Stroke has a complex aetiopathogenesis influenced by numerous risk factors. There is growing interest in the study of the pathophysiological changes associated with stress and their potential relationship with cerebrovascular disease. The purpose of this paper is to assess the strength of association between exposure to stress and stroke.
MethodsWe conducted a case–control study (1:1) to compare exposure to stress in a group of patients with a history of a first transient ischaemic attack (TIA) or minor stroke and in a control group. Participants were asked a subjective question about their perception of stress in the previous months and completed the standardised Effort-Reward Imbalance (ERI) questionnaire. Logistic regression models were used for data analysis.
ResultsThe study included data on 50 cases and 50 controls. There were no significant differences in demographic variables and economic, social, and employment status between cases and controls. Fifty percent of the cases reported moderate to severe stress, compared to 30% of controls (OR: 2.33; 95% CI: 1.02-5.30; P=.041). ERI questionnaire results found that greater effort at work (OR: 1.48; 95% CI: 1.19-1.83) and greater commitment is associated with stroke (OR: 1.34; 95% CI: 1.17-1.54), while higher reward constitutes a protective factor against the disease (OR: 0.71; 95% CI: 0.61-0.82).
ConclusionsThere is a strong association between self-perceived psychological stress and TIA. The imbalance between effort and reward at work is also clearly related to TIA.
El ictus tiene una etiopatogenia compleja en la que influyen un gran número de factores de riesgo. Existe un creciente interés por el estudio de los cambios fisiopatológicos que conlleva el estrés y su posible relación con la enfermedad cerebrovascular. El propósito de este trabajo es valorar la fuerza de asociación entre la exposición al estrés y el ictus.
MétodoRealizamos un estudio de casos y controles (1:1), comparando la exposición al estrés en un grupo de pacientes con antecedentes de un primer ataque isquémico transitorio o ictus minor, frente a un grupo control. Se realizó una pregunta subjetiva sobre la percepción de estrés en los últimos meses y se aplicó el cuestionario estandarizado Effort-Reward Imbalance (ERI). Para el análisis utilizamos modelos de regresión logística.
ResultadosIncluimos 50 casos y 50 controles. No hubo diferencias significativas en las variables demográficas entre casos y controles, ni en nivel económico, situación social o laboral. El 50% de los casos refería situación de estrés moderada o grave frente al 30% de controles (OR: 2,33; IC95%: 1,02-5,30; p=0,041). Cuestionario ERI: se observa que un mayor esfuerzo en el trabajo (OR: 1,48; IC95%: 1,19-1,83) y un mayor compromiso frente a una menor implicación laboral se asocia con el ictus (OR: 1,34; IC95%: 1,17-1,54); mientras que una mayor recompensa laboral tiene un factor protector (OR: 0,71; IC95%: 0,61-0,82).
ConclusionesExiste una fuerte asociación entre la percepción del estrés y el ataque isquémico transitorio. El desequilibrio entre el esfuerzo y la recompensa laboral también se relaciona claramente con el ataque isquémico transitorio.
The aetiopathogenesis of stroke is complex and heterogeneous. This is reflected in the wide range of stroke risk factors identified in epidemiological studies.1,2 Traditional vascular risk factors do not fully explain cerebrovascular disease in all cases; other lines of research have suggested psychosocial stress as a potential risk factor.3 There is growing interest in the pathophysiological changes brought on by stress and their possible role in the development of disease.4 Evidence has been found of an association between stress and ischaemic heart disease, and psychological stress is considered a new cardiovascular risk factor. Evidence of the association between stress and cerebrovascular disease is less conclusive, however.5,6
Stress is defined as a process in which environmental demands compromise or exceed an organism's adaptive capacity, resulting in psychological and biological changes. This alters the body's homeostasis, triggering the activation of a series of genetically determined and environmentally modulated circuits. The purpose of these changes is to make the organism respond to the stressor as adaptively as possible. The physiological stress response is very complex, and involves both the nervous and the endocrine system.6,7
Stress is the second most frequent work-related health problem in the European Union, after musculoskeletal disorders. According to the Sixth Spanish National Working Conditions Survey (2005), 27.9% of workers reporting work-related health problems presented symptoms of stress.7
Several models have been used to identify work-related factors of psychosocial stress; one of these is the “effort-reward imbalance” model, developed by Siegrist.8 According to this model, highly demanding tasks associated with low rewards cause negative stress, which increases the risk of cardiovascular diseases and negatively affects mental health.9 The “effort-reward imbalance” model enables reasonably accurate estimation of an individual's work-related stress, since it evaluates both intrinsic and extrinsic variables affecting patients’ working life. Extrinsic variables include the effort and reward of the work, whereas intrinsic variables involve commitment and stress coping strategies.8
The aim of this study was to evaluate the strength of association between stroke and exposure to stress, and to determine whether the type of work (manual vs non-manual labour) has a significant impact on stroke risk.
