To determine the profile of children and adolescents diagnosed with autism spectrum disorder (ASD) in a comprehensive care centre in Bogota, Colombia.
Material and methodsA descriptive-correlational study with a sample of patients who had attended the institution from 2003 to 2009. Demographic and clinical aspects were evaluated and a correlation between the diagnosis and severity being analysed in search for risk factors.
ResultsA total of 138 patients were studied. The average age of onset was 21 months, and diagnosis had been made at 45 months. There was a male predominance (6.15:1). The predominant diagnosis was autistic syndrome (83%), followed by pervasive developmental disorder not otherwise specified (17%). There was no pathological background in the family history, during pregnancy or during the neonatal period. Motor development during the first year was normal but acquisition of language skills was compromised. The specific signs of ASD as regards the disorder in itself, communication skills, spontaneous speech, verbal comprehension, attention, imitation, use of objects, self-care and symbolic play were significantly related to the severity of the disease.
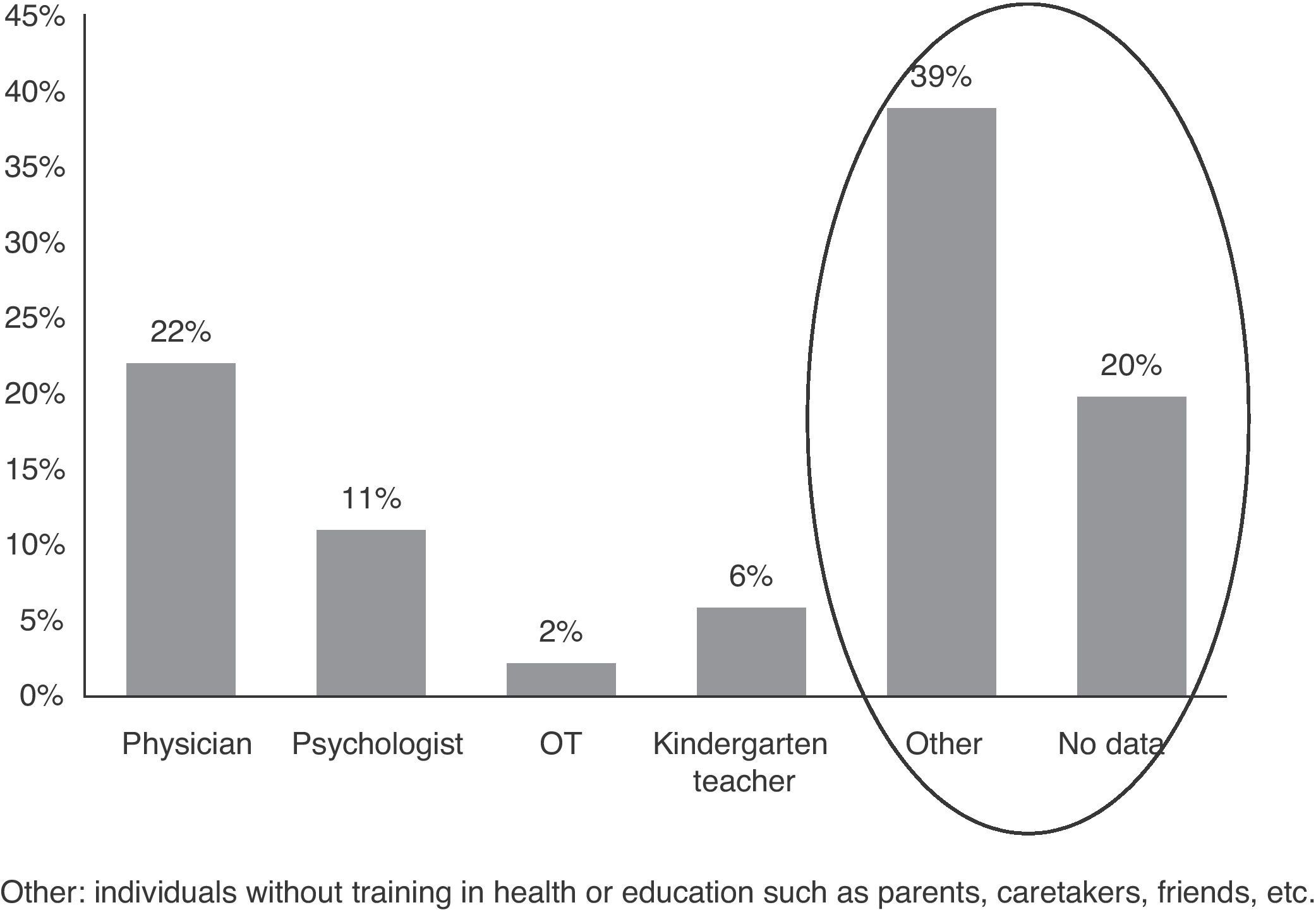
ConclusionsDiagnosis of ASD is still delayed in our population and usually after referral from someone other than a health professional. The most important problems were found in communication skills and relationships with peers. The study did not show significant associated risk factors.
