Dear Editor
Heat stroke is a medical emergency1–4 characterised by a systemic inflammatory response secondary to an increase in body temperature above 40 °C, with severe multiple organ involvement, including the central nervous system (CNS), which is particularly vulnerable to hyperthermia.1–3,5–7 Heat stroke may be fatal or cause irreversible lesions. Though infrequent, its incidence is expected to increase due to the increasing frequency of heat waves.
Few imaging data on CNS involvement in heat stroke are available, and the published data are mainly from case reports that describe a range of supratentorial lesions; although no specific imaging findings of heat stroke have been described, cerebellar atrophy is frequently reported.1–9
We present the case of a 61-year-old man with history of arterial hypertension who was admitted to the emergency department during a heat wave due to reduced level of consciousness (5/15 on the Glasgow Coma Scale), with a body temperature of 43 °C.
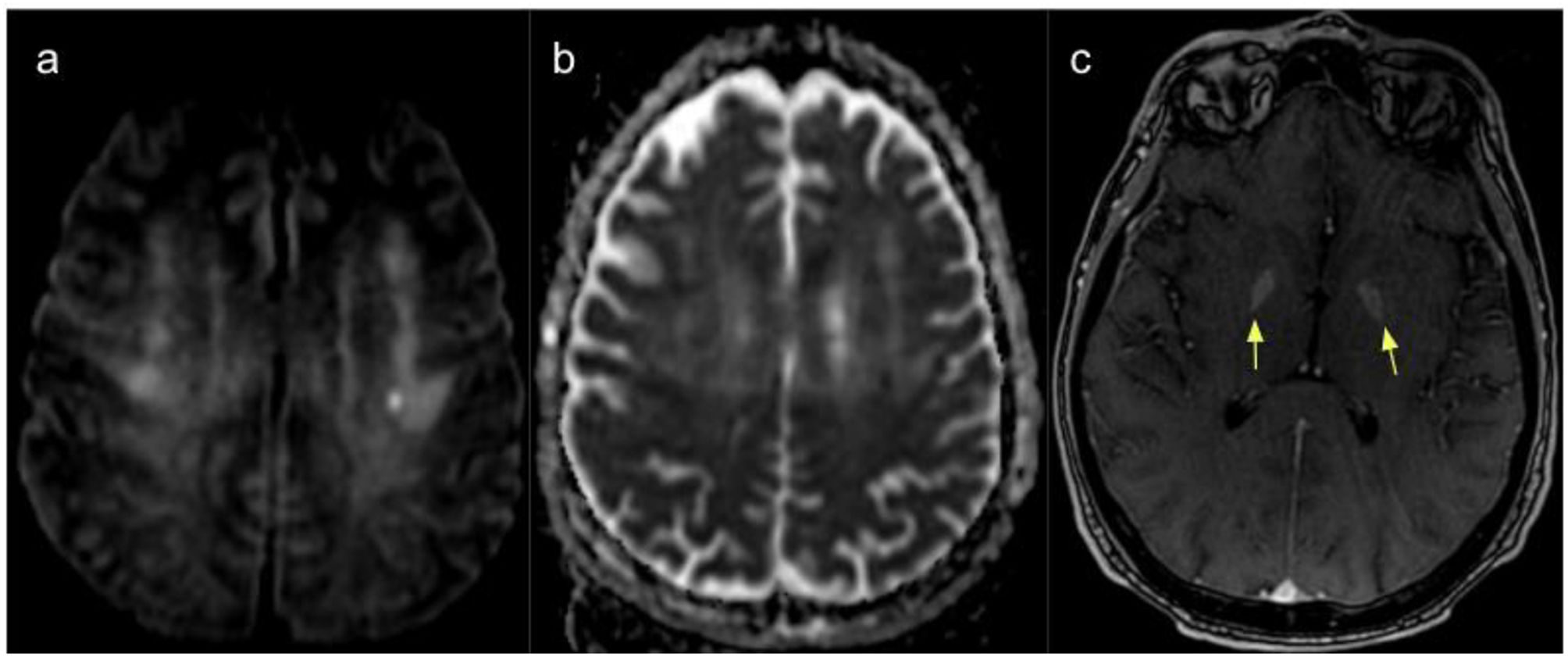
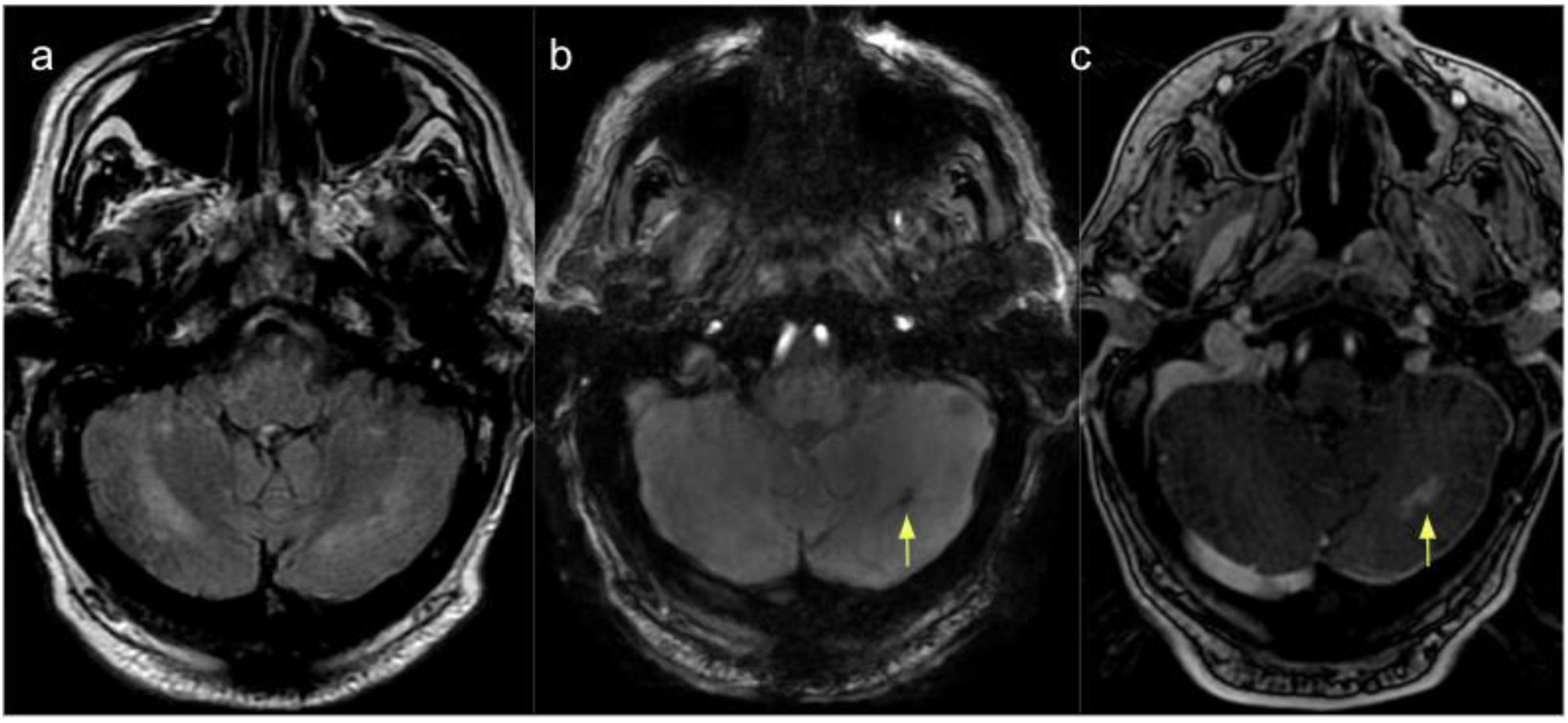
A CT scan revealed no alterations; however, as neurological symptoms persisted at 10 days after admission, he underwent a brain MRI scan, which revealed hyperintensities on T2-weighted sequences in both cerebellar hemispheres (dentate nuclei), particularly on the right side, with restricted diffusion on DWI sequences. We also observed a hyperintense focus in the left corona radiata, with diffusion restriction on diffusion sequences and a small area of blood deposition in the left cerebellar hemisphere. Post-contrast sequences revealed contrast uptake in the cerebellar lesions and globi pallidi (Figs. 1 and 2).