MethodsOur observational case–control study analysed exposure to work-related stress in a group of patients with history of transient ischaemic attack (TIA) or minor stroke (patients) against individuals with no history of stroke (controls).
All members of the target population were active workers younger than 70 years old with a history of cerebrovascular disease. Controls were gathered from the same setting and had no history of cerebrovascular disease.
Inclusion criteria for patients were as follows (patients had to meet one of the 2 descriptions): (1) experiencing an episode of neurological impairment lasting less than 1hour, regardless of presence of signs of acute infarction on DWI; or (2) minor stroke, referring to patients not eligible for fibrinolysis or endovascular treatment (baseline NIHSS score≤3). All patients underwent MRI studies.
We gathered the following information from our sample: sociodemographic data (age, sex, place of residence, education level, income level); employment status (current status and type of work); personal history of depression or family history of stroke, dementia, or heart disease; and vascular risk factors (arterial hypertension, dyslipidaemia, diabetes, atrial fibrillation, ischaemic heart disease, tobacco, or alcohol use). We measured participants’ blood pressure and calculated body mass index. The Gijon's social-familial evaluation scale was used to evaluate social risk. We also gathered subjective data, asking participants whether they had experienced stress in the past few months and their perceived stress level.
Stress was measured with the standardised Effort-Reward Imbalance (ERI) questionnaire. The first part of the questionnaire evaluates self-perceived work-related stress and comprises 2 scales. The first scale evaluates the extrinsic effort an individual's work demands (effort scale), whereas the second evaluates rewards by analysing 3 factors: job promotion, esteem, and job security (reward scale). Combining both scales gives the effort-reward (ER) ratio, which differentiates between high-risk (> 1) and low-risk individuals (≤ 1). The second part assesses intrinsic components of stress, such as work commitment and the worker's positive or negative feelings towards his/her job (overcommitment scale).
Data were gathered with a structured interview; patients completed the interview during admission, whereas controls were interviewed at a time convenient to them.
We performed a descriptive analysis of variables using measures of central tendency and dispersion (mean [standard deviation; SD]) for quantitative variables, and frequencies for qualitative variables. The chi-square test was used to compare the distribution of qualitative variables between patients and controls. The t test for independent samples was used to analyse quantitative variables. We analysed the strength of association between stroke and exposure to stress using logistic regression analysis of each scale of the ERI questionnaire and the ER ratio. We also analysed the correlation between self-perceived stress and ERI scores. The SPSS statistical software, version 23.0 (IBM, Ehningen, Germany), was used for statistical analysis.
All participants were informed verbally and in writing about the purpose of the study and what was expected from them; individuals willing to participate signed informed consent forms. The confidentiality of personal data was guaranteed.
ResultsThe patient group included 50 consecutive patients who presented a first TIA or minor stroke in 2016 and were admitted to our hospital's stroke unit. The group included 35 men (70%) and 15 women (30%). Mean age (SD) was 57.7 (8.02) years. The control group included 50 individuals with no known cerebrovascular disease, and comprised 27 men (54%) and 23 women (46%) with a mean age of 56.8 years.6,8
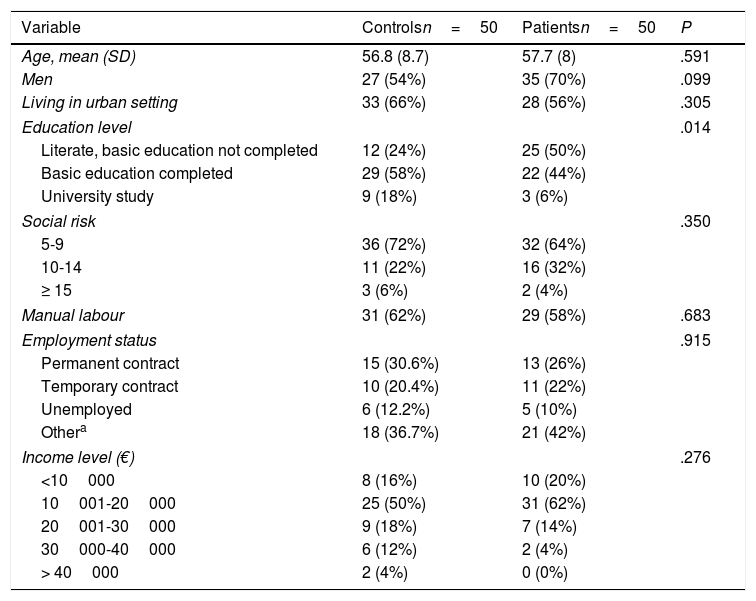
Twenty-nine patients (58%) and 31 controls (62%) had manual jobs (P=.683); the remaining participants performed non-manual work. No significant differences in employment status were observed between patients and controls. In the patient group, 13 (26%) had a permanent contract, 11 (22%) had a temporary contract, 5 (10%) were unemployed, and 21 (42%) had another employment status. In the control group, 15 (30.6%) had a permanent contract, 10 (20.4%) had a temporary contract, 6 (12.2%) were unemployed, and 18 (36.7%) had another employment status. No significant inter-group differences were observed in terms of place of residence (P=.305), social risk (P=.506), or income level (P=.276); however, significant differences were observed in education level (P=.014). Table 1 summarises the sociodemographic characteristics of patients and controls.