Caracterizar la población de niños y adolescentes con diagnóstico de trastornos del espectro autista (TEA) en un centro de atención integral en Bogotá Colombia.
Material y métodosEstudio descriptivo-correlacional, de la población de pacientes que han asistido al centro desde el año 2003 hasta el 2009. Se evaluaron los aspectos demográficos y clínicos, y se realizó una correlación entre las variables con el diagnóstico y la severidad para la búsqueda de factores de riesgo.
ResultadosSe estudió a 138 pacientes. La edad promedio de inicio fue a los 21 meses y el diagnóstico a los 45. Hubo predominancia masculina (6,15:1). El diagnóstico mas frecuente fue síndrome autista (83%), seguido por trastorno generalizado del desarrollo no determinado (17%). No se encontraron antecedentes importantes en la familia, durante el embarazo ni en el periodo neonatal. El desarrollo motor durante el primer año fue normal mientras que el desarrollo de la comunicación verbal se encontró comprometido. Los signos específicos de TEA como el trastorno en referencia a sí mismo, comunicación, habla espontánea, comprensión verbal, atención, imitación, utilización de objetos, autocuidado y juego simbólico se relacionaron significativamente con la severidad del cuadro.
ConclusionesEl diagnostico de los TEA continúa siendo tardío en nuestra población y generalmente luego de la remisión de personal ajeno a la salud. Las alteraciones más importantes se encuentran en la comunicación y en la relación con los pares. En el estudio no se evidenciaron factores de riesgo que pudieran estar asociados.
According to the Diagnostic and Statistical Manual of Mental Disorders of the American Psychiatric Association (DSM IV), the criteria for what are known as generalised developmental disorders or autism spectrum disorders (ASDs) include a group of medical conditions that manifest during early childhood through involvement of developmental skills for social interaction and communication or by the presence of repetitive motor behaviours, stereotypes and unusual or peculiar interests. Taking into account specific characteristics, these entities have been named autistic disorder (AD), Asperger syndrome (AS), pervasive developmental disorder-not otherwise specified (PDD-NOS), Rett syndrome (RS) and childhood disintegrative disorder (DD).1
All ASDs share some of the classic symptoms of autism described by Kanner but differ in terms of severity, combination of affected areas, course and prognosis.2 In RS and DD there is a developmental regression after a period of normality (5–30 months in RS and 2–10 years in DD). In both disorders, a seemingly normal child loses the development achieved in motor skills, language and socialisation, developing some of the classic symptoms of autism. RS is a rare, progressive, neurological disease in which there is a deceleration of brain growth. It is assumed that DD is due to acquired neurological damage, but in many cases its aetiology is unknown. AS is defined by impairment in 2 domains of the autism triad: social interaction and stereotyped behaviours, peculiar interests and activities. Although its diagnosis does not require changes in communication, such constraints are often present, especially in the pragmatics of language. The diagnosis of PDD-NOS is reserved for cases in which there are no symptoms of autism, but there are no criteria for any of the other 4 ASDs because the symptoms appear minimally or their onset is belated.3
Early detection and an appropriate intervention can mitigate the long-term deleterious effects and improve quality of life. The importance of ASD lies in their high prevalence, which is between 60 and 70/10,000 inhabitants. They are distributed according to the different types of clinical profiles as follows4: AD 20/10,000; PDD-NOS 30/10,000; AS 6/10,000; RS 1/10,000–20,000 and childhood disintegrative disorder 2/100,000.
