Moyamoya disease (MD) is a progressive, occlusive disease of the arteries of the anterior cerebral circulation that may cause ischaemia or haemorrhage. Patient management aims to prevent new cerebrovascular events through surgical revascularisation and/or pharmacological treatment.
Materials and methodsWe studied a series of 17 patients with MD (n = 14) or moyamoya syndrome (MS; n = 3), who were evaluated between January 1989 and December 2016; 11 patients were women and 6 were men. Thirteen patients had definitive MD (76%), one had unilateral MD (5.2%), and 3 had MS (18%). The condition manifested as intraparenchymal haemorrhage (in 35.2% of patients), brain ischaemia (29.4%), subarachnoid haemorrhage (17.6%), seizures (11.7%), and headache with no associated haemorrhage (1 patient).
ResultsTen patients (58.8%) underwent revascularisation and 7 (41.2%) received pharmacological treatment. All patients were evaluated with the modified Rankin Scale (mRs) at admission and at the last consultation; mRs scores were significantly lower in the group undergoing surgery (P < .04). During follow-up, none of the patients undergoing revascularisation experienced recurrences, whereas 2 patients receiving pharmacological treatment did experience a new vascular event (one ischaemic and one haemorrhagic) (P < .05). No significant differences were observed between the treatment outcomes of different revascularisation techniques.
ConclusionsAlthough our population has different demographic characteristics from those of other non-Asian populations, ours is the largest published series of Hispanic individuals with MD. Our results support the use of revascularisation procedures to improve these patients’ neurological status and to prevent new cerebrovascular events.
La enfermedad Moyamoya (EM) es una arteriopatía oclusiva y progresiva de la circulación cerebral anterior, que puede producir eventos isquémicos o hemorrágicos. El objetivo terapéutico es la prevención de nuevos eventos a través de tratamiento médico o cirugía de revascularización.
MétodosSe estudiaron 17 pacientes con EM y síndrome Moyamoya (SM), atendidos de enero de 1989 a diciembre del 2016. Trece pacientes tenían EM definitiva (76%), 1 paciente EM unilateral (5.2%) y 3 pacientes SM (18%). Once pertenecían al sexo femenino y 6 al masculino. Su forma de presentación fue hemorragia intraparenquimatosa (35.2%), isquemia cerebral (29.4%), hemorragia subaracnoidea (17.6%), crisis convulsivas (11.7%) y 1 paciente debutó con cefalea sin hemorragia.
ResultadosEn 10 pacientes se realizó una cirugía de revascularización (58.8%), y 7 pacientes se manejaron médicamente (41.2%). La valoración neurológica, empleando la escala modificada de Rankin al ingreso y en su última consulta, mostró una diferencia significativa (p < 0.04) a favor del grupo quirúrgico. Ningún paciente del grupo quirúrgico presentó nuevos eventos vasculares, mientras que 2 pacientes del grupo médico desarrollaron uno nuevo (1 isquémico y 1 hemorrágico). En nuestro estudio no hubo una diferencia significativa entre los métodos de revascularización, pero sí en comparación con los pacientes que se trataron médicamente (p < 0.05).
ConclusionesSi bien nuestra población muestra diferencias con otras series reportadas fuera de Asia, esta es la serie reportada más numerosa para una población hispana. Nuestros resultados sugieren que los procedimientos de revascularización son útiles para prevenir nuevos eventos vasculares isquémicos o hemorrágicos.
Moyamoya disease (MD) is an idiopathic arterial occlusive disease characterised by progressive involvement of the anterior cerebral circulation, most commonly manifesting with bilateral stenosis or occlusion of the supraclinoid internal carotid artery (ICA) and its main branches1–5; in exceptional cases, the posterior circulation is affected.6–10 Global incidence is estimated at 0.086 cases per 100 000 population,11 and the disease is very rare in Hispanic populations.
