Cervical artery dissection (CAD) results from the subintimal penetration of blood and subsequent longitudinal extension of the intramural haematoma between different layers of the vessel.1 The pathophysiology of the condition is not known. It has been suggested that, in addition to minor trauma, such environmental factors as acute infection may act as trigger factors in predisposed individuals.2 Fifteen percent of patients may present multiple CADs simultaneously3; however, dissection of more than 2 cervical arteries is extremely rare.4 We present the case of a patient with simultaneous, progressive dissection of 3 cervical arteries, occurring concurrently with upper respiratory tract infection.
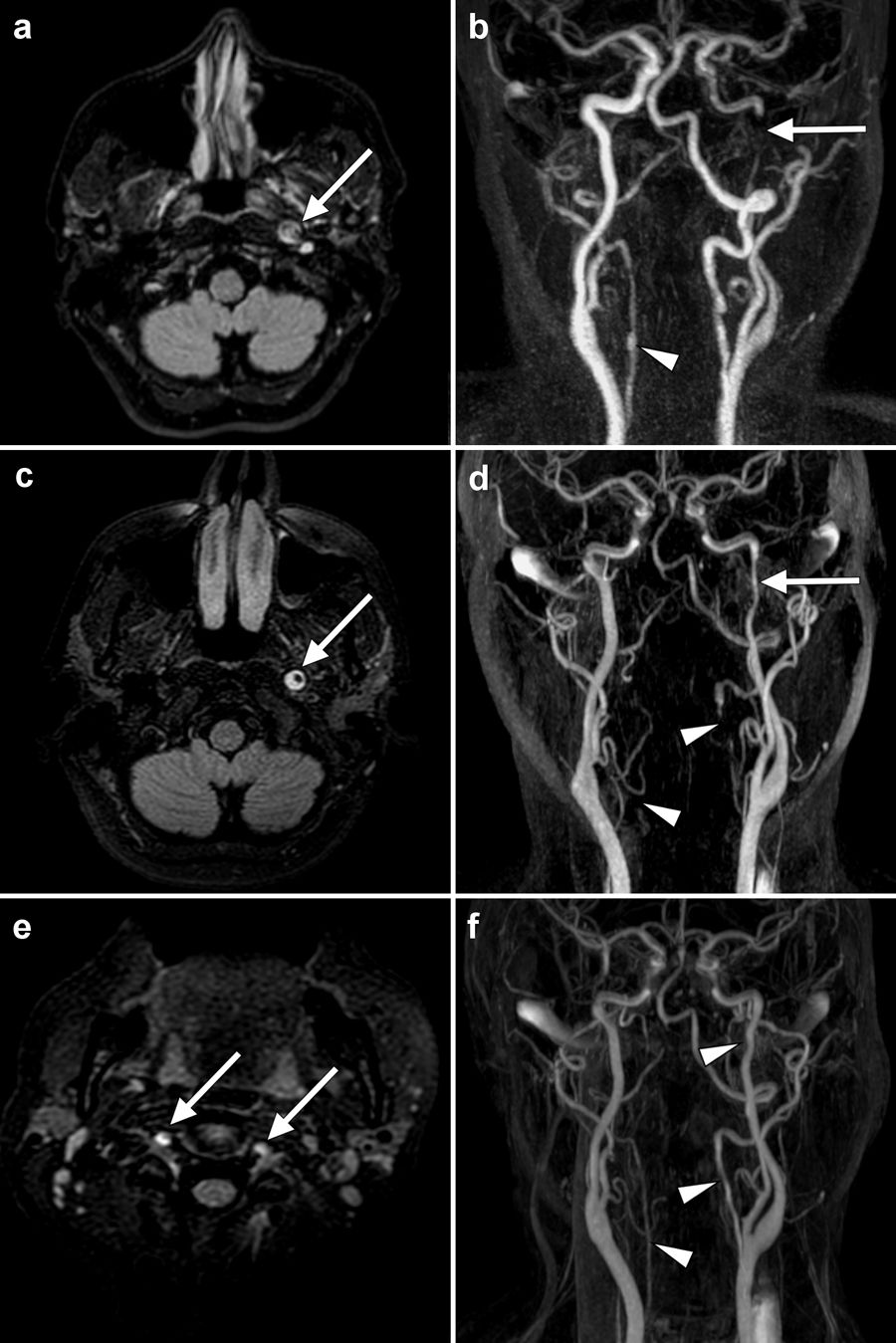
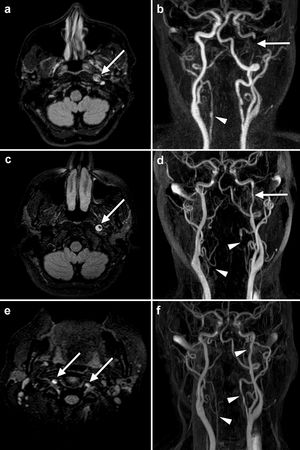
The patient was a 45-year-old woman who consulted due to ptosis and miosis in the left eye associated with severe headache. She reported a 3-day history of sore throat, cough, and fever (up to 39°C). Physical examination detected left-sided Horner syndrome and no other abnormalities. Blood analysis detected elevated levels of inflammatory markers, including mild leukocytosis, fibrinogen level of 410 mg/dL, and ultrasensitive C-reactive protein level of 3.22 mg/dL. An electrocardiography study, chest radiography, and head CT scan all returned normal results. A neurosonology study revealed absence of flow in the terminal segment of the internal carotid artery; slow, dampened flow in the left middle cerebral artery; and reverse flow in the A1 segment of the left anterior cerebral artery, with opening of the ipsilateral posterior communicating artery, feeding the left middle cerebral artery. A brain MRI scan with an angiography sequence confirmed dissection of the left internal carotid artery (Fig. 1a and b); no ischaemic lesions were observed. The absence of clinical events or radiological lesions suggestive of brain ischaemia was related to the compensation of brain haemodynamics through the opening of collateral arteries, as shown in the neurosonology study. We started treatment with analgesics and anticoagulants. The patient was discharged home after headache resolved.
