The prevalence of sexual dysfunction (SD) in men with multiple sclerosis (MS) is reported variously in different studies. The most common form of SD in these patients is erectile dysfunction (ED). The goal of this systematic review and meta-analysis is to determine the pooled prevalence of SD and ED in men suffering from MS.
MethodsWe searched PubMed, Scopus, EMBASE, CINAHL, Web of Science, and gray literature (references of references, and congress abstracts) up to 14th November 2020.
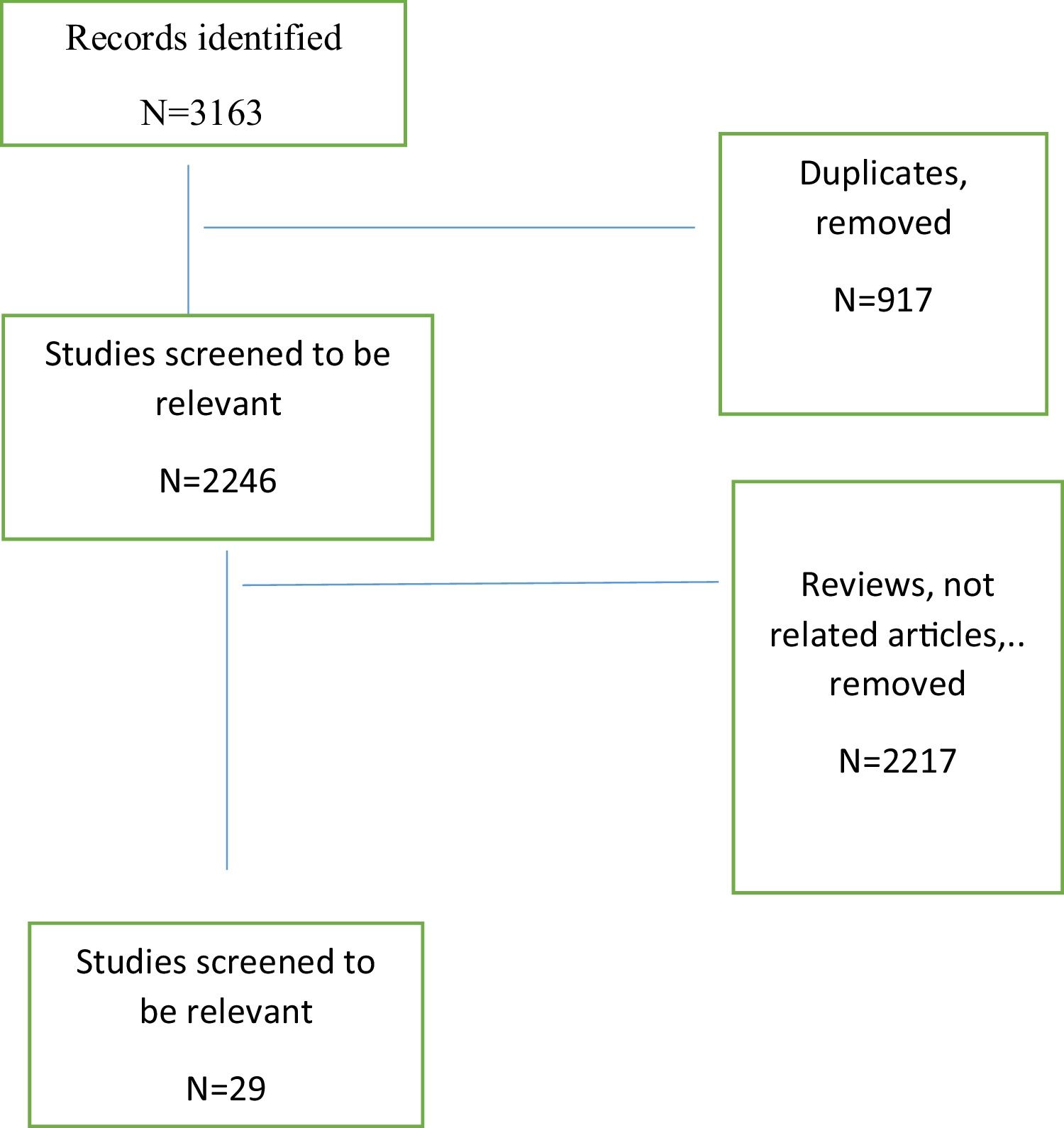
ResultsWe found 3163 studies by primary search, 2246 were included after deletion of duplicates. Finally, 29 studies were included for meta-analysis. A total of 3349 patients were evaluated. The pooled prevalence of SD was 66% (95% CI: 64%–69%). The pooled prevalence of erectile dysfunction was 49% (95% CI: 47%–50%).