Treatments for the disease aim to increase cerebral blood flow in the affected hemisphere and to reduce the risk of cerebrovascular events. Revascularisation is achieved through the creation of an extracranial-intracranial anastomosis, for example through direct revascularisation from the superficial temporal artery (STA) to the middle cerebral artery (MCA), or indirect revascularisation with encephaloduroarteriosynangiosis (EDAS).10
Although MD is more common in Asian populations, a well-defined phenotype has been identified. The disease predominantly affects women, with the form of presentation depending on age: children develop ischaemia due to inadequate formation of collateral vessels, whereas adults present haemorrhage due to rupture of fragile collateral vessels. Few studies describe the characteristics and treatment of MD in Hispanic populations. This study describes the epidemiological features of MD and the experience of its treatment in Mexican patients older than 18 years of age at a single centre.
Patients and methodsPatientsWe present a series of patients diagnosed with MD (definitive MD, unilateral MD) and moyamoya syndrome and treated between 1989 and 2016 at the Instituto Nacional de Neurología y Neurocirugía Manuel Velasco Suárez in Mexico City. We used the 2012 diagnostic criteria established by the Japanese Ministry of Health, Labour, and Welfare research committee.12 The series includes patients attending the neurosurgery and vascular neurology departments with some ischaemic or haemorrhagic event and diagnosed with MD.
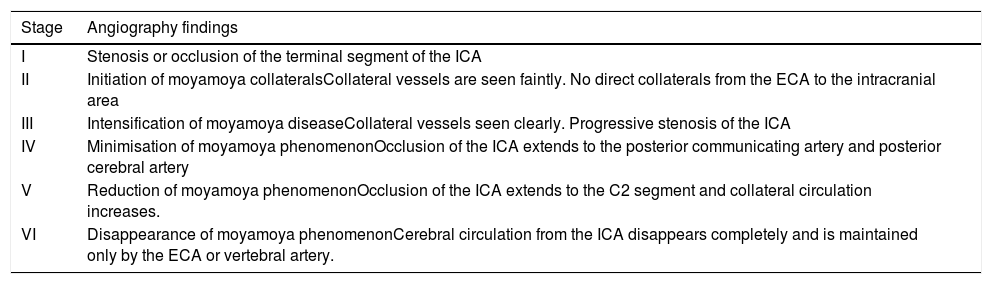
Data were collected on demographic variables, form of presentation (ischaemic or haemorrhagic), neurological status at admission, imaging studies with a description of angiography findings based on the Suzuki staging system for MD,9 indicated medical or surgical treatment (where applicable), and neurological status at discharge (Tables 1 and 2).
Stages of moyamoya disease and description of angiography findings.
| Stage | Angiography findings |
|---|---|
| I | Stenosis or occlusion of the terminal segment of the ICA |
| II | Initiation of moyamoya collateralsCollateral vessels are seen faintly. No direct collaterals from the ECA to the intracranial area |
| III | Intensification of moyamoya diseaseCollateral vessels seen clearly. Progressive stenosis of the ICA |
| IV | Minimisation of moyamoya phenomenonOcclusion of the ICA extends to the posterior communicating artery and posterior cerebral artery |
| V | Reduction of moyamoya phenomenonOcclusion of the ICA extends to the C2 segment and collateral circulation increases. |
| VI | Disappearance of moyamoya phenomenonCerebral circulation from the ICA disappears completely and is maintained only by the ECA or vertebral artery. |
ECA: external carotid artery; ICA: internal carotid artery.
Clinical and sociodemographic variables of patients with moyamoya disease or moyamoya syndrome.
| Variable | |
|---|---|
| Patients studied | 17 |
| Mean age, years (range) | 37 (19−63) |
| Age group, n (%) | |
| 16-20 | 1 (5) |
| 21-30 | 4 (23) |
| 31-40 | 7 (41) |
| 41-50 | 2 (11) |
| 51-60 | 1 (5) |
| 61-70 | 2 (11) |
| Sex, n (%) | |
| Men | 6 (35) |
| Women | 11 (64) |
| Cardiovascular risk factors, n (%) | |
| AHT | 6 (35) |
| DM2 | 5 (29) |
| Smoking | 3 (17) |
| Dyslipidaemia | 2 (11) |
| Stroke, n(%) | |
| Haemorrhagic | 9 (52) |
| Ischaemic | 8 (47) |
| Disease stage (Suzuki staging system), n(%) | |
| I | 2 (11) |
| II | 4 (23) |
| III | 4 (23) |
| IV | 6 (35) |
| V | 0 (0) |
| VI | 1 (5) |
AHT: arterial hypertension; DM2: type 2 diabetes mellitus.
