Horner syndrome is characterised by ptosis secondary to paralysis of the superior tarsal muscle, miosis, pseudoenophthalmos, and, on occasion, anhidrosis or hypohidrosis.1 The condition may result from a number of causes, including head or neck trauma, brain haemorrhage, cervical disc disease, neck or apical lung tumours, stroke, lateral medullary syndrome, cluster headache, carotid artery dissection, multiple sclerosis, syringomyelia, acute transverse myelopathy, and thoracic aortic aneurysms.2 Carotid artery dissection is the most frequent cause of painful Horner syndrome.3,4 Exploring anhidrosis and any other skin changes that may appear may help locate the involvement of the cervical sympathetic chain.5 We present the case of a patient with Horner syndrome and an infrequent though characteristic change in face colouration that alarmed the patient.
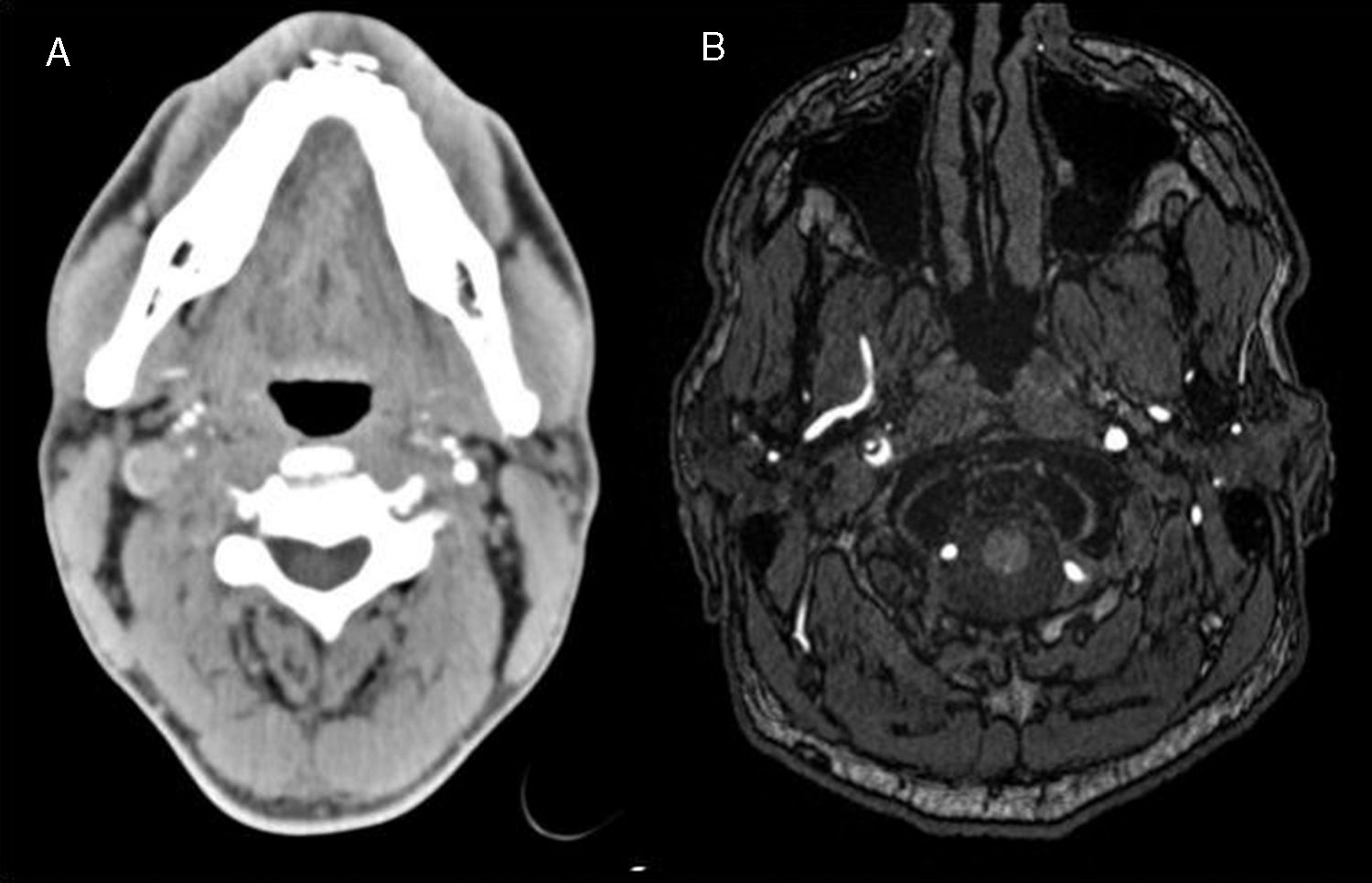
This 44-year-old man was a triathlete and reported no allergies to medications and no alcohol, smoking, or drug habits. During the swimming leg of a triathlon, the patient received a blow to the right side of the neck and began to feel pain in the right side of the face and neck. Pain persisted after finishing the swimming leg, and was associated with right-sided ptosis and blurred vision; the patient went to hospital 24hours later. The examination revealed right miosis with preserved pupillary light reflex and right ptosis; the patient reported diplopia with extreme right gaze positions. The neurological and general examination revealed no other relevant findings. A blood analysis detected no remarkable alterations. A brain CT scan and a CT angiography study showed no parenchymal alterations and revealed reduced contrast flow in the extracranial section of the right internal carotid artery (after the bifurcation), with occlusion of the arterial lumen (Fig. 1A). Brain MRI and MRI angiography findings suggested right internal carotid artery dissection at the cervical level, associated with a lack of blood flow from the carotid canal to the venous sinus on time-of-flight sequences (Fig. 1B), and punctiform cortical–subcortical ischaemic lesions in the watershed territory of the right anterior and middle cerebral arteries. The patient was diagnosed with Horner syndrome and headache secondary to traumatic right internal carotid artery dissection, and was discharged with oral anticoagulants and conventional analgesics. After several weeks of rest, and resuming work and daily activities, including exercise, he became concerned by his symptoms and sent us a photograph of himself (Fig. 2). He presented changes in facial skin colouration after exercise: the left side of his face was flushed and sweaty, whereas the right side was pale, showing anhidrosis. A 3-month follow-up examination revealed clinical improvements, with mild right ptosis and miosis persisting. Additional MRI and MRI angiography studies revealed no alterations; acenocoumarol was switched for acetylsalicylic acid.
