Rheumatoid arthritis is a chronic, inflammatory, systemic disease that mainly affects ligaments, joints, and ultimately bone. Its pathophysiology involves genetic, autoimmune, and environmental factors. The condition is caused by synovial inflammation, leading to destruction of the joints.1 However, the condition has also been associated with cardiovascular, pulmonary, digestive, haematological, and more rarely neurological manifestations.2 Rheumatoid arthritis is one of the most frequent rheumatic disorders worldwide, with an estimated prevalence of 0.5%-1% in the adult population.3,4
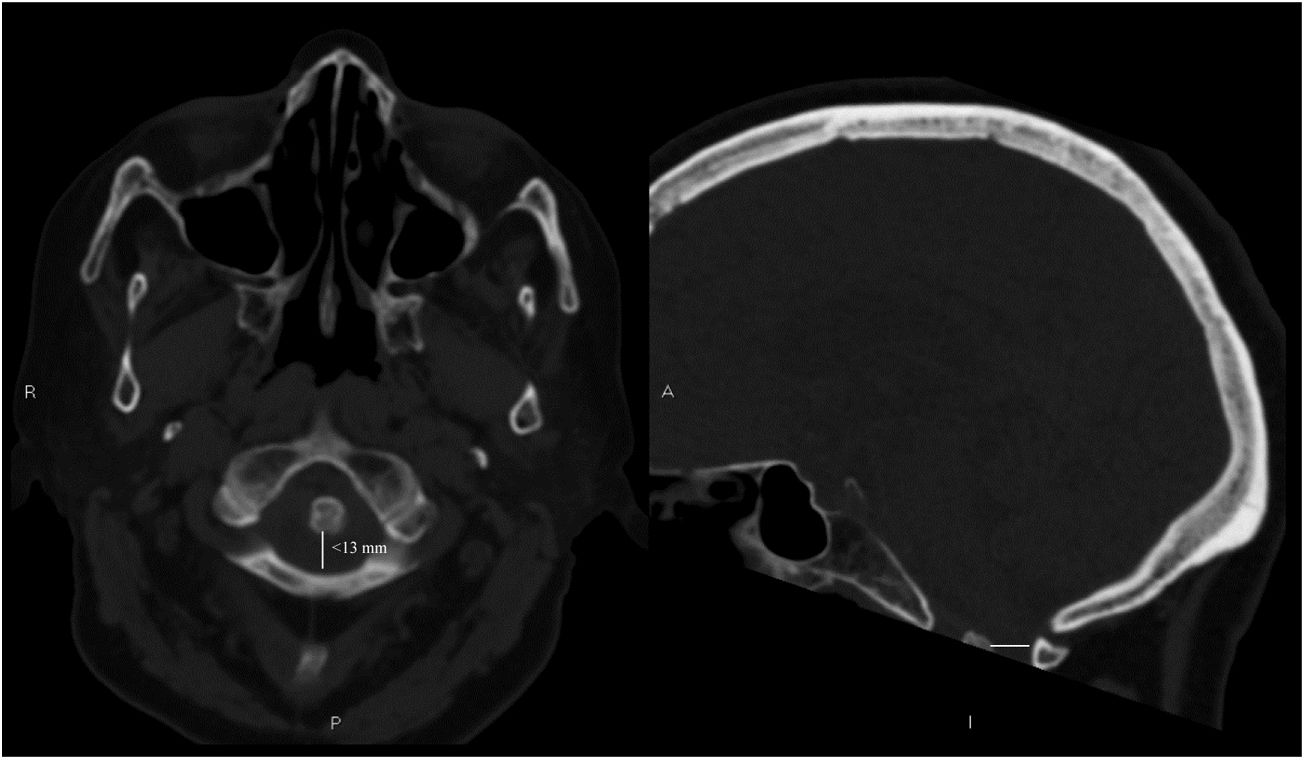
We present the case of a 76-year-old woman with no known vascular risk factors, under treatment with methotrexate and folic acid due to chronic rheumatoid arthritis. She visited our hospital's emergency department due to inability to walk as a result of loss of muscle strength in the right leg of less than 24 hours’ progression. She presented no neck pain and reported no history of trauma. The examination revealed paresis in the proximal part of the right leg (3/5), mild hyperreflexia of the right limbs, and extensor plantar reflex in the right foot, associated with impaired proprioceptive sensitivity (arthrokinetic and positional) in the right leg. Examination of cranial nerves and tactile and pain sensitivity revealed no alterations. An emergency blood analysis including a biochemistry study and a complete blood count yielded normal results, and a head CT scan revealed no alterations in the brain parenchyma. However, it did show incipient compression of the medulla oblongata by the dens of the axis, with a posterior atlantodental interval <13mm (radiological measurement between the posterior surface of the odontoid process and the posterior arch of the atlas,5 with normal values being >14mm) (Fig. 1).