Sociodemographic characteristics of patients and controls.
| Variable | Controlsn=50 | Patientsn=50 | P |
|---|---|---|---|
| Age, mean (SD) | 56.8 (8.7) | 57.7 (8) | .591 |
| Men | 27 (54%) | 35 (70%) | .099 |
| Living in urban setting | 33 (66%) | 28 (56%) | .305 |
| Education level | .014 | ||
| Literate, basic education not completed | 12 (24%) | 25 (50%) | |
| Basic education completed | 29 (58%) | 22 (44%) | |
| University study | 9 (18%) | 3 (6%) | |
| Social risk | .350 | ||
| 5-9 | 36 (72%) | 32 (64%) | |
| 10-14 | 11 (22%) | 16 (32%) | |
| ≥ 15 | 3 (6%) | 2 (4%) | |
| Manual labour | 31 (62%) | 29 (58%) | .683 |
| Employment status | .915 | ||
| Permanent contract | 15 (30.6%) | 13 (26%) | |
| Temporary contract | 10 (20.4%) | 11 (22%) | |
| Unemployed | 6 (12.2%) | 5 (10%) | |
| Othera | 18 (36.7%) | 21 (42%) | |
| Income level (€) | .276 | ||
| <10000 | 8 (16%) | 10 (20%) | |
| 10001-20000 | 25 (50%) | 31 (62%) | |
| 20001-30000 | 9 (18%) | 7 (14%) | |
| 30000-40000 | 6 (12%) | 2 (4%) | |
| > 40000 | 2 (4%) | 0 (0%) | |
SD: standard deviation.
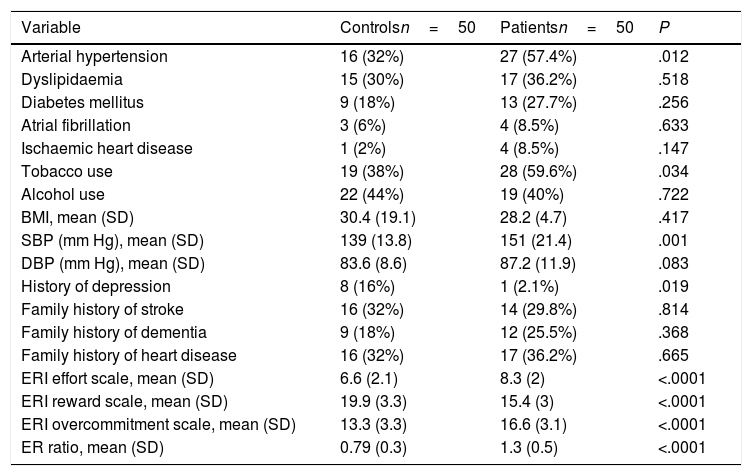
Table 2 lists the risk factors and personal and family history of the patients included in our study. The only variables showing significant inter-group differences were arterial hypertension and tobacco use. Mean systolic/diastolic blood pressure was 151/87mm Hg in patients and 139/84mm Hg in controls (P=.001 and P=.083).