Patients were assessed with the modified Rankin Scale (mRS) every 6 months after the definitive diagnosis was established; patients undergoing surgery were assessed at discharge and monthly for 3 months and then every 6 months if no incidents related to the procedure were recorded. Clinical findings were considered favourable if the patient’s functional status had not worsened with respect to the previous appointment and if imaging studies did not indicate any new cerebrovascular event.
Data analysisFor the analysis of clinical findings, patients were grouped as follows: 1) patients treated surgically; 2) patients treated medically; and 3) patients receiving no treatment.
Sociodemographic variables were analysed with descriptive statistics and by study group. Data were subsequently analysed with the SPSS (version 22 for Windows; IBM) and MATLAB software. Data were tested for normal distribution with the Kolmogorov-Smirnov test. Continuous quantitative variables were analysed with the Wilcoxon and Kruskal-Wallis tests and nominal qualitative variables were studied with the Fisher exact test.
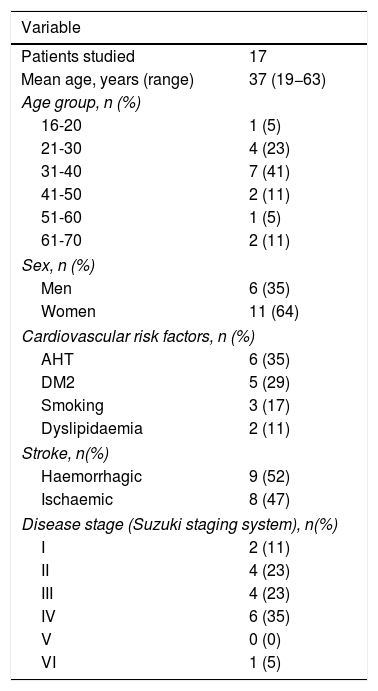
ResultsEpidemiological and clinical dataA total of 17 patients with MD were attended between January 1989 and December 2016. Of these, 13 (76%) were diagnosed with definitive MD, one with unilateral MD (5.2%), and 3 with moyamoya syndrome (18%); the latter syndrome was characterised by angiography findings suggestive of bilateral moyamoya phenomena associated with atherosclerosis of the extracranial ICA in 2 patients (10.4%) and fibromuscular dysplasia in one (5.2%).
Eleven patients (64.7%) were women and 6 (35.5%) were men; therefore, the female-to-male ratio was 1.8:1. The mean age was 37.6 years (range, 18–61). All patients were Mexican; by state, 5 patients were from Mexico City (29.4%), 5 were from Guerrero (29.4%), 2 were from Oaxaca (11.7%), one was from Veracruz (5.8%), one was from Puebla (5.8%), one was from Hidalgo (5.8%), one was from Nuevo León (5.8%), and one was from the State of Mexico (5.8%). No patient had family history of MD.
Of the 17 patients in the series, 7 presented no cardiovascular risk factors (41.1%), 7 presented one risk factor (41.1%), one presented 2 risk factors (5.8%), and 2 presented metabolic syndrome according to the World Health Organization definition (11.7%). The risk factors recorded were arterial hypertension in 6 patients (35.2%), smoking in 5 (29.4%), diabetes mellitus in 3 (17.6%), and dyslipidaemia in 2 (11.7%) (Table 2).
Clinical presentation was intraparenchymal haemorrhage in 6 patients (35.2%), subarachnoid haemorrhage in 3 (17.6%), ischaemia in 5 (29.4%), ischaemia and seizures in 2 (11.7%), and headache without haemorrhage in one (5.8%) (Table 3).
