ß-Thalassaemia is a group of autosomal recessive forms of anaemia caused by decreased or absent synthesis of the β chains of haemoglobin. The condition is endemic to the Mediterranean region. Thalassaemia major manifests with symptoms of haemolytic anaemia and extramedullary haematopoiesis. Spinal cord compression is an extremely rare complication of extramedullary haematopoiesis, observed in fewer than 1% of patients. We present the case of a patient with progressive paraparesis secondary to thoracolumbar spinal cord compression by epidural masses resulting from extramedullary haematopoiesis; the patient was treated with haemotherapy, hydroxycarbamide, and radiotherapy.
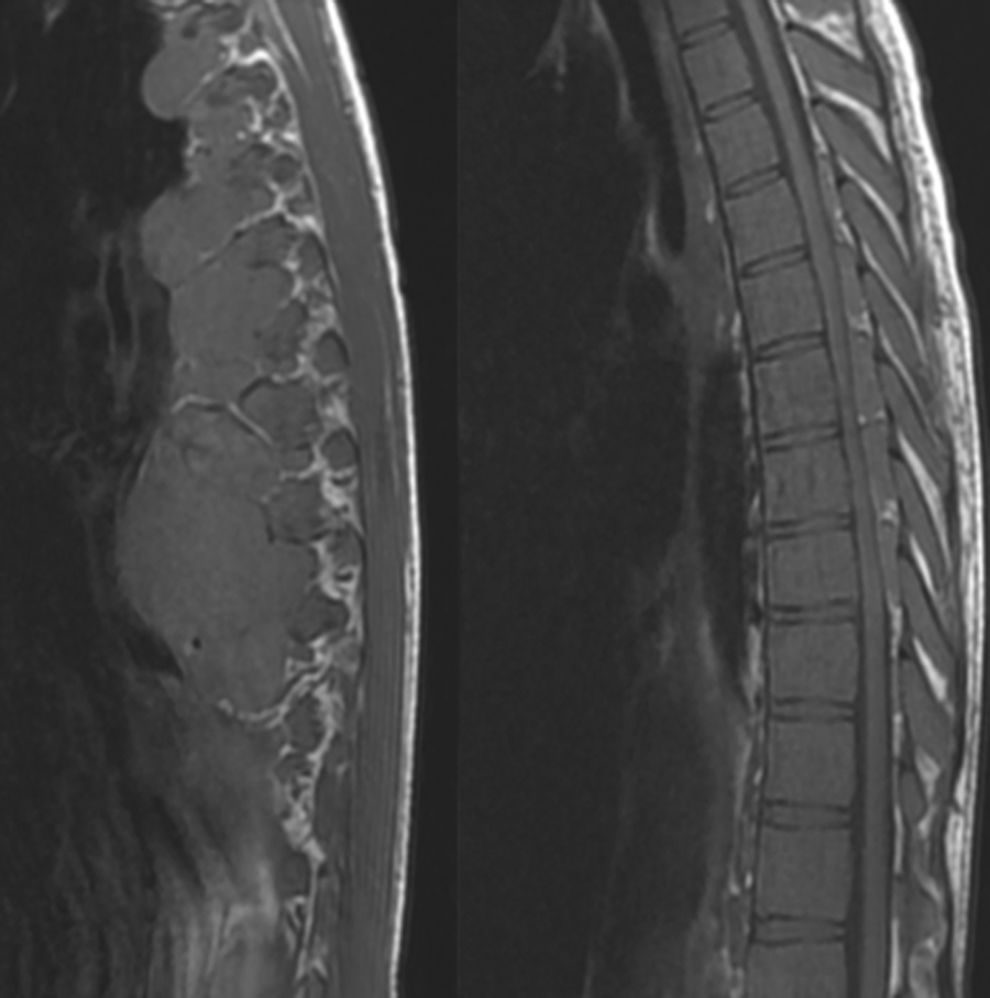
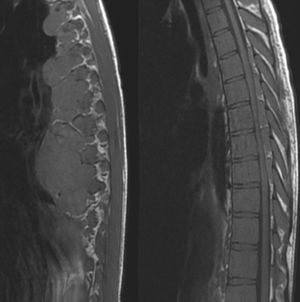
The patient was a 28-year-old woman who was diagnosed with ß-thalassaemia major at the age of 5; she underwent splenectomy and received periodic blood transfusions. Due to the transfusions received, the patient has Child–Pugh class A liver disease secondary to hepatitis C virus infection. She was lost to follow-up some years previously. She visited the emergency department due to urinary retention and spastic paraparesis. She reported a 2-month history of ataxia and progressive sensory impairment in the lower limbs. The physical examination showed malar prominence, depressed nasal bridge, pale skin, and mild jaundice. The patient showed loss of strength in the lower limbs (4/5), associated with hyperreflexia, ankle clonus, bilateral Babinski sign, and sensory level at T10. Results from a complete blood count were normal except for a haemoglobin level of 6g/dL and mild leukocytosis. A chest and abdomen MRI scan revealed spinal cord compression by paravertebral and epidural masses located at T5-T9, associated with signs of myelopathy at T9; the paravertebral mass measured 6.8cm×5.1cm on the axial plane. The lumbar spine also displayed multiple nodules deforming and compressing the thecal sac, compatible with extramedullary haematopoiesis (Fig. 1).