Risk factors, medical history, and ERI questionnaire results in our sample.
| Variable | Controlsn=50 | Patientsn=50 | P |
|---|---|---|---|
| Arterial hypertension | 16 (32%) | 27 (57.4%) | .012 |
| Dyslipidaemia | 15 (30%) | 17 (36.2%) | .518 |
| Diabetes mellitus | 9 (18%) | 13 (27.7%) | .256 |
| Atrial fibrillation | 3 (6%) | 4 (8.5%) | .633 |
| Ischaemic heart disease | 1 (2%) | 4 (8.5%) | .147 |
| Tobacco use | 19 (38%) | 28 (59.6%) | .034 |
| Alcohol use | 22 (44%) | 19 (40%) | .722 |
| BMI, mean (SD) | 30.4 (19.1) | 28.2 (4.7) | .417 |
| SBP (mm Hg), mean (SD) | 139 (13.8) | 151 (21.4) | .001 |
| DBP (mm Hg), mean (SD) | 83.6 (8.6) | 87.2 (11.9) | .083 |
| History of depression | 8 (16%) | 1 (2.1%) | .019 |
| Family history of stroke | 16 (32%) | 14 (29.8%) | .814 |
| Family history of dementia | 9 (18%) | 12 (25.5%) | .368 |
| Family history of heart disease | 16 (32%) | 17 (36.2%) | .665 |
| ERI effort scale, mean (SD) | 6.6 (2.1) | 8.3 (2) | <.0001 |
| ERI reward scale, mean (SD) | 19.9 (3.3) | 15.4 (3) | <.0001 |
| ERI overcommitment scale, mean (SD) | 13.3 (3.3) | 16.6 (3.1) | <.0001 |
| ER ratio, mean (SD) | 0.79 (0.3) | 1.3 (0.5) | <.0001 |
BMI: body mass index; DBP: diastolic blood pressure; ER: effort-reward; ERI: Effort-Reward Imbalance questionnaire; SBP: systolic blood pressure; SD: standard deviation.
Cerebrovascular disease presented with motor symptoms in 30 patients (60%), with language impairment in 17 (34%), and with other symptoms in 12 (24%). All patients underwent MRI studies; DWI sequences revealed lesions in 41 patients (82%). Aetiology was atherothrombotic in 9 (18%), cardioembolic in 3 (6%), lacunar in 12 (24%), undetermined in 23 (46%), and another cause in 3 (6%).
Eighty-six percent of patients reported self-perceived stress, which was moderate to severe in 25 (50%); 70% of controls reported stress, which was moderate to severe in 15 (30%). Self-perceived stress was found to be associated with TIA, with an OR of 2.33 (95% CI, 1.02-5.30; P=.04).
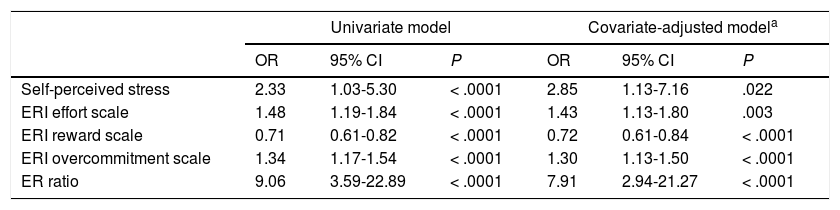
Stroke was found to be associated with greater effort (effort scale: OR=1.48; 95% CI, 1.19-1.83) and overcommitment at work (overcommitment scale: OR=1.34; 95% CI, 1.17-1.54), whereas greater reward was found to have a protective effect (reward scale: OR=0.71; 95% CI, 0.61-0.82). The ER ratio was clearly associated with cerebrovascular disease in our sample (OR=9.1; 95% CI, 3.59-22.89). ER ratio and self-perceived stress continued to be strongly associated with cerebrovascular disease after the 3 ERI scales were adjusted for sex, education level, and presence of arterial hypertension. Table 3 shows the results of the univariate and covariate-adjusted regression models.
Strength of association between stress and TIA or minor stroke.
| Univariate model | Covariate-adjusted modela | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | |
| Self-perceived stress | 2.33 | 1.03-5.30 | < .0001 | 2.85 | 1.13-7.16 | .022 |
| ERI effort scale | 1.48 | 1.19-1.84 | < .0001 | 1.43 | 1.13-1.80 | .003 |
| ERI reward scale | 0.71 | 0.61-0.82 | < .0001 | 0.72 | 0.61-0.84 | < .0001 |
| ERI overcommitment scale | 1.34 | 1.17-1.54 | < .0001 | 1.30 | 1.13-1.50 | < .0001 |
| ER ratio | 9.06 | 3.59-22.89 | < .0001 | 7.91 | 2.94-21.27 | < .0001 |
95% CI: 95% confidence interval; ER: effort-reward; ERI: Effort-Reward Imbalance questionnaire; OR: odds ratio; P: significance level; TIA: transient ischaemic attack.