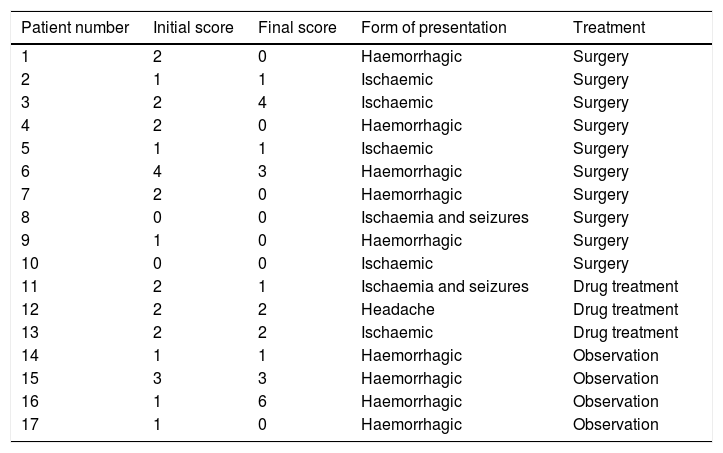
Initial and final modified Rankin Scale scores.
| Patient number | Initial score | Final score | Form of presentation | Treatment |
|---|---|---|---|---|
| 1 | 2 | 0 | Haemorrhagic | Surgery |
| 2 | 1 | 1 | Ischaemic | Surgery |
| 3 | 2 | 4 | Ischaemic | Surgery |
| 4 | 2 | 0 | Haemorrhagic | Surgery |
| 5 | 1 | 1 | Ischaemic | Surgery |
| 6 | 4 | 3 | Haemorrhagic | Surgery |
| 7 | 2 | 0 | Haemorrhagic | Surgery |
| 8 | 0 | 0 | Ischaemia and seizures | Surgery |
| 9 | 1 | 0 | Haemorrhagic | Surgery |
| 10 | 0 | 0 | Ischaemic | Surgery |
| 11 | 2 | 1 | Ischaemia and seizures | Drug treatment |
| 12 | 2 | 2 | Headache | Drug treatment |
| 13 | 2 | 2 | Ischaemic | Drug treatment |
| 14 | 1 | 1 | Haemorrhagic | Observation |
| 15 | 3 | 3 | Haemorrhagic | Observation |
| 16 | 1 | 6 | Haemorrhagic | Observation |
| 17 | 1 | 0 | Haemorrhagic | Observation |
All patients underwent digital subtraction angiography studies, and MD was classified according to the Suzuki staging system (Table 1). The anterior circulation was affected in all cases. Fourteen patients (82.3%) presented stenosis of the terminal segment of both ICAs, extending to the main branches; in 3 (17.6%), involvement of the proximal segment of the MCA was more severe than that of the ICA. In 2 of the patients with haemorrhagic presentation, we found evidence of multiple old lacunar infarcts in the MCA territory bilaterally, with no apparent clinical manifestation prior to the haemorrhagic event.
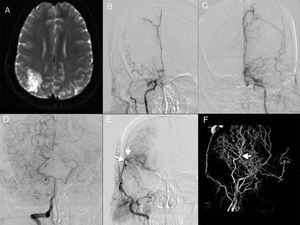
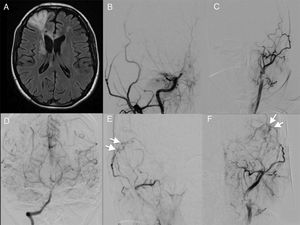
Indication of revascularisation surgeryTen patients (58.8%) underwent surgery, whereas conservative treatment was indicated for 7 (41.17%) (Table 3). Conservative treatment was prescribed to patients in whom the surgical procedure was contraindicated due to their clinical condition, comorbidities, or preferences. Five of the patients undergoing surgery (29.4% of the total sample) presented haemorrhage and the remaining 5 presented ischaemia. Nine patients (52.9%) underwent bilateral revascularisation; a second procedure was contraindicated in one patient (5.8%) due to comorbidities. The first procedure was performed on the symptomatic side. In 8 of the 9 patients undergoing bilateral surgery (47.1% of the total sample), the first procedure performed was direct revascularisation with an STA-MCA bypass, most commonly in segment M3 or M4 (see video in Supplementary Material), and the remaining patient (5.8%) underwent indirect revascularisation through EDAS. The second procedure was STA-MCA bypass in 6 patients (35.2%) (Fig. 1 and 2 show representative cases) and EDAS in 4 (23.5%).
