Numerous neurological manifestations of glycaemic alterations have been described, with hypoglycaemia being a well-known cause of epileptic seizures.1 It is less well known that neurological symptoms may present as the initial manifestation of hyperglycaemia,2 with epilepsia partialis continua being a characteristic form; these patients usually present focal motor seizures, unlike those with hypoglycaemia.3 Hyperosmolar non-ketotic hyperglycaemia is the type of hyperglycaemia most frequently associated with these symptoms, and is occasionally the initial manifestation of undiagnosed diabetes mellitus.4 The specific pathophysiological mechanism underlying this association is not fully understood, and ketosis may protect against seizures in patients with hyperglycaemia.4 We present the case of a patient with occipital epilepsia partialis continua in the context of non-ketotic hyperglycaemia, resolving with metabolic control. This case underscores the need to consider this entity, which, though rare, has considerable therapeutic and prognostic implications.
The patient was a 61-year-old man with hypertension, dyslipidaemia, and type 2 diabetes mellitus, which had previously been well controlled. He was being treated with telmisartan, simvastatin, fenofibrate, metformin, acetylsalicylic acid, and omeprazole. He had no history of seizures or any other relevant history. He began to present simple visual hallucinations of sparkling lights; onset was sudden and episodes were of variable duration (seconds to hours). Visual hallucinations affected both eyes and the entire visual field, and persisted when the eyes were closed. He reported reversal of vision metamorphopsia when the symptoms initially presented, although this resolved spontaneously. The patient presented no visual field deficits, headache, or any other focal neurological sign. These symptoms had progressed for 20 days before the patient consulted the department; the frequency of the episodes ranged from 5 to 20 per day, with no defined temporal or circadian pattern.
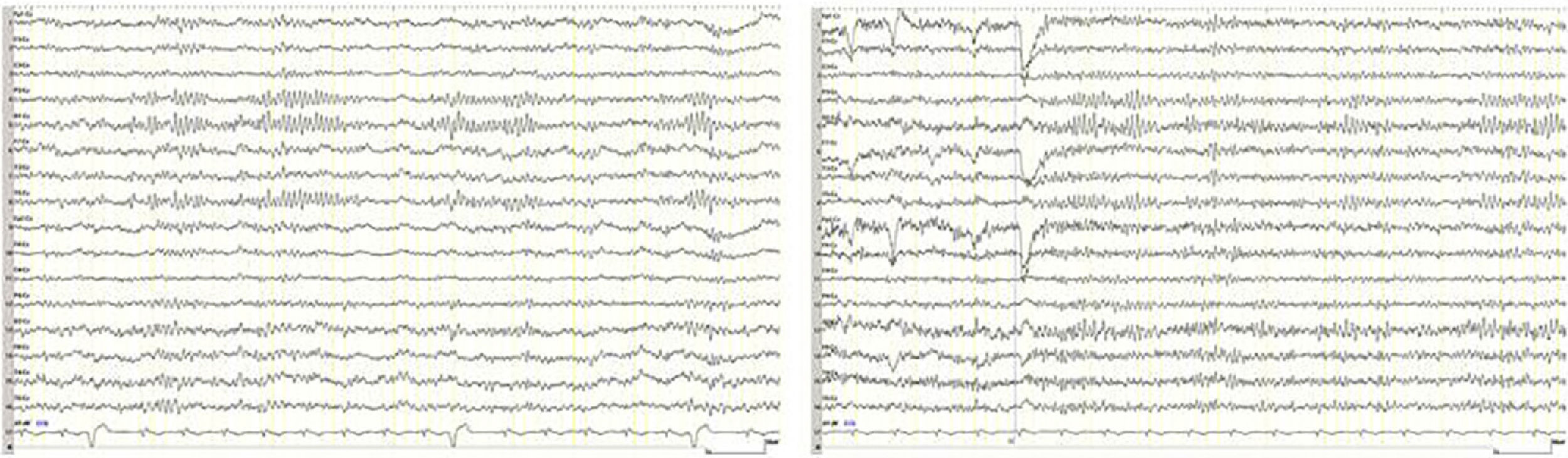
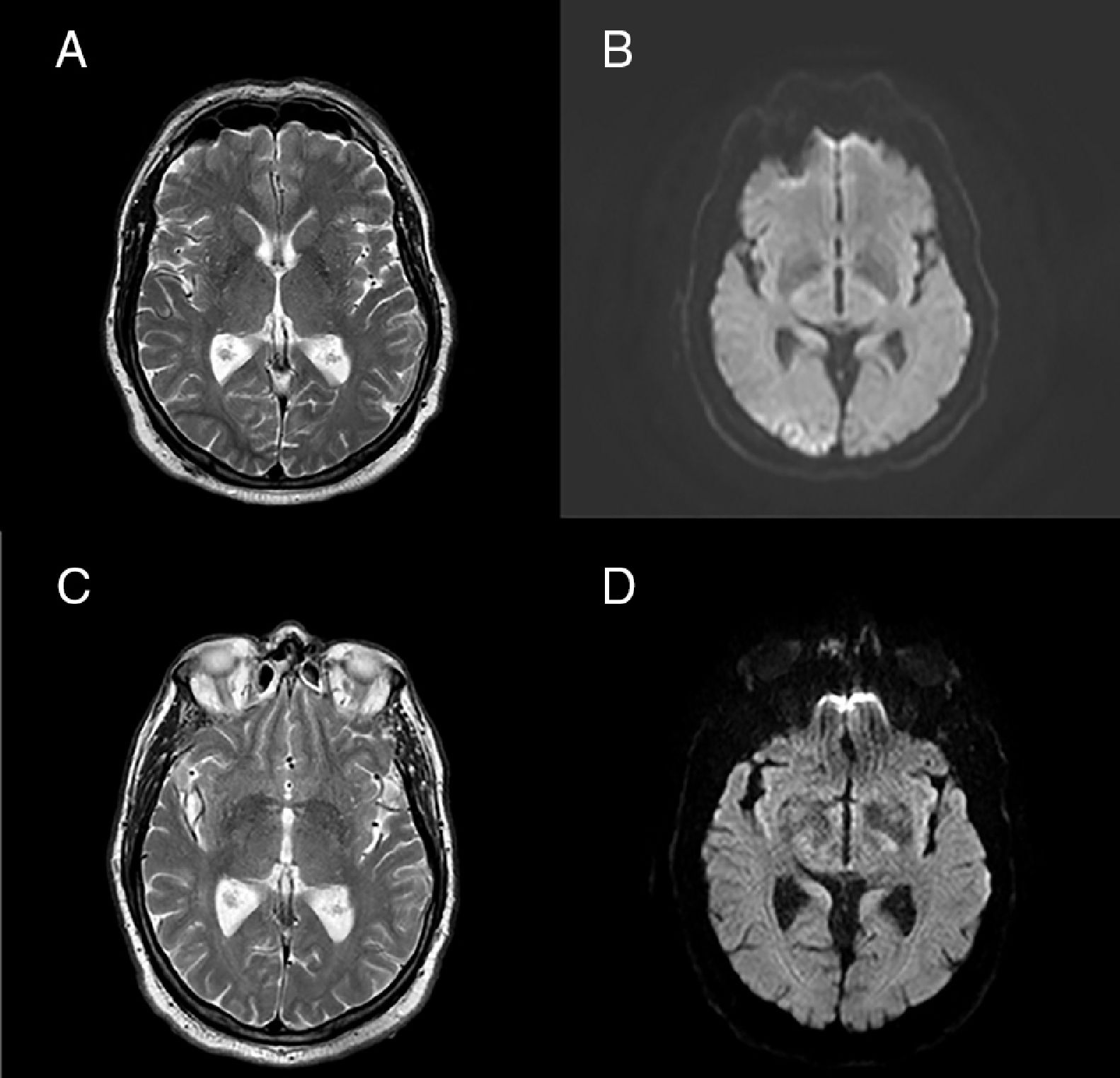