A thoracolumbar MRI scan revealed spinal cord compression due to paravertebral and epidural masses at the level of T5-T9, associated with signs of myelopathy at T9; the paravertebral mass measured 6.8cm×5.1cm on the axial plane. The lumbar spinal cord displayed multiple nodules compressing the thecal sac, compatible with extramedullary haematopoiesis.
The patient was diagnosed with spinal cord compression secondary to extramedullary haematopoiesis. Treatment was started with 16mg intravenous dexamethasone and blood transfusions; haemoglobin level reached 12.5g/dL at 72hours after admission. She also received radiotherapy in the area affected by extramedullary haematopoiesis (2Gy in 10 fractions of 200cGy), and was administered hydroxycarbamide 500mg/day. The patient improved progressively, recovering urinary function, strength, and sensitivity almost completely by 14 days after admission. At 18 months, the patient has no neurological symptoms and has haemoglobin levels above 10g/dL; she receives blood transfusions on a monthly basis and hydroxycarbamide at 500mg/day.
Extramedullary haematopoiesis is a common compensatory mechanism in cases of poorly controlled haemolytic anaemia. Its incidence in patients with β-thalassaemia major who are receiving multiple blood transfusions is below 1%; location is paraspinal in 11% to 15% of cases.1 Spinal cord compression is most frequent at the thoracic level, given the restricted mobility and the smaller diameter of the spinal canal in this area; up to 80% of cases are asymptomatic, however.2 Neurological symptoms range from low back pain to paraplegia. MRI typically reveals paraspinal masses. These are isointense on T1- and T2-weighted sequences when they are recent and hypervascular, whereas older or regressing masses are either hyperintense, if they are predominantly fatty, or hypointense if they contain iron deposits.1 Unlike metastases, these masses do not show gadolinium uptake.3 Biopsy is not recommended for diagnosis due to the high risk of massive bleeding2; this technique is only used for elderly patients in cases of high suspicion of malignancies, or in those displaying non-specific symptoms and imaging findings. Differential diagnosis should include metastasis, epidural abscess, multiple myeloma, and lymphoma; however, extramedullary haematopoiesis is usually simple to diagnose unless the patient displays a single, unilateral, active lesion.2
Several other cases of extramedullary haematopoiesis have been published since Gatto et al.5 reported the first case in 1954; management continues to be controversial, however. At present, treatment aims to raise haemoglobin levels above 10g/dL6 with blood transfusions. Given that extramedullary haematopoiesis is a compensatory mechanism for anaemia, transfusions reduce the need for this mechanism, quickly reducing the size of haematopoietic masses. The first transfusions are usually combined with administration of hydroxycarbamide7; this ribonucleotide reductase inhibitor stimulates the synthesis of fetal haemoglobin, decreasing the need for extramedullary haematopoiesis. Despite the usefulness of combination therapy with hydroxycarbamide plus haemotherapy, the drug's profile for long-term use is not fully established.8,9
Combination therapy usually results in slow, incomplete recovery.10 Therefore, patients with acute, severe neurological involvement also require low-dose radiotherapy (900-3500cGy), which is associated with positive outcomes within 3-7 days in over 50% of cases, given that haematopoietic tissue is highly radiosensitive.1,10 Patients with mild neurological involvement only receive radiotherapy if haemotherapy fails or in the event of recurrence; radiotherapy is the best option to prevent recurrences.5
Decompressive laminectomy is indicated for refractory cases or when other treatments are contraindicated.3,4 This surgical technique achieves immediate decompression and enables histological diagnosis, but is associated with a high risk of bleeding. In the long term, the condition may cause kyphosis and instability; surgical correction of kyphosis should be performed when possible. Sudden excision of haematopoietic elements in these patients may lead to decompensation of the underlying disease. Patients usually display diffuse involvement of several vertebral bodies, which makes surgery suitable only in cases of acute, severe, progressive neurological involvement.
ß-Thalassaemia may cause reversible paraplegia; the condition should therefore be included in the differential diagnosis of compressive lesions in patients with chronic anaemia. Unlike in such other causes of spinal cord compression as tumours or trauma, medical treatment alone (haemotherapy, hydroxycarbamide, and low-dose radiotherapy) can lead to early recovery in patients with extramedullary haematopoiesis; surgery should be limited to cases with poor clinical progression. Personalised treatment may therefore achieve complete, stable recovery of neurological symptoms.
Please cite this article as: Duque SG, Jureschke FR, Leal RG. Compresión medular con paraparesia reversible en paciente con ß-talasemia. Neurología. 2019;34:270–272.