ConclusionSexual dysfunction is a prevalent complication of MS in male patients which should be considered by clinicians.
La prevalencia de la disfunción sexual (SD) en hombres con esclerosis múltiple (EM) se informa de forma diversa en diferentes estudios. La forma más común de SD en estos pacientes es la disfunción eréctil (DE). El objetivo de esta revisión sistemática y metanálisis es determinar la prevalencia combinada de SD y DE en hombres que padecen EM.
MétodosSe realizaron búsquedas en PubMed, Scopus, EMBASE, CINAHL, Web of Science y literatura gris (referencias de referencias y resúmenes de congresos) hasta el 14 de noviembre de 2020.
ResultadosEncontramos 3163 estudios por búsqueda primaria, 2246 permanecieron después de la eliminación de duplicados. Finalmente, 29 estudios fueron incluidos para metanálisis. Se evaluaron en total 3349 pacientes. La prevalencia combinada de SD fue del 66% (IC del 95%: 64%–69%). La prevalencia combinada de disfunción eréctil fue del 49% (IC del 95%: 47%–50%).
ConclusiónLa disfunción sexual es una complicación frecuente de la EM en pacientes masculinos que debe ser considerada por los médicos.
Multiple sclerosis (MS) is an autoimmune disease which affects individuals in reproductive age (mostly between 20–50 years of age) and causes a wide range of complications including sexual dysfunction (SD).1,2
Sexual dysfunction in MS may be divided into three categories: primary (due to disease course), secondary (due to fatigue, bowel dysfunction, spasticity), or tertiary (due to psychological complications such as depression),3–6 and interferes with quality of life.7 Signs and symptoms are widely different in patients and the location of the plaques plays an important role in SD development.8
Between 64–91% of men with MS suffer from SD and erectile dysfunction(ED) is the most frequent dysfunction (16%–92%).9
For clinicians, it is very important to consider SD in men and manage it to improve marital life and also the quality of life.8
Several studies have reported the prevalence of SD in men with MS. As there is no comprehensive study, we designed this systematic review and memeta-analysiso determine the pooled prevalence of SD and ED in men suffering from MS.
MethodsLiterature searchTwo independent researchers searched PubMed, Scopus, EMBASE, Web of Science, and Google Scholar as well as gray literature (references of references and conference abstracts) until 14th November 2020.
Inclusion criteriaWe included cross-sectional studies which reported SD and/or ED in men with MS.
Exclusion criteriaLetters to the editor, case-control, case reports, narrative reviews, and systematic reviews were excluded.
Data search and extractionThe search strategy included the MeSH and text keywords as ((Sclerosis[all] AND Multiple[all]) OR MS[all] OR “Multiple Sclerosis”[all]) AND ((Dysfunction[all] AND “Psychological Sexual”[all]) OR “Psychological Sexual Dysfunction”[all] OR “Psychosexual Dysfunctions”[all] OR “Psychosexual Disorders”[all] OR “Hypoactive Sexual Desire Disorder”[all] OR “Sexual Aversion Disorder”[all] OR “Orgasmic Disorder”[all] OR “Orgasmic Disorders”[all] OR “Sexual Arousal Disorder”[all] OR Frigidity[all] OR “Premature Ejaculation”[all] OR “Erectile Dysfunction”[all] OR Dyspareunia[all]).