In terms of incidence, developed countries present 1 new case per year for every 500–700 newborns. However, up to 40% of patients who received a diagnosis of ASD at some point did not have the diagnosis confirmed subsequently with specific tests.5 The male to female ratio is 4:1, except for RS, which is more common in the female population.6 No studies could be found evaluating the epidemiology of this disorder in Colombia or determining its presentation, demographics or symptoms.
This project aimed to study a population of children and adolescents attending ANTHIROS, a reference centre for the diagnosis and rehabilitation of patients with ASD in Bogotá, Colombia. We described their clinical features and relevant diagnostic history so as to determine the existence of risk factors during the different periods of development. We also analysed the possible association between these and the presence and severity of ASD.
Patients and methodsWe conducted a descriptive, observational study of a series of children and adolescents diagnosed with autism spectrum disorder, taken from the population of children who attended the child development institution ANTHIROS for diagnosis and rehabilitation. We excluded all medical records of children younger than 2 years and older than 18 years, as well as those in which it was clear that the children suffered from severe hearing loss, metabolic disorders, Gilles de la Tourette syndrome, meningitis, epileptic encephalopathy, genetic syndromes with known cause or mental retardation with symptoms similar to those found in ASD.
We reviewed the medical records of all patients examined at the institution between 2003 and 2009. We recorded those variables associated with the risk of ASD onset, as well as those considered in the child evaluation protocol of the institution. Among them, we recorded demographic variables, family and personal history (prenatal, perinatal, postnatal), motor, speech and psycho-emotional development and behavioural variables.
We created an Excel database to store the information according to the instrument designed previously. In order to ensure data accuracy, we reviewed each of the medical records to confirm the diagnosis prior to entering the information into the database. We excluded from the study those records not having complete information or those in which the quality of the information did not allow for conclusive identification of the information relevant to the study. We conducted a review of the database to identify any missing data or alterations during typing.
Data for qualitative variables such as demographic, aetiological, and evaluative factors and other factors were analysed using measurements of absolute and relative frequencies expressed as percentages. Quantitative variables were expressed using measures of central tendency such as mean and median, and dispersion variables were expressed using range and standard deviation. For the purpose of calculating the mean in the case of acquisition of development patterns in patients who had not acquired a specific item, we took their age in months at the time of admission to the institution. We used the Pearson chi-square association test and the Fisher exact probability test (expected values <5) to assess the association between various risk factors and the presence and severity of ASD. Likewise, we used the Kruskal–Wallis test to evaluate the medians. Results were considered positive when the significance level was less than 5% (P<.05). Finally, we conducted an associative model of multivariate analysis using unconditional logistic regression of diagnoses and clinical signs to assess the severity using a hierarchical selection model and we assessed the multicollinearity among the different factors that made up the model.
This study was classified as safe without risks according to the standards set by the Health Ministry of Colombia. In addition, we followed the recommendations of the Helsinki Declaration of the World Medical Association. The protocol was approved by the institution prior to gaining access to medical histories and was also approved by the research ethics committee at Universidad del Rosario. All data were handled through the clinical history ID number, with no mention to names of patients or their families in order to preserve confidentiality.
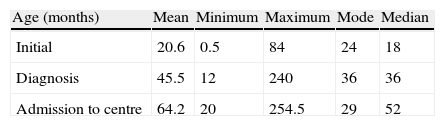
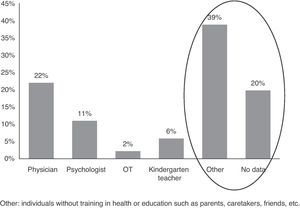
ResultsWe evaluated the medical records of 138 patients, 52% of whom were from the city of Bogotá and the rest from other cities throughout the country. The mean age of onset according to parents was 21 months, but the diagnosis took place at 45 months (Table 1). There was male predominance, with 119 males and 19 females (6.15:1). Patients were admitted to the institution with a mean age of 64 months, mostly referred by people outside the health or education services (Fig. 1).