We found no association between type of work and risk of TIA (P=.683), or between type of work and ERI questionnaire results (effort scale [P=.921], reward scale [P=.900], overcommitment scale [P=.08], or ER ratio [P=.710]).
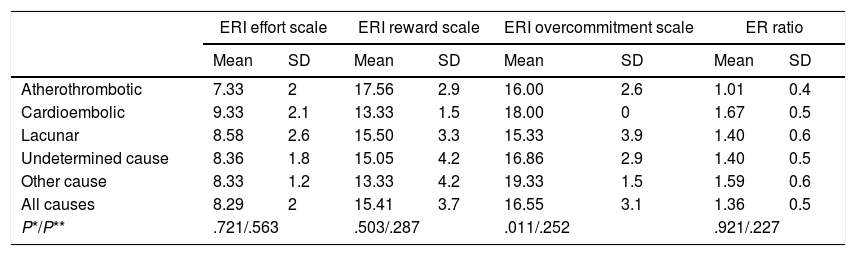
No correlation was observed between aetiology and level of stress (Table 4).
Association between stress and aetiology of TIA or minor stroke in our patients (n=50).
| ERI effort scale | ERI reward scale | ERI overcommitment scale | ER ratio | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Atherothrombotic | 7.33 | 2 | 17.56 | 2.9 | 16.00 | 2.6 | 1.01 | 0.4 |
| Cardioembolic | 9.33 | 2.1 | 13.33 | 1.5 | 18.00 | 0 | 1.67 | 0.5 |
| Lacunar | 8.58 | 2.6 | 15.50 | 3.3 | 15.33 | 3.9 | 1.40 | 0.6 |
| Undetermined cause | 8.36 | 1.8 | 15.05 | 4.2 | 16.86 | 2.9 | 1.40 | 0.5 |
| Other cause | 8.33 | 1.2 | 13.33 | 4.2 | 19.33 | 1.5 | 1.59 | 0.6 |
| All causes | 8.29 | 2 | 15.41 | 3.7 | 16.55 | 3.1 | 1.36 | 0.5 |
| P*/P** | .721/.563 | .503/.287 | .011/.252 | .921/.227 | ||||
However, we did find a correlation between self-perceived stress level and ERI scores (Pearson correlation coefficient: effort scale, 0.349 [P<.0001]; reward scale, −0.216 [P=.035]; overcommitment scale, 0.223 [P=.029]; and ER ratio, 0.315 [P=.002]).
DiscussionThe study of factors involved in stroke pathogenesis continues to be relevant, since the best known risk factors cannot fully explain all cases of stroke or the upward trend in cerebrovascular disease incidence in young adults.10,11 Our results suggest a strong association between exposure to stress and risk of TIA.
The physiological stress response is very complex and involves the nervous system (the autonomic nervous system, particularly the sympathetic nervous system, and the hypothalamus) and the endocrine system (pituitary and adrenal glands). The hypothalamus and the pituitary gland are anatomically and structurally connected, acting as a bridge between the nervous and endocrine systems. They also play a role in immune response and behaviour. Stressors activate the sympathetic nervous system, stimulating catecholamine release from the adrenal medulla and adrenergic terminals. The hypothalamic–pituitary–adrenal axis is also activated: the hypothalamus secretes hormones, mainly corticotropin-releasing hormone, which in turn stimulates the anterior pituitary gland. The latter releases adrenocorticotropic hormone, resulting in peripheral release of glucocorticoids (cortisol) and mineralocorticoids (aldosterone). This hormonal response triggers a series of changes: increases in blood levels of glucose, leukocytes, erythrocytes, and platelets; increased heart rate, force of contraction of cardiac muscles, and respiratory rate; vasodilation of coronary arteries and blood vessels of skeletal muscles; and vasoconstriction of blood vessels in other organs.7,12
Cardiovascular disease is currently thought to be greatly influenced by psychosocial factors, including lifestyle and long-term exposure to stress; these are both aetiopathogenic and prognostic factors.4,5,13 Numerous experimental studies have evaluated the association between chronic stress and cardiovascular disease, reporting exacerbation of coronary artery disease due to increased autonomic nervous system activity, with endothelial dysfunction and necrosis.4,14 Research has shown that stress may trigger ischaemic heart disease and arrhythmia and promote platelet aggregation, increase blood viscosity, and cause vasoconstriction of coronary arteries.15
Some studies suggest that a stressful environment increases morbidity and mortality associated with coronary artery disease, mainly as a result of arterial hypertension.13 In a study published in 2003 by Kario et al.,16 exposure to a stressor, the Hanshin-Awaji earthquake, was found to increase systolic and diastolic blood pressure by 14mm Hg and 6mm Hg, respectively, in 134 elderly patients with arterial hypertension living close to the epicentre.16 In a study by Vrijkotte et al.,17 individuals working in a highly demanding environment and with low reward showed higher heart rates and blood pressure readings and lower vagal tone than peers with better effort-reward balance.