Neurological examination revealed no focal neurological deficits. A complete blood count revealed a glucose level of 382mg/dL, with 14% glycated haemoglobin. The only other alteration detected was known hypertriglyceridaemia. Results for ketone bodies were negative. The patient displayed EEG asymmetry, with abnormal occipital alpha waves in the right hemisphere (Fig. 1). The brain MRI study revealed T2 hyperintensity and diffusion restriction in the right occipital cortex, with T2 hypointensity in the adjacent subcortical region (Fig. 2). We also performed a head and neck MRI angiography and a transcranial and supra-aortic trunk Doppler ultrasound study, with no relevant findings. Insulin therapy was started and the visual symptoms resolved within hours and have not recurred to date (15 months of follow-up), with the patient presenting optimal glycaemic control. Findings from subsequent EEG and MRI studies were normal (Figs. 1 and 2). Antiepileptic drugs were not administered at any time.
Brain MRI study. (A) T2-weighted sequence showing hyperintensity in the right visual cortex and adjacent subcortical hypointensity. (B) Diffusion-weighted sequence showing an area of restricted diffusion in the right visual cortex. (C and D) T2- and diffusion-weighted sequences obtained after onset of insulin therapy, showing total resolution of the alterations.
Occipital epileptic seizures are rare in patients with hyperglycaemia5; in recent years, they have been linked to characteristic MRI findings, such as subcortical hypointensities on T2-weighted sequences and diffusion restriction in the occipital cortex.6–8 The pathophysiological mechanism underlying this association remains unknown, although it has been suggested that abnormal iron deposition may play a role.6 The resolution of clinical, radiological, and EEG signs after onset of diabetes treatment is essential to diagnosis, avoiding unnecessary complementary tests and the introduction of chronic antiepileptic treatment and the associated consequences.
We are grateful to the patient and his family for their collaboration.
Please cite this article as: Garzo Caldas N, Gomez Cibeira E, Saiz Díaz RA, Herrero Sanmartín A. Epilepsia parcial continua con foco occipital inducida por hiperglucemia no cetósica. Neurología. 2020;35:437–439.
This study was presented as a poster at the 15th Annual Meeting of the Madrid Association of Neurology, held in October 2017.