Considering the DSM IV criteria, the diagnosis established through evaluation by an interdisciplinary team corresponded to autistic syndrome in 109 cases (80%), followed by PDD-NOS in 22 (17%). As expected, the number of children diagnosed with childhood disintegrative disorder or AS was very low and there were no girls with Rett syndrome.
Children were classified as follows, according to severity as assessed by the childhood autism rating scale (CARS)7:
- -
Not autistic (score 15–29): 2.2%.
- -
Moderately abnormal (score 30–36): 45.6%.
- -
Severely autistic (score 37–60): 52.2%.
These data are significantly related to the type of diagnosis, being more severe in children with AS, followed by those who presented childhood disintegrative disorder (P=.000).
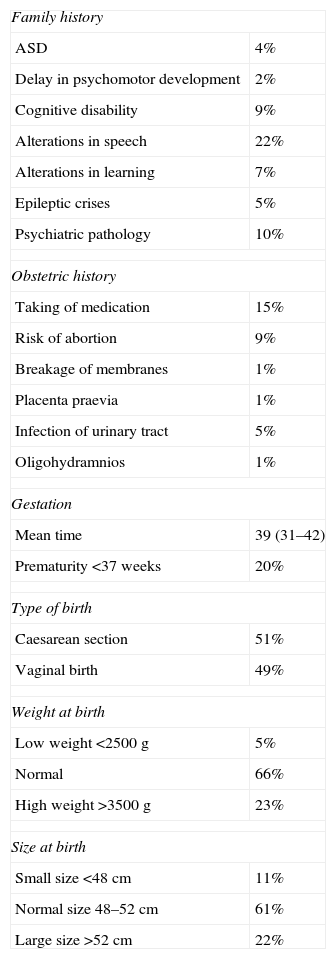
The mean age of the mother was 30 (16–43) years and that of the father was 33 (19–58) years. No consanguinity was found in 84% of them. No significant family history during pregnancy or the neonatal period was observed, except for some family members with conditions that could somehow be related to ASD. A total of 51% of cases were born by caesarean section and 20% of premature infants were identified (Table 2). Perinatal complications, specifically acute foetal distress, took place in only 12% and severity was not greater since neither neonatal resuscitation nor neonatal intensive care were required. No neurological disorders were reported in the newborn. Weight and size were appropriate in 70% of children.
Positive precedents in the clinical history.
| Family history | |
| ASD | 4% |
| Delay in psychomotor development | 2% |
| Cognitive disability | 9% |
| Alterations in speech | 22% |
| Alterations in learning | 7% |
| Epileptic crises | 5% |
| Psychiatric pathology | 10% |
| Obstetric history | |
| Taking of medication | 15% |
| Risk of abortion | 9% |
| Breakage of membranes | 1% |
| Placenta praevia | 1% |
| Infection of urinary tract | 5% |
| Oligohydramnios | 1% |
| Gestation | |
| Mean time | 39 (31–42) |
| Prematurity <37 weeks | 20% |
| Type of birth | |
| Caesarean section | 51% |
| Vaginal birth | 49% |
| Weight at birth | |
| Low weight <2500g | 5% |
| Normal | 66% |
| High weight >3500g | 23% |
| Size at birth | |
| Small size <48cm | 11% |
| Normal size 48–52cm | 61% |
| Large size >52cm | 22% |
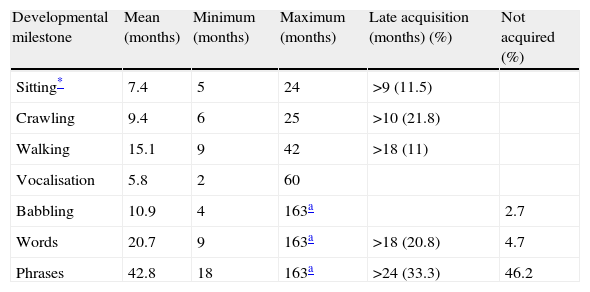
Motor development during the first year was generally normal, but an association was found between late onset of sitting and severity of ASD (P=.000). With regard to the development of verbal expression (babbling, words and phrases), the acquisition was generally above the expected range for the age and a significant number of children who had not acquired verbal communication skills were observed at the time of admission at the institution (Table 3).