(A) CT angiography showing reduced blood flow in the right internal carotid artery at the level of the cervical spine. (B) MRI angiography (time-of-flight sequence) showing reduced blood flow in the same artery (this sequence was taken at a higher level than the CT angiography sequence) and a false lumen in the medial region.
Horner syndrome is caused by disruption of sympathetic nervous system fibres. The first-order neuron emerges from the hypothalamus and descends through the brainstem to the spinal cord, where it synapses in the Clarke column, at the C8-T1 level. The second-order neuron exits the spinal cord via the T1 nerve root, ascending through the cervical chain ganglia and synapsing in the superior cervical ganglion (C1-C2). The third-order (postganglionic) neuron travels along the carotid artery to the iris dilator muscle.5 First-order neuron lesions affect sweating on the same side of the body, whereas second-order neuron lesions cause ipsilateral facial alterations and third-order neuron lesions either do not affect sweating or affect sweating only in the upper part of the face.6 In our patient, compression of the cervical sympathetic plexus was located at the level of the internal carotid artery, immediately below the superior cervical ganglion. Insufficient evidence is available to confirm that anticoagulants are more effective than antiplatelets.7,8 However, early treatment is essential to prevent ischaemic brain lesions; associated mortality may reach 20%. Around 30% of patients are left with permanent neurological sequelae.9 In our patient, the acute episode was managed with anticoagulants due to MRI evidence of atheroembolic lesions; once symptoms had resolved, the patient received conventional antiplatelets.
We present the case of a patient with rare though characteristic imaging signs of cervical sympathetic chain involvement. The association between anhidrosis or hypohidrosis and skin colouration changes is a typical sign of the disease that helps locate the lesions to the cervical sympathetic chain.
We wish to express our sincere thanks to our patient for consenting to the publication of his case and images; this study would have not been possible without his cooperation.