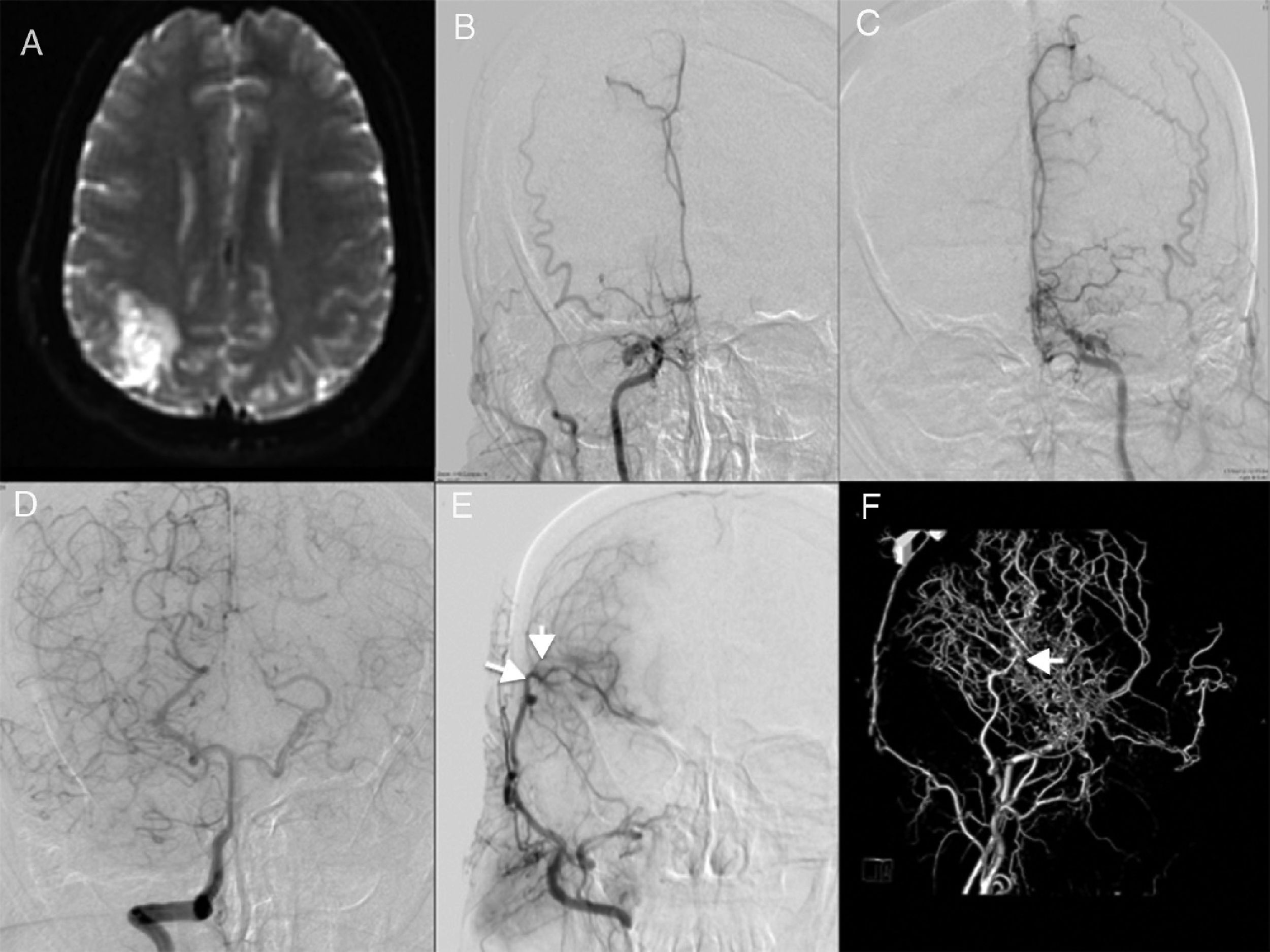
Representative case 1. Bilateral moyamoya disease with unilateral revascularisation. A) MRI showed ischaemia in the right parietal region. B and C) An angiography study revealed severe stenosis of both internal carotid arteries (Suzuki stage 5). D) Contrast administration to the right vertebral artery revealed bilateral collateral circulation. E) Follow-up angiography study after revascularisation from the superficial temporal artery to the middle cerebral artery, with excellent results (arrows). F) 3D angiography study showing the collateral circulation (arrow) through the parietal branch of the superficial temporal artery.