Acquisition age of different developmental milestone.
| Developmental milestone | Mean (months) | Minimum (months) | Maximum (months) | Late acquisition (months) (%) | Not acquired (%) |
| Sitting* | 7.4 | 5 | 24 | >9 (11.5) | |
| Crawling | 9.4 | 6 | 25 | >10 (21.8) | |
| Walking | 15.1 | 9 | 42 | >18 (11) | |
| Vocalisation | 5.8 | 2 | 60 | ||
| Babbling | 10.9 | 4 | 163a | 2.7 | |
| Words | 20.7 | 9 | 163a | >18 (20.8) | 4.7 |
| Phrases | 42.8 | 18 | 163a | >24 (33.3) | 46.2 |
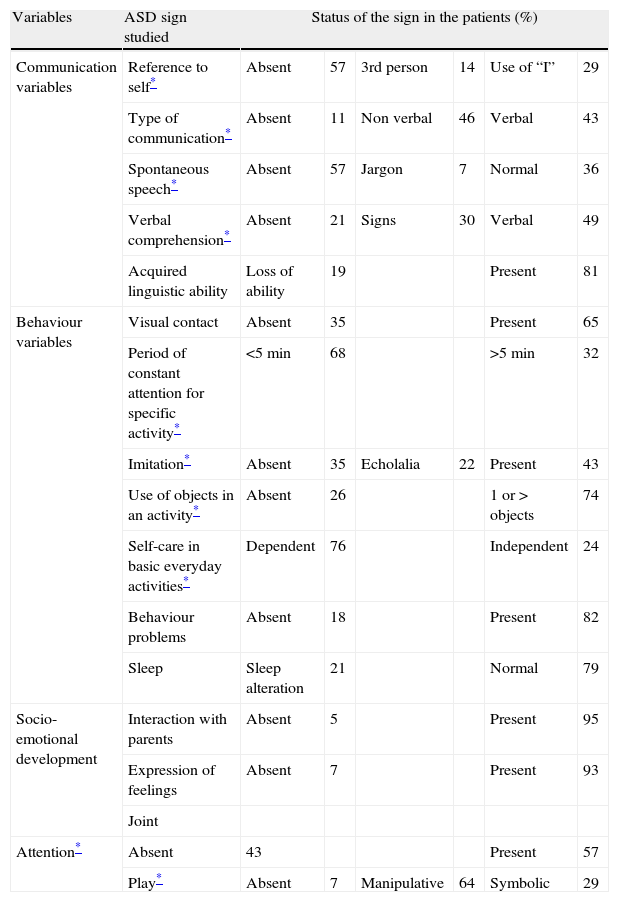
The areas of self-reference signs, communication disorders, spontaneous speech, verbal comprehension, attention, imitation, use of objects, self-care and play were found to be altered and significantly related to the severity of the disease (Table 4).
Evaluation of the specific signs of ASD expressed in percentages (%).