Risk of bias assessmentWe evaluated the risk of potential bias with the NEWCASTLE - OTTAWA QUALITY ASSESSMENT SCALE(NOS) (adapted for cross-sectional studies).10
Statistical analysisAll statistical analyses were performed using STATA (Version 14.0; Stata Corp LP, College Station, TX, USA). We used the fixed-effects model.
To determine heterogeneity, inconsistency (I2) was calculated.
ResultsWe found 3163 studies by primary search. Of those, 2246 articles were screened after deletion of duplicates. Finally, twenty-nine studies were included in the meta-analysis. Twenty-three full texts and 6 conference abstracts were included (Fig. 1).
A total of 3349 patients were evaluated. Fourteen studies provided the frequency of cases with SD and 22 provided the frequency of men with ED.
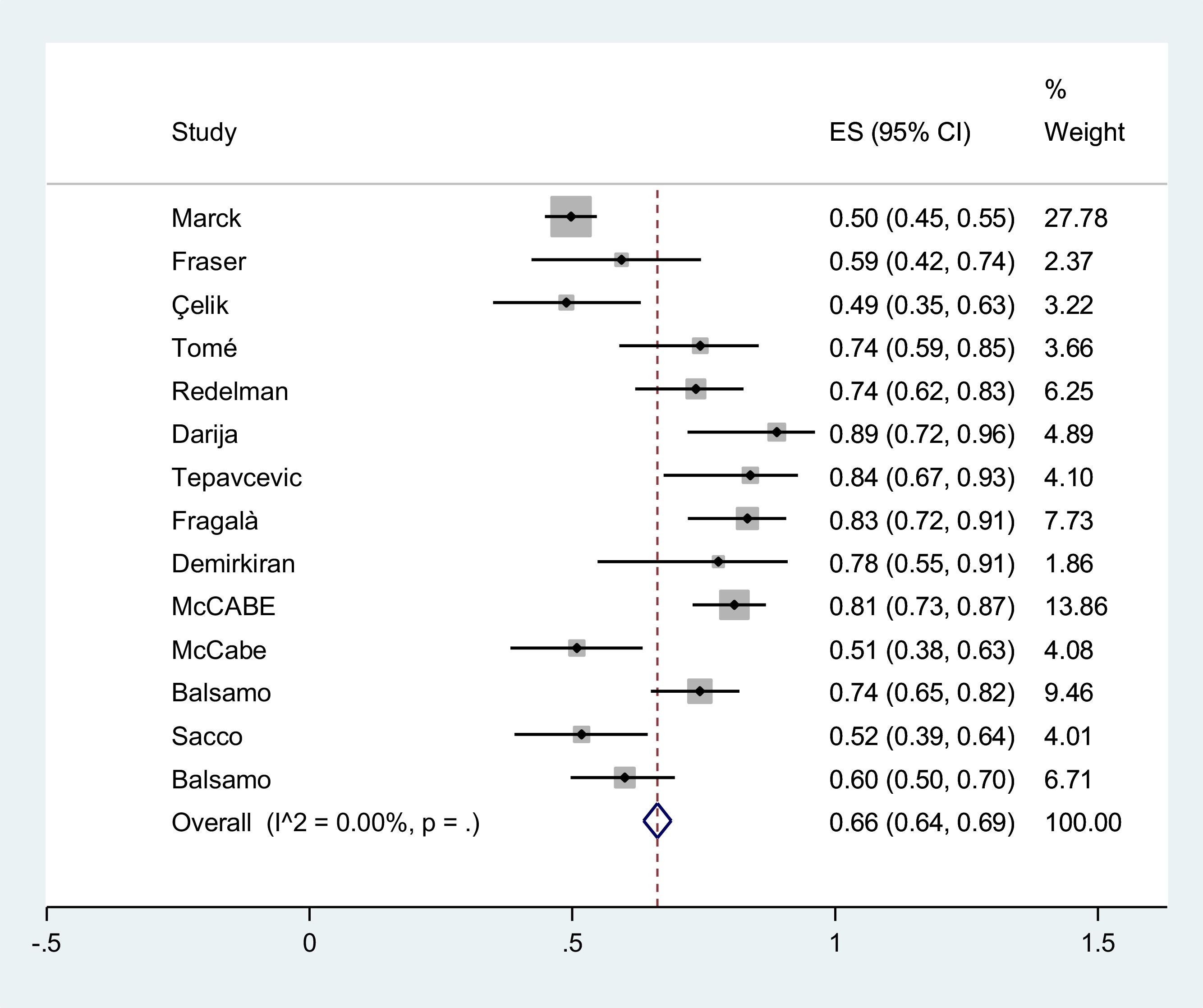
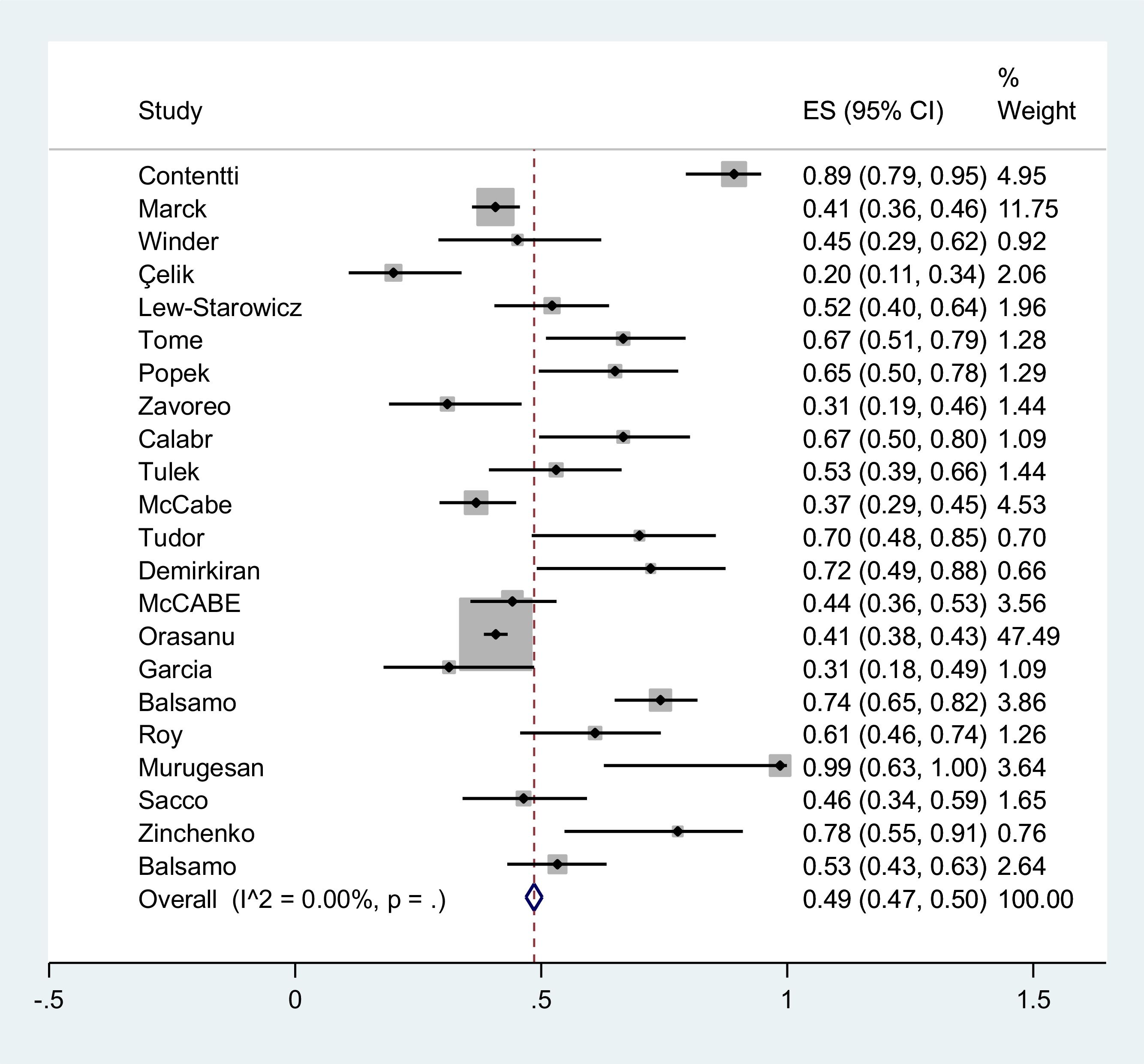
Basic characteristics of the studies are summarized in Table 1. The NOS ranged between 3 and 9 (Table 2). The pooled prevalence of SD estimated as 66% (95% CI: 64–69%) (I2=0) (Fig. 2). The pooled prevalence of erectile dysfunction estimated was 49% (95% CI: 47–50%) (I2=0)(Fig. 3).