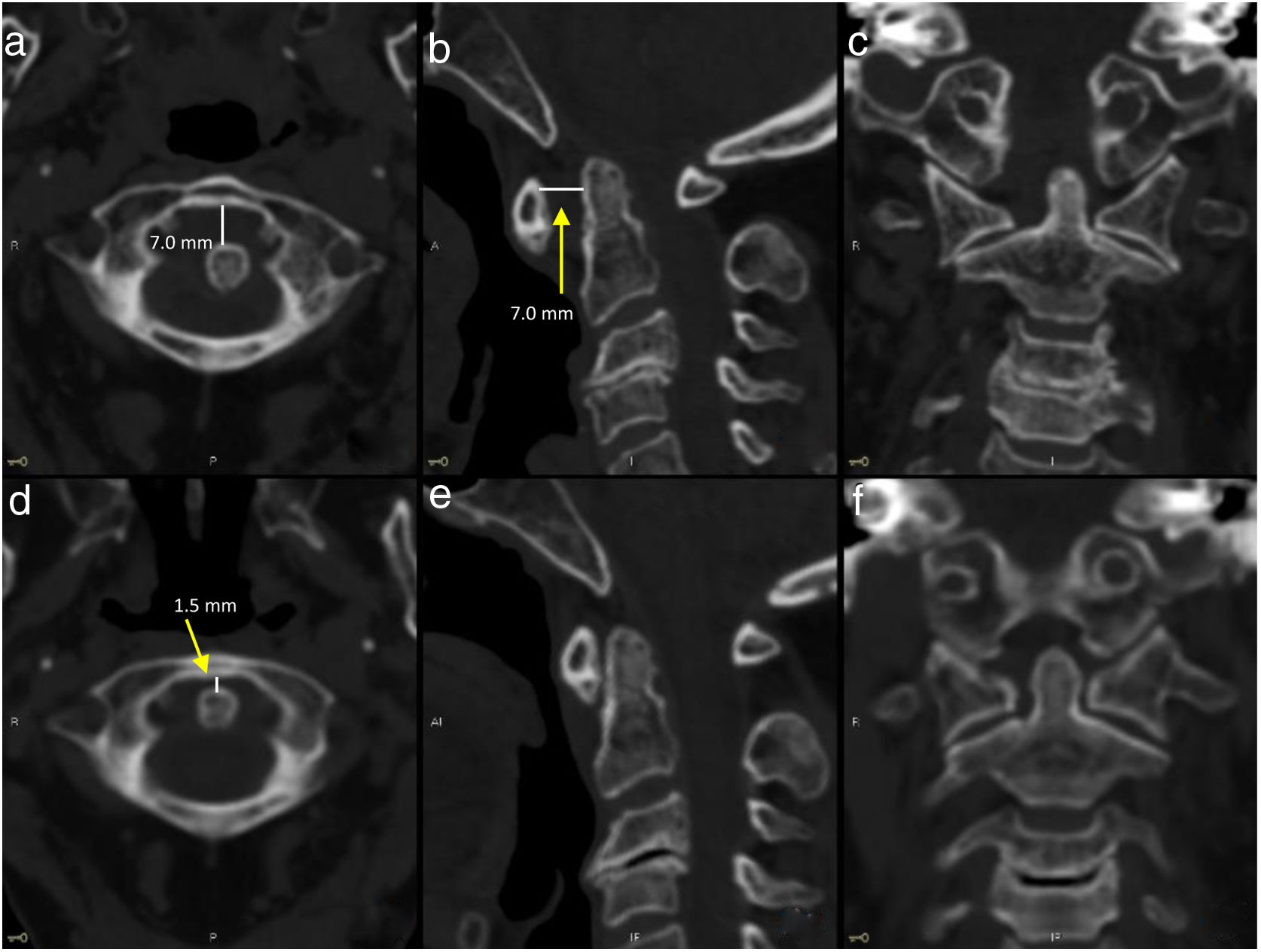
Clinical findings were anatomically correlated with radiological findings, and compatible with incomplete right hemimedullary syndrome. In view of the patient's history and symptoms, we decided to perform a neck CT scan (Fig. 2), which revealed atlantoaxial subluxation and an anterior atlantodental interval of 7mm (distance between the anterior surface of the odontoid process and the anterior arch of the atlas5; normal value, <3mm). The patient was instructed to wear a Halo vest to immobilise the cervical spine, and subsequently underwent surgery for screw fixation. At discharge, motor deficits in the right leg persisted.
Non-contrast neck CT images taken before (a–c) and after (d–f) cervical spine immobilisation with a Halo vest. The neuroimaging study performed before the intervention revealed an abnormal anterior atlantodental interval (>3mm, a and b), which was subsequently corrected (d and e).
Cervical myelopathy secondary to atlantoaxial subluxation is a known complication in patients with rheumatoid arthritis, and is associated with poorer prognosis and greater mortality rates.6 Involvement of this large joint, which is occasionally asymptomatic, is described in up to 40% of patients with rheumatoid arthritis, and is one of the most frequent alterations after small joint erosion.7 The risk of developing cervical instability has been associated with a number of factors, including long disease progression, long-term corticosteroid treatment, involvement of other large joints, and high degree of inflammatory activity of the disease (elevated C-reactive protein levels or erythrocyte sedimentation rate).7,8 The development of myelopathy in the context of rheumatoid arthritis is frequently associated with neck pain, occipital headache, Lhermite sign, tinnitus, otalgia, and crepitation with neck movement.7
We present the case of a patient with rheumatoid arthritis and atlantoaxial subluxation manifesting as acute hemimedullary syndrome, without neck pain or history of trauma. Although several cases have been reported of cervical myelopathy associated with Brown-Sequard syndrome,9 the interest of our case lies in the incomplete, atypical presentation of the syndrome (acute presentation without the prodromal symptoms listed above), which may have delayed diagnosis. Emergency neuroimaging (atlantodental interval in axial CT images) may be extremely useful for early diagnosis in the event of acute presentation in patients with no history of trauma, or not presenting other symptoms suggestive of spinal cord compression.
Atlantoaxial subluxation is a known, alarming complication of rheumatoid arthritis. However, cervical instability may be silent in some patients and can remain undiagnosed for years. Neuroimaging studies may help in the early diagnosis of atypical cases, enabling early surgical treatment.
FundingDaniel Macías-García has received funding as part of the “Río Hortega” training programme (CM18/00142; Institute of Health Carlos III). The remaining authors have received no funding for this study.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Macías-García D, Jurado Serrano J, Parada Blazquez MJ, Moniche F. Paresia aguda de miembro inferior en paciente con artritis reumatoide: hallazgos en la neuroimagen de urgencia. Neurología. 2020;35:593–595.