| Variables | ASD sign studied | Status of the sign in the patients (%) | |||||
| Communication variables | Reference to self* | Absent | 57 | 3rd person | 14 | Use of “I” | 29 |
| Type of communication* | Absent | 11 | Non verbal | 46 | Verbal | 43 | |
| Spontaneous speech* | Absent | 57 | Jargon | 7 | Normal | 36 | |
| Verbal comprehension* | Absent | 21 | Signs | 30 | Verbal | 49 | |
| Acquired linguistic ability | Loss of ability | 19 | Present | 81 | |||
| Behaviour variables | Visual contact | Absent | 35 | Present | 65 | ||
| Period of constant attention for specific activity* | <5min | 68 | >5min | 32 | |||
| Imitation* | Absent | 35 | Echolalia | 22 | Present | 43 | |
| Use of objects in an activity* | Absent | 26 | 1 or > objects | 74 | |||
| Self-care in basic everyday activities* | Dependent | 76 | Independent | 24 | |||
| Behaviour problems | Absent | 18 | Present | 82 | |||
| Sleep | Sleep alteration | 21 | Normal | 79 | |||
| Socio-emotional development | Interaction with parents | Absent | 5 | Present | 95 | ||
| Expression of feelings | Absent | 7 | Present | 93 | |||
| Joint | |||||||
| Attention* | Absent | 43 | Present | 57 | |||
| Play* | Absent | 7 | Manipulative | 64 | Symbolic | 29 | |
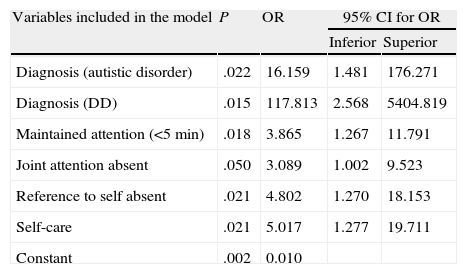
When studying the multivariate logistic regression model, we found a significant explanation for the severity of ASD using the following factors: type of diagnosis (AS and DD), lack of sustained attention, lack of joint attention, absence of reference to self and dependence for basic self-care activities. We found the existence of multicollinearity between the various factors specific to ASD, so that absence of communication, spontaneous speech and verbal comprehension could have also been included within the model (Table 5).
Multivariate model used to explain ASD severity.
| Variables included in the model | P | OR | 95% CI for OR | |
| Inferior | Superior | |||
| Diagnosis (autistic disorder) | .022 | 16.159 | 1.481 | 176.271 |
| Diagnosis (DD) | .015 | 117.813 | 2.568 | 5404.819 |
| Maintained attention (<5min) | .018 | 3.865 | 1.267 | 11.791 |
| Joint attention absent | .050 | 3.089 | 1.002 | 9.523 |
| Reference to self absent | .021 | 4.802 | 1.270 | 18.153 |
| Self-care | .021 | 5.017 | 1.277 | 19.711 |
| Constant | .002 | 0.010 | ||
CI: confidence interval; DD: disintegrative disorder; OR: odds ratio; P: statistical significance value.
ASDs are characterised by persistent disabilities in several areas of development: inability in reciprocal social interaction, inability to communicate or the presence of repetitive motor behaviours, stereotypes and unusual and/or peculiar interests.1,8 Qualitatively, the impairments defining these conditions are clearly deviant relative to the developmental level or mental age of the individual. All these disorders are usually evident from the earliest years of life and can often be associated with cognitive dysfunction of varying severity. They may also be present accompanying a diverse group of neurological disorders such as chromosomal abnormalities, congenital infections and structural abnormalities of the central nervous system.9,10 All ASDs share some of the classic symptoms of autism described previously, but they differ in terms of severity, combination of affected areas, course and prognosis. In RS and DD there is a developmental regression after a period of normality (5–30 months in RS and 2–10 years in DD). In both disorders, a seemingly normal child loses his/her development in motor skills, language and socialisation, and develops some of the classic symptoms of autism.11 Although the diagnosis does not require communication disorders to be present, such impairments are frequently observed, especially in the pragmatics of language.12 The diagnosis of PDD-NOS is reserved for cases that do not exhibit symptoms of autism but do not meet the criteria for any of the other 4 ASDs because the symptoms are minimal or their onset is belated.3
Some of the difficulties encountered in these children may be modified with appropriate treatment started early. For this reason, the American Academy of Paediatrics recommends close monitoring of all children during the first 2 years, in order to obtain a diagnosis of ASD as quickly as possible. However, some studies report that the mean age of identification is around 5.5–6 years. This age is related to the intellectual level of children, the regression in development presented and maternal education, among other factors.9,11,13,14 The lack of access to specialised medical services and confusion among uninformed physicians delay an accurate diagnosis. The families of these children are often given 3 or 4 diagnoses prior to that of autism or AS.11,13 In addition, diagnostic error is common and generates high costs for families and service providers. In the present study, children were identified at a relatively early age (45 months), but we also observed a significant gap with respect to the start of treatment (64 months).