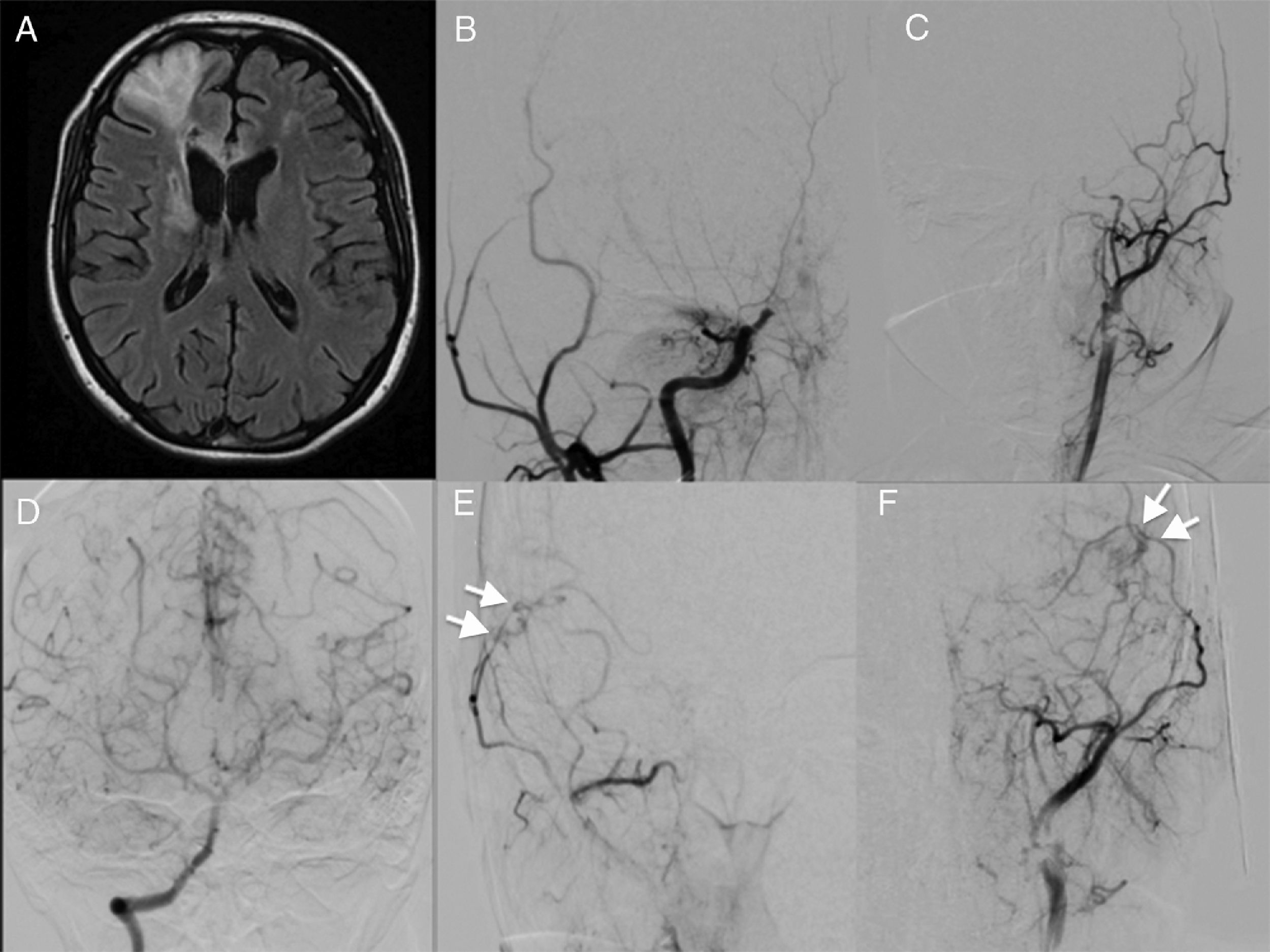
Representative case 2. Patient with bilateral moyamoya disease who underwent bilateral revascularisation. A) An MRI study revealed ischaemia in the right frontal lobe. B and C) An angiography study showed bilateral internal carotid artery occlusion (Suzuki stage 4). D) Contrast administration to the vertebral artery revealed collateral circulation through the posterior communicating arteries. E and F) Angiography study with contrast administration to the right external carotid artery, showing the site of anastomosis of the superficial temporal artery to the middle cerebral artery, with good flow (arrows; see video in Supplementary Material).