Basic characteristics of the included studies.
| Title | Type of publication | Author | Year | Country | Sample size | MS Type | Mean age (SD) | Mean Disease duration (Mean±sd) or (Medianquartiles range) | Mean EDSS (SD) |
|---|---|---|---|---|---|---|---|---|---|
| Sexual dysfunction in patients with multiple sclerosis from Argentina: what are the differences between women and men?11 | Original article | Contentti et al. | 2019 | Argentina | 65 | RRMS=55PPMS=9SPMS=1 | 42.6 (9.7) | 7.5 (±0.6) | |
| Sexual function in multiple sclerosis and associations with demographic, disease and lifestyle characteristics: an international cross-sectional study12 | Original article | Marck et al. | 2016 | Australia | 388 | ||||
| Insular multiple sclerosis lesions are associated with erectile dysfunction13 | Original article | Winder et al. | 2018 | Germany | 31 | 38.2 (11.2) | 3.75±4.2 | 3.3 (2–4.4) | |
| Correlates of sexual dysfunction in men and women with multiple sclerosis5 | Original article | Fraser et al. | 2008 | US | 32 | 47 (8.9) | 6.9 (3.5) | ||
| Sexual dysfunction ın multiple sclerosis: Gender differences14 | Original article | Çelik et al. | 2012 | Turkey | 45 | ||||
| Sexual dysfunctions and sexual quality of life in men with multiple sclerosis7 | Original article | Lew-Starowicz et al. | 2014 | Poland | 67 | RRMS=25PPMS=30SPMS=8 | 49.9 (15.5) | 5.32 (2.11) | |
| Lower urinary tract symptoms and sexual dysfunction in men with multiple sclerosis15 | Original article | Tomé et al. | 2019 | Brazil | 39 | ||||
| Is multiple sclerosis only a neurological problem? Evaluation of sexual dysfunctions in a group of multiple sclerosis patients16 | Original article | Popek et al. | 2018 | Poland | 40 | ||||
| Sexual dysfunction and incidence of depression in multiple sclerosis patients17 | Original article | Zavoreo et al. | 2016 | Croatia | 42 | ||||
| Sexual function in young individuals with multiple sclerosis: does disability matter?18 | Original article | Calabrò et al. | 2018 | Italy | 33 | ||||
| Exploring sexual problems among patients with multiple sclerosis19 | Original article | Tulek et al. | 2011 | Turkey | 49 | ||||
| Relationship functioning and sexuality among people with multiple sclerosis20 | Original article | McCabe et al. | 2002 | Australia | 144 | 46.88 | |||
| Identifying barriers to help-seeking for sexual dysfunction in multiple sclerosis21 | Original article | Tudor et al. | 2018 | Croatia | 20 | ||||
| Sexual difficulties for persons with multiple sclerosis in New South Wales, Australia22 | Original article | Redelman et al. | 2009 | Australia | 68 | ||||
| Sexual dysfunction in multiple sclerosis: a 6-year follow-up study23 | Original article | Darija et al. | 2015 | Serbia | 27 | ||||
| The impact of sexual dysfunction on the quality of life measured by MSQoL-54 in patients with multiple sclerosis24 | Original article | Tepavcevic et al. | 2008 | Serbia | 31 | RRMS=19PPMS=5SPMS=7 | 41.6 (6.9) | 9.0 (5.1) | 4.2 (1.9) |
| Relationship between urodynamic findings and sexual function in multiple sclerosis patients with lower urinary tract dysfunction25 | Original article | Fragala et al. | 2014 | Italy | 60 | ||||
| Multiple sclerosis patients with and without sexual dysfunction: are there any differences?26 | Original article | Demirkiran et al. | 2006 | Turkey | 18 | ||||
| Changes over time in sexual and relationship functioning of people with multiple sclerosis27 | Original article | McCabe et al. | 2003 | Australia | 120 | 48.1 | |||
| Exacerbation of symptoms among people with multiple sclerosis: impact on sexuality and relationships over time28 | Original article | McCabe et al. | 2004 | Australia | 57 | ||||
