Daytime and nigh-time excessive, generalised recurrent sweating is an infrequent and under-reported symptom in elderly patients. When present, however, it may point to a number of conditions, including tumours.1,2 Acute confusional state (ACE) or delirium is frequent among elderly patients and may be the reason for institutionalisation or an intercurrent condition in institutionalised patients. Cancer is a possible diagnosis for this manifestation.3 Both diaphoresis and delirium are regarded as syndromes due to the wide range of causes potentially triggering them.4
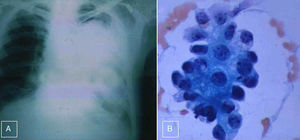
We present the case of a 79-year-old man who was brought in the morning to the emergency department of our hospital due to behavioural changes, inattention, incoherent thinking, and visual hallucinations. The night before he had displayed normal behaviour and cognition. He had no history of vascular risk factors and had previously been diagnosed with right bundle branch block. Our patient had been taking 50μg levothyroxine during fasting for the last 20 years and was not receiving any psychoactive drugs. Over the previous year he had experienced episodes of excessive sweating in the evening and night 2-3 times per week, which forced him to change clothes. These episodes were not associated with hyperthermia; complete blood counts performed on 2 occasions in the previous months revealed normal results. He displayed diaphoresis the night before admission. Physical examination revealed no abnormalities except for mild gait instability, increased base of support, and side stepping. Our patient displayed cognitive and behavioural alterations and was inattentive; we were unable to perform more specific tests due to lack of patient cooperation. He met the diagnostic criteria for ACE.5 Results from the heart examination were normal except for right bundle branch block; he displayed normal heart rate and blood pressure level, and required no additional medications. A brain CT scan revealed moderate cortical and central atrophy, a typical finding for his age, and no lesions in or around the brain parenchyma. A complete blood count showed normal results except for low glucose levels (26mg per cent). We suspected a typing error since our patient was not diabetic and was not taking any antidiabetic drugs. A blood sugar test revealed a glucose level of 28mg per cent; we therefore started treatment with glucose 10%. Chest radiography revealed a large radiopaque mass on the left side (Fig. 1A). ACE resolved 2hours after glucose infusion. An insulin test disclosed 7.5mIU/mL (normal range: <10mIU/mL). A lung biopsy revealed mesothelioma with typical cells and reactive fibrosis (Fig. 1B). We ruled out asbestos exposure based on reports from our patient's relatives. Our patient was discharged one week later. We decided not to excise the mesothelioma in view of its proximity to the mediastinum and our patient's advanced age. He received medications similar to those prior to admission, started a carbohydrate-rich diet, and was instructed to eat every 3hours, even at night. Our patient was followed-up every 3 months for 5 years; he experienced no further episodes of diaphoresis or ACE, his cognitive function was normal, and he was independent for daily living activities. Follow-up chest radiographies were performed every 4 months and revealed no changes compared to the image shown in Fig. 1A. Our patient was diagnosed with benign pleural fibrous mesothelioma associated with occasional episodes of hypoglycaemia6; these episodes were responsible for long-term diaphoresis and ACE. Low glucose levels triggers an exaggerated adrenergic response which may cause behavioural disorders and profuse sweating. Insulinoma causes similar symptoms but is associated with hyperinsulinaemia.7 Benign or malignant mesothelioma and other types of tumours produce a peptide with similar structure and activity to insulin (insulin-like growth factor 2).8 Diaphoresis and ACE in elderly patients may be helpful for early diagnosis and treatment of some types of tumours.
The authors have no conflicts of interest to declare. The study and figures were approved for publication by the Training and Research Committee at our hospital. Confidentiality of patient data was preserved.
Please cite this article as: Domínguez RO, Cárdenas EM, Marulanda YHS, Bartolomé EL. Diaforesis recurrente, estado confusional agudo y mesotelioma pleural. Neurología. 2017;32:484–485.