Mean follow-up time was 38.4 months (range, 2–120). mRS scores improved in 5 patients (29.4%), remained unchanged in 4 (23.5%), and decreased in one (5.8%). Clinical assessment and imaging studies did not show any further cerebrovascular events in any patient.
Of the 7 patients (41.1%) receiving conservative treatment, 3 (17.6%) presented ischaemic events and received antiplatelet therapy with acetylsalicylic acid, and 4 (23.5%) presented haemorrhagic events, and were not administered any drug. Mean follow-up time was 54 months (range, 2-130). mRS scores improved in 2 patients (11.7%), remained unchanged in 4 (23.5%), and decreased in one (5.8%) (Table 3). Two patients (11.7%) presented a further cerebrovascular event: one (5.8%) presented an ischaemic stroke and subsequently returned to his baseline condition; the other (5.8%) presented a haemorrhage associated with rapidly progressing haemodynamic and neurological impairment, leading to the patient’s death.
Statistical analysisIn the first statistical analysis, we compared initial and final mRS scores for the total sample, including all treatment groups (P = .1300). The Wilcoxon test was used to compare scores only in those patients undergoing direct or indirect revascularisation (P = .1012).
In a subsequent analysis, we compared the difference in mRS score (initial vs final) between treatment groups; we used the Kruskal-Wallis test due to the small size of our sample. For the comparison of all 3 treatment groups, we obtained a value of P = .1871. When we excluded the patient with type 2 diabetes mellitus from the group of patients receiving no treatment, the test yielded a value of P = .1311. Finally, we compared the surgery and no-treatment groups, obtaining a value of P = .043.
DiscussionThis is the first study into MD in a population of Mexican adults. Diagnosis was established according to the methods and criteria recommended by the Japanese guidelines and the international criteria accepted in clinical practice.9,12
As expected, the incidence and prevalence rates calculated based on our data are much lower than those for Korea and Japan. The female-to-male ratio in our sample (1.8:1) is lower than those reported in the United States (3:1),17 Finland (4.5:1),18 and Germany (4.25:1).19 Recent publications signal an increase in MD incidence in different non-Asian ethnic groups in the United States, including the Hispanic population, although to a lesser extent.13,14 Kainth et al.11 analysed data from 7473 patients (2236 paediatric patients and 5237 adults) diagnosed with MD in the United States between 2005 and 2008; Hispanic patients accounted for 11.9% of those aged 19-45 years and 5.9% of those aged older than 45. Uchino et al.14 report an incidence of 0.03 cases per 100 000 person-years in the Hispanic population in the state of California, estimating a national incidence rate of 10 new cases per year among the Hispanic population.14 In our study, MD accounted for 0.03% of cases of cerebrovascular disease in our hospital’s registry (n = 4481).20 MD should be considered within the group of rare causes of stroke, and in patients with stroke aged under 50 years, as is reported by Arboix et al.21,22 and confirmed in the present study: 82% of our patients were aged 50 years or younger at the time of onset. However, MD continues to be a very rare entity in Latin American countries, and few studies analyse its epidemiology (in paediatric or in adult patients) in the region. The average age at onset in our series is very similar to that reported in European studies (37.6 years, vs 37.1 in Finland and 40.5 in Germany). Once more, it should be noted that while MD is rare in the general population, it predominantly presents in younger individuals, and should be considered among the causes of stroke in young patients, as this group presents a clearly distinct clinical profile.21
In 2005, Quintana15 published a series of 10 patients with MD and its variants in Chile. In that study, 5 patients were older than 18 years (range, 18–46), all of whom were women with haemorrhagic presentation. Clinical presentation was predominantly atypical (unilateral MD in 4 patients and definitive MD in one). In 2007, Urrutia-Ruiz et al.16 published their experience of the diagnosis and management of the disease in 7 paediatric patients in Mexico between 1995 and 2005, reporting similar clinical behaviour to that observed in other series of paediatric patients. Our series is similar to those mentioned above in that most patients were women and presented the haemorrhagic form.