| Determinants of sexual impairment in multiple sclerosis in male and female patients with lower urinary tract dysfunction: results from an Italian cross-sectional study29 | Original article | Fragalà et al. | 2014 | Italy | 60 | ||||
| Sexual dysfunction in patients with multiple sclerosis30 | Original article | Orasanu et al. | 2013 | US | 1568 | ||||
| Sexual dysfunction in male patients with multiple sclerosis31 | Conference abstract | Garcia et al. | 2016 | Spain | 32 | 35.4(6.4) | 6.9(5.4) | 1.2 (0–5) | |
| Increased risk of erectile dysfunction in men with multiple sclerosis: an Italian cross-sectional study8 | Original article | Balsamo et al. | 2017 | Italy | 101 | RRMS=64PPMS=28SPMS=9 | 41.26 (11.6) | 11.5 (7.5) | 3.77 (2.01) |
| Depression influences erectile dysfunction in multiple sclerosis patients with primary and tertiary sexual dysfunction32 | Conference abstract | Roy et al. | 2018 | Germany | 41 | 29.3 (29.3–42.5) | |||
| A study of sexual dysfunction and awareness on its rehabilitation measures in multiple sclerosis33 | Conference abstract | Mulanur Murugesan et al. | 2018 | India | 7 | ||||
| Sexual dysfunctions in patients affected by multiple sclerosis: evaluation in a contemporary cohort from a referral center34 | Conference abstract | Sacco et al. | 2011 | Italy | 56 | ||||
| Sexual dysfunction in young men with relapsing-remitting multiple sclerosis35 | Conference abstract | Zinchenko et al. | 2010 | United Kingdom | 18 | RRMS=18 | 30.8 (4.3) | ||
| Determinants of sexual dysfunctions and sexual quality of life in men with multiple sclerosis36 | Conference abstract | Balsamo et al. | 2016 | Italy | 90 | 40 (20–64) |
RRMS: relapsing-remitting multiple sclerosis; PPMS: primary-progressive multiple sclerosis; SPMS: secondary-progressive multiple sclerosis.
Number of patients with SD and ED.
| NOS score | Number of patients with erectile dysfunction | Number of patients with Sexual dysfunction | Sexual test | Author | Title |
|---|---|---|---|---|---|
| 8 | 58 | Multiple Sclerosis Intimacy and Sexuality Questionnaire (MSISQ-19) | Contentti et al. | Sexual dysfunction in patients with multiple sclerosis from Argentina: what are the differences between women and men? | |
| International Index of Erectile Function (IIEF5-ED) | |||||
| 9 | 158 | 193 | Sexual function scale | Marck et al. | Sexual function in multiple sclerosis and associations with demographic, disease and lifestyle characteristics: an international cross-sectional study |
| satisfaction item | |||||
| 7 | 14 | IIEF5 | Winder et al. | Insular multiple sclerosis lesions are associated with erectile dysfunction | |
| MSISQ-19 | |||||
| 3 | 19 | The Guy’s Neurological Disability Scale (GNDS) | Fraser et al. | Correlates of sexual dysfunction in men and women with multiple sclerosis | |
| 7 | 9 | 22 | MSISQ scores | Çelik et al. | Sexual dysfunction ın multiple sclerosis: gender differences |
| 8 | 35 | IIEF | Lew-Starowicz et al. | Sexual dysfunctions and sexual quality of life in men with multiple sclerosis | |
| Sexual Quality of Life Questionnaire—Male Version (SQoL-M) | |||||
| 7 | 26 | 29 | IIEF-15 | Tomé et al. | Lower urinary tract symptoms and sexual dysfunction in men with multiple sclerosis |
| 7 | 26 | IIEF | Popek et al. | Is multiple sclerosis only a neurological problem? Evaluation of sexual dysfunctions in a group of multiple sclerosis patients | |
| 6 | 13 | Sexual Satisfaction Scale, SSS | Zavoreo et al. | Sexual dysfunction and incidence of depression in multiple sclerosis patients | |
| 3 | 22 | Interview and 40-item questionnaire | Calabrò et al. | Sexual function in young individuals with multiple sclerosis: does disability matter? | |