We did not find any significant factors in the group of children studied in this investigation that could be related to a positive family history or relevant prenatal and perinatal problems. The only points that attracted our attention were, firstly, that half of the population was born by caesarean section, which was significant at a national level, where the mean figure for caesarean sections in the last 5 years was around 36%.15 This is a predisposing factor considered by Bilder et al.,10 but in their case it was related more to the presentation of the foetus than to the surgery itself. However, we must keep in mind that this type of delivery has increased significantly in obstetric practice and more so in the case of higher social strata.16 The second factor was the figure of premature deliveries. This was slightly higher than the national average (17%), but was also associated with the severity of the disorder. As mentioned by Buchmayer,17 the increased risk of ASD in premature infants may possibly be more related with postnatal problems presented by these children than with the condition of prematurity itself.17 The gender difference found in favour of males (6.5:1) was slightly greater than that reported in the literature but no explanations can be raised, given the sampling to our interest employed in this study.18,19
Although advanced maternal and paternal age has also been associated with the presence of this clinical condition, in our study group the mean age of parents was 30 and 33 years, respectively.20,21 Moreover, unlike the reports in the literature regarding the prevalence of psychiatric disorders in the relatives of the autistic population, the families of the study group presented no significant psychiatric history (10%).22
Since Kanner's original description, which considered autism as a psychosis of childhood arising from maternal negligence,1,23 multiple works and approaches have shown that ASDs consist of neurodevelopmental disorders, primarily of the basic communication skills, development of social interaction and specific aspects of conduct.10,11,24 Although in the present study, psychomotor development during the first year averaged normal, there was a significant percentage of children with a delay in motor and language skills acquisition. The latter were significantly altered, especially from the second year and, as suggested by some authors, this could be a predictor of a subsequent diagnosis.25–28 It is likely that this alteration of language development starts during the stage of preverbal communication with failures in the use and recognition of gestures and objects, as well as the understanding of everyday life situations.21,26 Similarly, sound production patterns are often abnormal even before the start of spoken language.27 In general, motor development has not represented a compromised aspect in children with ASD from the point of view of gross skill acquisition, such as sitting, crawling or walking.24 However, there is a dysfunction in fine motor skills and coordination that can be clinically represented by academic learning problems, repetitive movements, mannerisms and stereotypes.22,29 The presence of a delay in the acquisition of sitting in the children tested may suggest that these children are part of the group with greatest severity within the overall spectrum.
Regarding the remaining points mentioned, we observed that all the children presented alterations to greater or lesser degree in communication, social relations and behaviour, which was reported as a primary element of diagnosis and placement within the spectrum when taking into account the degree of severity.23
In conclusion, the present study describes the background and presentation of a selected population of children with ASD from a reference centre. However, these data do not allow inferences to the general population. Consequently, a future national collaborative study with children from different population groups and social strata would be desirable. In this way, it would be possible to evaluate aspects such as incidence, prevalence, risk factors and aetiology. Finally, mechanisms for early detection could be proposed favouring feasible and effective intervention within our environment, in order to minimise the deleterious effects of this clinical condition.
FinancingThis work was supported in part by the Universidad del Rosario (salaries of researchers and recruitment of young researchers).
Conflict of interestsThe authors have no conflicts of interest to declare.
The authors wish to thank Dr. Juan Fernando Muñoz, psychiatrist for children and adolescents, for his collaboration in the initial planning of this work; the medical students from the School of Medicine and Health Sciences at Universidad del Rosario Nicole Motta Rojas, Luisa Díaz Galindo, Felipe Castilla Gómez and Javier Aluja León, for their cooperation in producing databases; and, finally, Dr. Milciades Ibáñez, for statistical advice.
Please cite this article as: Talero-Gutiérrez C, et al. Caracterización de niños y adolescentes con trastornos del espectro autista en una institución de Bogotá, Colombia. Neurología. 2011;27:90–6.