In 2 patients with haemorrhagic MD, CT findings were suggestive of multiple old infarcts in the same territory, which were presumably asymptomatic. We observed a lower percentage of patients with unilateral MD than those reported in other studies (5.8%, vs 23% in Finland and 17% in Germany),17–19 although figures from Europe are higher than those reported in Japan (10.6%).23
Presentation was more frequently haemorrhagic in our series (52.94%) than in samples from Japan (21%), Finland (15.7%), the United States (12%), and Germany (7.85%).17–19,23
Various studies indicate that revascularisation surgery, which may be direct or indirect according to the surgeon’s judgement, is a low-risk procedure that is effective for preventing further ischaemic events in patients with MD and considerably improves quality of life in both adult and paediatric patients. One of the largest prospective cohort studies demonstrated the effectiveness of both direct and indirect revascularisation for preventing recurrent ischaemic events in patients with MD; however, no significant difference was found for the prevention of recurrent haemorrhage.25–28 A recent meta-analysis found that direct revascularisation was more beneficial than indirect revascularisation for reducing the risk of subsequent ischaemic events.29 Of the 10 patients who underwent surgery, 9 underwent bilateral procedures; 5 had ischaemic MD and 5 had the haemorrhagic form. Of the 8 patients who were followed up for longer than one year, functional status improved in 6 and remained unchanged in 2 with respect to their status before surgery; no patient presented stroke recurrence. We found no statistically significant differences between direct and indirect revascularisation, although a difference was observed when we compared against patients not undergoing surgery. One patient, whose final mRS score was 4 points, presented cognitive impairment at onset; after indirect revascularisation by EDAS in the right hemisphere, he presented an acute right subdural haematoma in the immediate postoperative period, which was treated surgically. The increase observed in familial cases of MD is suggestive of genetic aetiology. Family history of the condition is recorded in 12.1% of patients in Japan and 2% of patients in the United States.24 In our sample, no patient had family history of MD. Comparison against more homogeneous populations is difficult due to the lack of series of Latin American patients.
While the characteristics of Mexican patients with MD do differ from those of populations from Germany and the United States, certain similarities were observed with the Japanese population, namely the predominance of female patients and the percentage of unilateral cases.
Ours is the first study to describe this disease in a subpopulation of Latin American adults, a group in which prevalence is low due to age and geographic region. Multicentre studies including hospitals from across Latin America would increase our understanding of the demographic and clinical characteristics of patients with MD, enabling us to more precisely establish the most successful treatment.
ConclusionsThis retrospective study is one of the first of its kind, reporting the largest series of patients with MD in a Mexican or Latin American population to date. Surgery was found to have better outcomes than conservative treatment, as measured with the mRS. However, the sample size represents a limitation. A future multicentre study would give a better picture of the incidence and prevalence of MD in our setting.
Conflicts of interestThe authors have no conflicts of interest to declare.
We are very grateful to the statistician and mathematician Jorge Alberto Vázquez Diosdado for reviewing our statistical analysis.
Please cite this article as: Nathal E, Serrano-Rubio A, Maciel E, Arauz A. Enfermedad Moyamoya en México. Experiencia Institucional. Neurología. 2021;36:603–610.