MRI sequences showing the progression of cervical artery dissection in our patient. The initial study (a and b) showed hyperintensity of the intramural thrombus (arrow) in the distal cervical segment of the left internal carotid artery (a: FLAIR sequence) and a filling defect (arrow) compatible with dissection (b: angiography sequence). An irregularity in the right vertebral artery (arrowhead) initially went undetected in this study. One month later (c, d, e) the crescent sign (arrow) persisted in the left internal carotid artery (c: FLAIR sequence), although blood flow had improved (d: angiography sequence). The extracranial segment of both vertebral arteries (e: FLAIR sequence) also showed increased signal intensity (arrows), which was correlated with lack of flow (d: angiography sequence; arrowheads), suggesting bilateral vertebral artery dissection. Angiography sequences obtained 6 months after onset (f) show restoration of blood flow in the left internal carotid artery and both vertebral arteries (arrowheads).
The patient was readmitted 3 weeks later due to recurrence of very severe headache. A second MRI study showed bilateral dissection of the vertebral arteries (Fig. 1c-e). We reviewed the original study (Fig. 1b), and identified slight irregularities in the extracranial vertebral arteries, which had initially gone undetected. Due to progression of the haematoma, anticoagulation was replaced with antiplatelet treatment with acetylsalicylic acid. Further testing was performed. Microbiology testing returned negative results. Antinuclear antibodies were detected at a titre of 1:320, with a homogeneous pattern, although the patient did not present definite signs of rheumatic disease. Chest and abdomen CT angiography findings were not compatible with fibromuscular dysplasia or other vasculopathies. The patient progressed favourably after a prolonged hospital stay to control pain. Six months after onset, a follow-up MRI study (Fig. 1f) showed incomplete resolution of the CAD. From a clinical perspective, headache has not recurred and she has presented no ischaemic events; the only persisting symptom is left-sided Horner syndrome.
The interest of this case lies in the simultaneous involvement of 3 of the 4 cervical arteries responsible for supplying the brain, the recent history of infection, and the progressive course. Triple and even quadruple CADs are extremely rare, affecting 1.5% and 0.1% of patients with spontaneous CAD, respectively.4 Recent history of infection (typically respiratory infection)5,6 is reported in up to 32% of patients with spontaneous CAD,7 and is 3 times as common in those with brain ischaemia of other causes and 6 times more frequent in patients with multiple dissections than in those with single dissections.5 The mechanism underlying this association is unclear. Mechanical mechanisms such as coughing, sneezing, or vomiting are insufficient.6 As with our case, these patients present high levels of inflammatory markers,7,8 which suggests inflammation may play a role in pathogenesis. It has been suggested that infection may trigger an inflammatory response that, through the release of cytokines and proteases, damages the extracellular matrix and weakens vessel walls.5,9 This may be especially relevant in susceptible patients with underlying arteriopathies or connective tissue diseases, who are at greater risk of multiple dissection.3,10 Overall, in the absence of other alterations, the literature suggests that the underlying disorder in these patients may be a transient vasculopathy.4
Another interesting aspect of this case was the recurrence of headache after the initial hospitalisation. While the patient initially consulted due to Horner syndrome, her intense headache was the most disabling symptom, and led to readmission. This enabled us to detect the progression of arterial dissection, which probably explained the worsening of headache. This is a fundamental finding that should alert us to the possibility of disease progression.
Finally, we should note a series of considerations regarding treatment. Firstly, recent studies indicate that patients with involvement of multiple arteries are 3 times more likely to present brain ischaemia or subarachnoid haemorrhage than patients with only one dissected artery.9 Secondly, while the CADISS (Antiplatelet Treatment Compared with Anticoagulation Treatment for Cervical Artery Dissection) trial found no significant differences in efficacy between anticoagulation and antiplatelet treatment in patients with CAD,11 no study to date has compared both treatments in patients with multiple CADs. While we initially opted to administer anticoagulation treatment, we decided to switch to antiplatelets, which we considered to be a safer option, in view of the progression of the haematoma, the detection of vertebral artery involvement (which is associated with higher risk of intracranial extension and therefore of subarachnoid haemorrhage), and the absence of brain ischaemia until that time. In any case, it should be noted that there are no data in the literature confirming that anticoagulant treatment contributes to the extension of the haematoma; we would expect this phenomenon to be rare, given the findings of studies into intravenous fibrinolysis in patients with CAD.12 Therefore, further studies are needed to determine the most suitable pharmacological treatment for patients with multiple CADs.
In conclusion, physicians should be alert to the possibility of multiple, simultaneous CADs. There is a need for research into the association with recent history of infection, and close monitoring is needed to prevent potentially fatal complications; headache progression should be considered a key marker of disease progression.
Ethical standardsThe patient gave informed consent for the publication of this case report.
Please cite this article as: Rodríguez-Castro E, Mosqueira AJ, Santmaría-Cadavid M, Arias-Rivas S. Disección triple y progresiva de las arterias cervicales asociada a infección respiratoria del tracto superior. Neurología. 2021;36:177–179.