| 2 | 26 | 5-item questionnaire | Tulek et al. | Exploring sexual problems among patients with multiple sclerosis | |
| 5 | 53 | Nature of the Sexual Problem Subscale of the Sexual Dysfunction Scale (SDS) | McCabe et al. | Relationship functioning and sexuality among people with multiple sclerosis | |
| Sexual Activity Subscale of the Sexual Function Scale (SFS) | |||||
| 5 | 14 | Arizona Sexual Experiences Scale (ASEX) | Tudor et al. | Identifying barriers to help-seeking for sexual dysfunction in multiple sclerosis | |
| MSISQ | |||||
| 5 | 50 | 28-item questionnaire | Redelman et al. | Sexual difficulties for persons with multiple sclerosis in New South Wales, Australia | |
| 7 | 8(loss) | 24 | 16-item questionnaire | Darija et al. | Sexual dysfunction in multiple sclerosis: a 6-year follow-up study |
| 18 (incomplete) | Szasz sexual functioning scale | ||||
| 7 | 7(loss) | 26 | 16-item questionnaire | Tepavcevic et al. | The impact of sexual dysfunction on the quality of life measured by MSQoL-54 in patients with multiple sclerosis |
| 16(incomplete) | Szasz sexual functioning scale | ||||
| 7 | 50 | IIEF15 | Fragala et al. | Relationship between urodynamic findings and sexual function in multiple sclerosis patients with lower urinary tract dysfunction | |
| MSISQ | |||||
| 6 | 13 | 14 | (MSISQ-19) | Demirkiran et al. | Multiple sclerosis patients with and without sexual dysfunction: are there any differences? |
| 8 | 53 | 97 | Index of Sexual Satisfaction (ISS) | McCabe et al. | Changes over time in sexual and relationship functioning of people with multiple sclerosis |
| Sexual Dysfunction Scale (SDS) | |||||
| Sexual Function Scale (SFS) | |||||
| 6 | 29 | Index of Sexual Satisfaction (ISS) | McCabe et al. | Exacerbation of symptoms among people with multiple sclerosis: impact on sexuality and relationships over time | |
| Sexual Function Scale (SFS) | |||||
| e Sexual Dysfunction Scale (SDS) | |||||
| 8 | 50 | IIEF-15 | Fragalà et al. | Determinants of sexual impairment in multiple sclerosis in male and female patients with lower urinary tract dysfunction: results from an Italian cross-sectional study | |
| FSFI | |||||
| MSISQ19 | |||||
| 7 | 639 | MSISQ-19 | Orasanu et al. | Sexual dysfunction in patients with multiple sclerosis | |
| 10 | MSISQ-19 | Garcia et al. | Sexual dysfunction in male patients with multiple sclerosis | ||
| IIEF | |||||
| 7 | 75 | 75 | IIEF-15 | Balsamo et al. | Increased risk of erectile dysfunction in men with multiple sclerosis: an Italian cross-sectional study |
| 25 | IIEF-5 | Roy et al. | Depression influences erectile dysfunction in multiple sclerosis patients with primary and tertiary sexual dysfunction | ||
| MSISQ-19 | |||||
| 7 | IIEF-5 | Mulanur Murugesan et al. | A Study of sexual dysfunction and awareness on its rehabilitation measures in multiple sclerosis | ||
| 26 | 29 | IIEF | Sacco et al. | Sexual dysfunctions in patients affected by multiple sclerosis: evaluation in a contemporary cohort from a referral center | |
| 14 | IIEF | Zinchenko et al. | Sexual dysfunction in young men with relapsing remitting-multiple sclerosis | ||
| MSISQ-19 | |||||
| 48 | 54 | IIEF-15 | Balsamo et al. | Determinants of sexual dysfunctions and sexual quality of life in men with multiple sclerosis |
MSISQ-19: multiple sclerosis intimacy and sexuality questionnaire ;IIFE5: international index of erectile function ; GNDS: the guy’s neurological disability scale; SQoL-M: sexual quality of life questionnaire; SSS: sexual satisfaction scale; SDS: sexual dysfunction scale; SFS: sexual function scale; ASEX: Arizona sexual experiences scale; ISS: index of sexual satisfaction.