There is a clear association between stress and arterial hypertension; the latter, in turn, is regarded as the main risk factor for stroke. Individuals exposed to chronic stress are more likely to develop arterial hypertension at early ages and therefore have a higher risk of stroke.13 Research has shown that individuals with greater cardiovascular reactivity have a higher risk of arterial hypertension, atherosclerosis, and ischaemic stroke.18 In 2007, Surtees et al.19 reported a 25% decrease in the risk of stroke in individuals with good stress coping strategies. A prospective study published in 2001 analysed the association between cardiovascular response to stress and stroke incidence in men, and found that individuals displaying increases in systolic blood pressure of over 20mm Hg had a 72% greater risk of stroke.20 We may expect to observe a stronger association between stress and lacunar stroke, given that the latter is the stroke subtype most frequently associated with arterial hypertension21; however, we found no significant differences between aetiologies.
Stress is not associated only with arterial hypertension; rather, it has an impact on other stroke risk factors, and is involved in the pathogenesis of atherosclerosis.4,14,15 In a study published in 2006, Chandola et al.22 evaluated work-related stress in a sample of civil servants, concluding that work-related stress was associated with a twofold increase in the risk of metabolic syndrome, as compared to workers without stress. A review article by Martínez Plaza7 explains how exposure to stressors induces hypercoagulability due to increases in levels of fibrinogen, factor VII, interleukin 6-induced acute phase proteins, homocystein, and leptin. These stress-induced changes act at least as markers of stroke risk.
According to our results, people with chronic stress are at a greater risk of TIA. This is consistent with the results of a study on the association between the psychosocial work environment and risk of stroke; the authors, who also used the ERI questionnaire, concluded that stress and exposure to conflict at work are independent risk factors of stroke.23
Hamer et al.24 prospectively studied a series of patients with no prior history of cardiovascular disease, evaluating psychosocial stress with the General Health Questionnaire at different times over an 8-year follow-up period. The authors report a higher risk of death due to ischaemic heart disease and stroke in patients with psychological distress. Another study using the General Health Questionnaire concluded that stress is a predictor of ischaemic stroke: patients with stress were found to be 1.45 times more likely to have a stroke.25 A more recent study concluded that the risk of stroke is 18% higher in people with psychosocial stress; the researchers also observed a stronger association between stress and risk of stroke in patients with haemorrhagic stroke than in those with ischaemic stroke.26
The ERI questionnaire has also been used in studies analysing the association between exposure to stress and acute myocardial infarction and arterial hypertension.27,28 In a cohort study conducted in Canada, high ERI scores were found to be correlated with higher blood pressure and poorer response to antihypertensive treatment; the authors concluded that reducing work-related stress may improve blood pressure and help prevent associated complications.27
Our study has certain limitations, including the small size of our sample and its case–control design: strictly speaking, the results of this type of studies do not imply causality. Information bias may have occurred in our study, since exposure to stress in our patients was evaluated after they had developed cerebrovascular disease. However, given the homogeneity and representativeness of our sample, we believe that the estimated risk is similar to the actual risk, which would at least enable an advance in this line of research. Our results can only be extrapolated to patients with TIA or minor stroke.
In conclusion, there is considerable biological and epidemiological evidence supporting the hypothesis that psychosocial stress is a cerebrovascular risk factor, given the association between stroke and exposure to stress. Patients’ self-perceived stress should be considered during clinical evaluations. Further research should aim to determine the intrinsic mechanisms by which psychosocial stress contributes to cerebrovascular disease and to assess the potential benefits of workplace stress prevention programmes in reducing stroke risk.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Ramírez-Moreno JM, Muñoz Vega P, Espada S, Bartolomé Alberca S, Aguirre J, Peral D. La autopercepción del estrés psicológico se asocia con el ataque isquémico transitorio e ictus minor. Un estudio de casos y controles. Neurología. 2020;35:556–562.