Thunderclap headache is a high-intensity headache of sudden onset which reaches its peak in less than one minute and lasts a minimum of 5minutes.1 Thunderclap headache may be caused by numerous factors, including some severe vascular intracranial disorders associated with high morbidity and mortality. Early assessment with imaging techniques and a lumbar puncture is therefore essential.2,3 Pneumocephalus is a rare cause of thunderclap headache. This condition is characterised by presence of intracranial gas, usually resulting from a connection between the intracranial and extracranial spaces following surgery, head trauma, or tumours; less frequent causes include non-surgical invasive procedures such as epidural anaesthesia using the ‘loss of resistance to air’ (LORA) technique.4 Pneumocephalus manifests clinically as headache of severe intensity, but sudden onset is rare. When headache does start abruptly, differential diagnosis should be performed to rule out other entities that may present similarly to thunderclap headache.3,5
We present the case of a 27-year-old primiparous woman with no relevant medical history who experienced holocranial thunderclap headache 2 days after vaginal delivery with epidural block; pain did not respond to traditional analgesics or caffeine. Pain was oppressive, sudden-onset, and severe in intensity, and exacerbated with horizontal posture. She presented no vomiting or visual disturbances. The general and neurological examinations revealed no abnormalities and no meningeal signs.
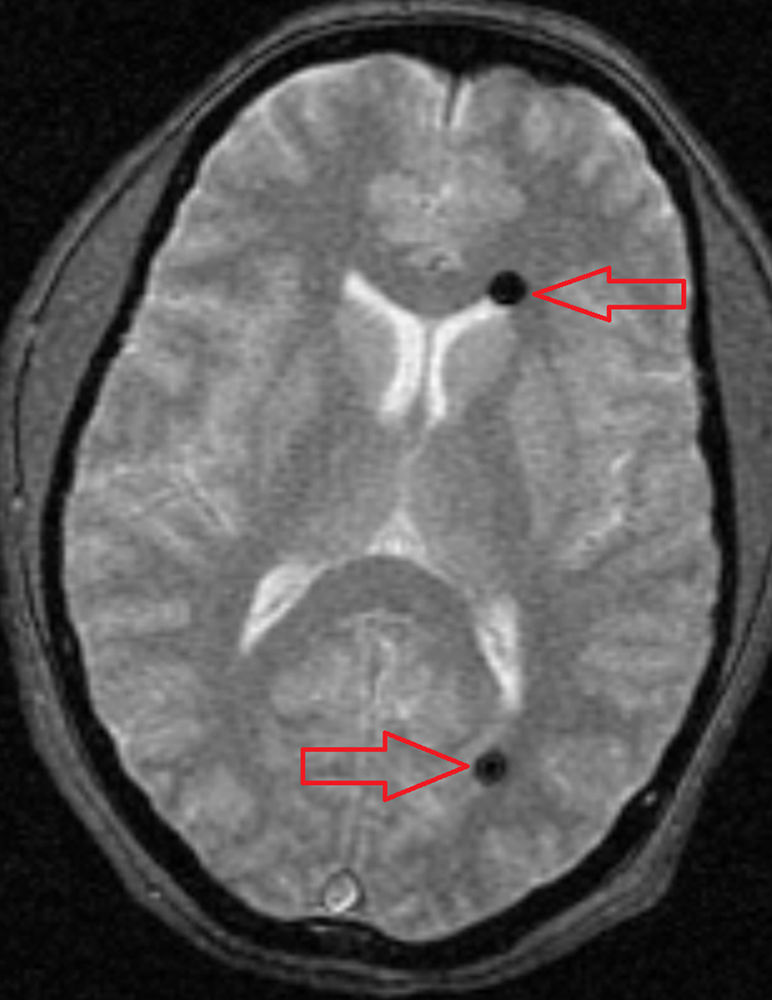
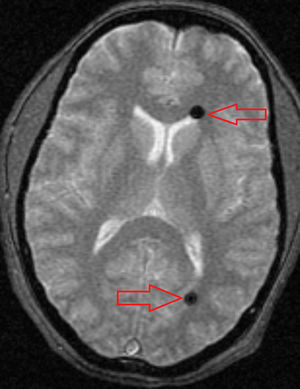
CT and MR images revealed 2 round shapes, located in the anterior and posterior areas of the left lateral ventricle, which were compatible with air bubbles (Figs. 1 and 2). MRI angiography of the intracranial vessels ruled out aneurysms, arteriovenous malformations, vertebral or internal carotid artery dissection, and venous sinus thrombosis. Our patient was diagnosed with thunderclap headache due to pneumocephalus secondary to an epidural block using the LORA technique. She received conservative treatment with analgesics and rest; symptoms resolved in a few days.
Published cases of thunderclap headache due to pneumocephalus secondary to epidural anaesthesia using the LORA technique are exceptional,6 especially late-onset cases. This is a rare complication of accidental dural puncture resulting from air entering the subdural or subarachnoid spaces and then migrating towards the brain. Two different types of headache have been associated with this technique: headache secondary to pneumocephalus and low CSF pressure headache.7 The first of these usually manifests immediately after puncture or when the patient resumes a standing position. In our case, the onset of headache 2 days after epidural block was probably triggered by a postural change from lying to standing and caused by an air bubble in the subarachnoid space having migrated to the cranial cavity. Low CSF pressure headache has been reported as a consequence of accidental dural puncture as well as a cause of thunderclap headache, and an orthostatic factor is typically involved. Brain MRI scans in patients with low CSF pressure frequently indicate extradural CSF collection, diffuse meningeal uptake, engorgement of venous structures, pituitary hyperaemia, and downward displacement of the brain.8 None of these signs were seen in our patient, making it unlikely that intracranial hypotension would be the cause of headache. Our patient did not undergo a lumbar puncture since neuroimaging studies revealed pneumocephalus as a possible cause of thunderclap headache. However, differential diagnosis of all the possible aetiologies of thunderclap headache is absolutely essential to rule out such severe entities as subarachnoid haemorrhage, other intracranial haemorrhages, cerebral venous thrombosis, cervical artery dissection, and reversible cerebral vasoconstriction syndrome. All patients with these headaches should undergo cranial CT and lumbar puncture, plus brain MRI and MRI angiography in selected cases.9
Such underlying processes as pneumocephalus and CSF hypovolaemia should be ruled out in patients experiencing thunderclap headache after undergoing an invasive procedure (for example, epidural anaesthesia with the LORA technique). This case and other published cases support using the ‘loss of resistance to saline’ technique to identify the epidural space. This method has been found to provide better analgesia with fewer adverse effects compared to the LORA technique.
FundingThis study received no funding of any kind.
Please cite this article as: Arenaza-Basterrechea N, Iglesias Díez F, López Sarnago P. Cefalea en trueno secundaria a neumoencéfalo. Neurología. 2017;32:132–133.
This study was presented in poster format in the headache section at the 66th Annual Meeting of the Spanish Society of Neurology.