To our knowledge, this is the first systematic review and meta-analysis evaluating SD and ED in men with MS. Our results demonstrated that the pooled prevalence of SD in men with MS was 66% and the pooled prevalence of ED was 49%.
The prevalence of SD in the included studies ranged between 49% and 89% which could be due to different inclusion and exclusion criteria, different applied tests, and different sample sizes.
Men with MS suffer from deterioration in their sexual life affecting their marital life, which is ignored in most cases. Neither physicians nor patients talk about this issue in most clinical settings. There are controversies regarding the role of some factors (including age, disease duration, and disability) in developing SD in men with MS.7,37
Zorzon et al. found that SD is more common in men with MS than patients with other chronic diseases (including rheumatoid arthritis, systemic lupus erythematosus, psoriatic arthritis, and ankylosing spondylitis) as well as healthy controls.38
In another study, Marck et al. evaluated 388 men with MS and reported SD in 49.7%. They found that difficulty in erection was the most frequent problem.12 Their results also showed that fatigue, depression and antidepressant use were independent predictors of SD.
Lew-Starowicz and Rola reported ED as the most common form of SD in men with MS (52.9%). They also investigated that age, disease duration and disability were not related with the incidence or severity of SD.7
It should be noted that ED affects sexual satisfaction and sexual self-esteem7 and ED diagnosis and treatment would improve marital life and overall quality of life.
In healthy men, the sexual response cycle includes libido, erection, ejaculation and orgasm.39 Men with MS may suffer from ejaculatory dysfunction and/ or orgasmic dysfunction, ejaculatory dysfunction and/or orgasmic dysfunction, and anorgasmia. 40 Despite its importance, Lew-Starowicz reported that only 6% of their patients discussed their sexual concerns with their physicians or received treatment for this problem.7
Sexual dysfunction is an important issue for patients with MS. Most patients are young and in reproductive age. SD influences mental health, quality of life and intimate relationships, but is not routinely evaluated.12 Asking a few questions as well as applying suitable questionnaires could help physicians to detect and treat SD. The International Index of Erectile Function is widely used for ED detection.
Sexual dysfunction in MS can be a direct result of neurological changes due to MS which is known as primary SD, or the consequence of medication use (medications which are applied for fatigue, bladder and bowel dysfunctions, spasms, and pain) which is known as secondary SD, or tertiary SD which is the result of psychological complications such as depression, anxiety, decreased self-esteem, fear of being sexually rejected, and body image perception distortion.40,41
Modification of some factors such as smoking cessation, depression and fatigue treatment, and increased physical activity could help improve SD.12
This systematic review has several strengths. First, it included 29 studies which used different tests. Second, studies are from different nations.
ConclusionSexual dysfunction is a prevalent complication of MS in male patients which should be considered by clinicians.
Ethics approval and consent to participateAll participants filled informed consent forms. All methods were carried out in accordance with relevant guidelines and regulations. All experimental protocols were approved by local ethics committee.
Consent for publicationAll authors consent for publication.
Availability of data and materialsThe datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing interestsThe authors had no conflicts of interest.
FundingWe had no funding.
Authors’ contributionVS: Study conception, data gathering article writing
OM: Data gathering, article writing
SV: Data gathering, article writing
NN: Data gathering, article writing
MG: Study design, data analysis, article writing
None.