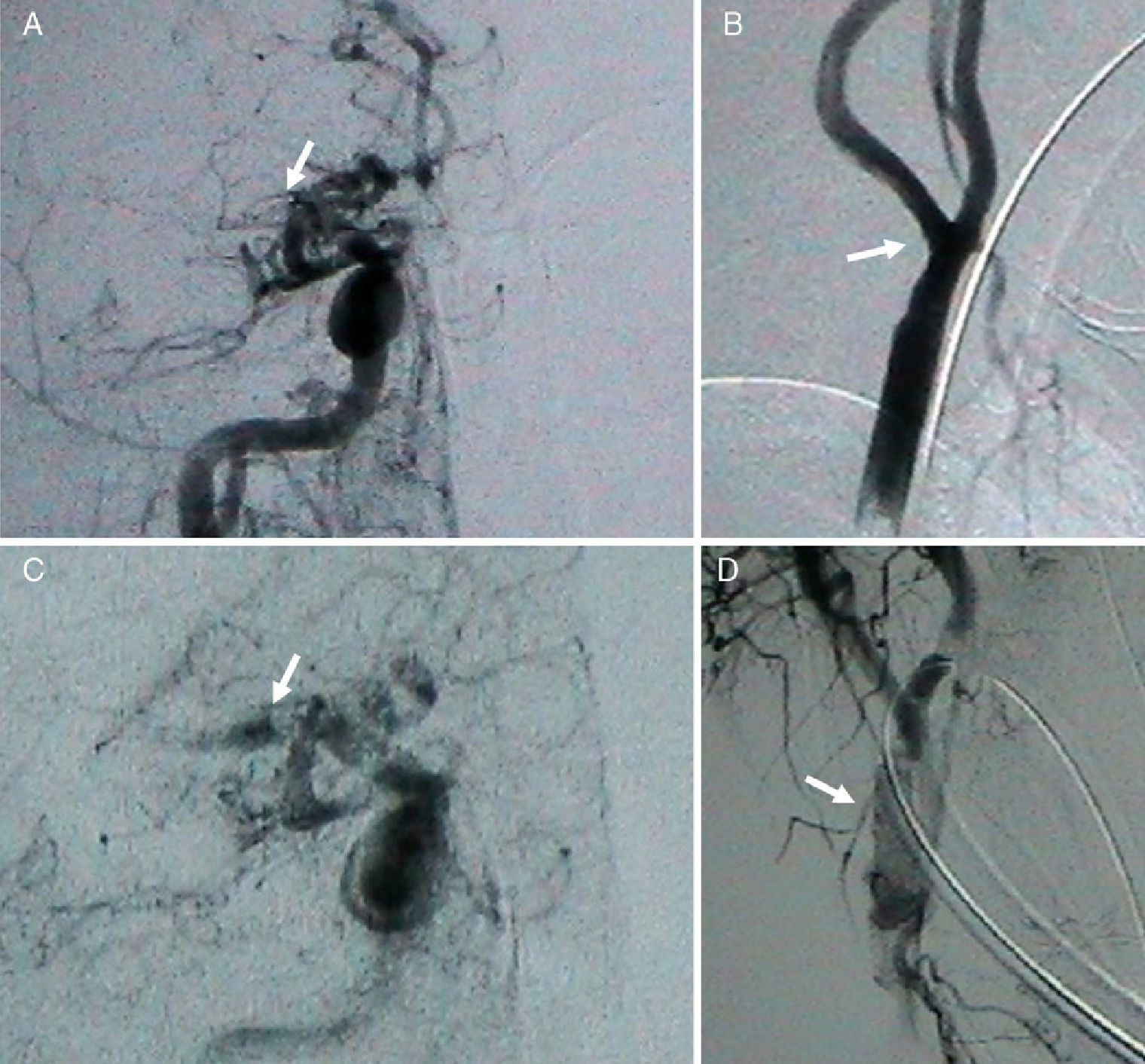
Given persistent symptoms and the presence of an occlusion in the RMCA, doctors opted for endovascular treatment. Since the 6-hour window for intra-arterial rtPA treatment had ended, they proposed mechanical RMCA thrombectomy using a Merci retriever. However, the large thrombus at the ipsilateral carotid bifurcation posed a risk of fracturing once more and releasing emboli during use of the Merci retriever. After running a risk-benefit analysis, we opted to place a stent at the level of the carotid thrombus. Prior to this, a protective filter was placed at the distal end and systemic heparin was administered in order to move the thrombus towards the arterial wall, eliminate the risk of fragmentation and facilitate access through the occlusion and towards the intracranial vascular territory. After placement of the carotid stent, the thrombus was partially extracted with a single pass of the Merci device, resulting in partial recanalisation of the M1 segment (Fig. 2). The Merci retriever was not employed again since the carotid stent had just been placed. Dual antiplatelet therapy with aspirin 100mg and clopidogrel 75mg was administered.
Arteriography. Image A shows the vascular territory of the anterior intracranial artery. Note the lack of blood flow in the entire right middle cerebral artery (RMCA) and its branches (arrow). Image B shows the cervical part of the internal carotid artery and the right carotid bifurcation with signs of mural thrombus (arrow). Image C shows the RMCA after thrombectomy using the Merci retriever. The M1 portion of the RMCA is now visible (arrow). Image D shows the stent placed in the right carotid bifurcation (arrow).
A subsequent cerebral CT showed a partial anterior circulation infarct in the vascular territory of the RMCA, which affected the vascular territory of the lenticulostriate branches. Routine radiology imaging did not reveal haemorrhagic transformation. At a later point, full recanalisation could be observed using transcranial duplex ultrasound. On a clinical level, the patient had an NIHSS score of 10 at 48 hours after the procedure, which dropped to 5 after 2 months (3 on the modified Rankin scale). One year later, the patient had experienced no further neurological events and the stent in the carotid bifurcation continues maintaining patency.
It is uncommon for a mural carotid thrombus with no associated atheromatosis to cause a stroke, and the best treatment has yet to be identified. In this case, we observed a very large and fragmented mural thrombus associated with an occlusion in the ipsilateral MCA, and produced by an artery-to-artery embolism.
In 1963, Gunning et al.3 were the first to describe mural carotid thrombi in a series of 16 patients with varying degrees of stenosis and protrusion towards the arterial lumen. Treatment approaches also varied greatly at the time. However, doubts still remain as to the best treatment for an unstable thrombus on the internal carotid artery wall. If haemodynamically significant stenosis is present, treatments employing carotid endarterectomy or angioplasty with a stent are widely accepted.4 However, the best treatment for mural or intraluminal thrombi that are not causing significant stenosis is unknown. Doctors have used various empirical treatments including emergency carotid surgery, antiplatelet drugs and even anticoagulant therapy with heparin.5
One method that is less invasive than surgery is the placement of a carotid stent, although experience is based on isolated cases that are not sufficient to demonstrate treatment efficacy. In the present case, the sizeable risk involved in inserting and moving the Merci retriever catheter tip through the lumen of the mural thrombus led to the decision to use a stent to stabilise the thrombus. Medium term results have been satisfactory.
In conclusion, there is no standard optimal treatment for tandem internal carotid artery/middle cerebral artery occlusions, with an unstable mural thrombus in the internal carotid artery. However, emergency placement of a stent may be a treatment option in selected cases.
Please cite this article as: Cazorla García R, et al. Angioplastia carotídea y trombectomía intracraneal simultánea en un ictus agudo. Neurología. 2012;27(4):249–51.