MRI scan of the cerebellum. (A) T2-weighted FLAIR sequence showing hyperintense lesions in the cerebellar hemispheres (dentate nuclei), predominantly on the right side, coinciding with areas of diffusion restriction on DWI sequences (image not displayed). (B) SWAN sequence showing a haemorrhagic focus in the left cerebellum. (C) Contrast T1-weighted sequence revealing foci of increased contrast uptake in the left cerebellum.
These findings are compatible with ischaemic and haemorrhagic processes in the context of heat stroke.
The patient died 14 days after admission due to limitation of therapeutic effort.
The pathophysiological mechanism of CNS damage and the related imaging findings is not well established, but is believed to be multifactorial,2,3,5,8 involving lesions secondary to direct thermal injury, as in the case of destruction of cerebellar Purkinje cells, as well as alterations in brain perfusion, with vasodilation, potentially leading to brain oedema, and subsequent vasoconstriction secondary to hypovolaemia, causing ischaemic damage and microvascular alterations similar to those occurring in disseminated intravascular coagulation, in association with brain haemorrhages.2,5–8
Previously reported imaging findings include bilateral lesions to the external capsule,1,6,8,9 the posterior limb of the internal capsule,6 splenium,2,5,9 basal ganglia,2,6,8,9 thalamus,1,9 and hippocampus,3,8,9 in addition to patchy lesions to the frontal and parietal cortex,9 insula,6 and subcortical white matter.2 These lesions are hypointense on T1-weighted sequences and hyperintense on T2-weighted, FLAIR, and DWI sequences.
Heat stroke has also been reported to cause cerebral venous thrombosis.6
Most published cases describe cytotoxic oedema at various supratentorial locations2,4,5,8,9 and diffuse cerebellar atrophy in studies performed at 90 days after the acute event.7–9
The largest series of patients undergoing MRI studies was published by Shimada et al.5 in 2019, with a review of 22 previously published cases plus 2 new cases. The authors classified MRI findings as infarction-like lesions (29.1%) or posterior reversible encephalopathy syndrome-like lesions (87.5%), due to the pathophysiological similarities and associated vascular regulation alterations; 4 patients presented both types of MRI lesions.
The interest of our case lies in the rarity of the clinical presentation and the presence of the classic cerebellar lesions, particularly lesions to the dentate nuclei (secondary to Purkinje cell destruction) with blood deposition, in addition to lesions to the corona radiata and basal nuclei, which showed contrast uptake; these findings are compatible with current theories on the pathophysiology of the condition as an ischaemic or haemorrhagic process.
The initial CT scan of patients with heat stroke usually detects no abnormalities,7 or only indirect signs of brain oedema4; however, CT is performed in the majority of cases to rule out potentially treatable lesions. Patients with persistent neurological symptoms may be assessed with MRI, with T2-weighted or FLAIR sequences to evaluate ischaemic or haemorrhagic small-vessel lesions and DWI and ADC sequences to detect cytotoxic oedema, which is linked to irreversible neuronal damage. Contrast-enhanced sequences reveal blood–brain barrier disruption secondary to vascular and/or inflammatory processes.
The clinical manifestations of the condition are highly variable. Most published cases describe altered level of consciousness in the acute phase, with subsequent recovery, as well as persistent, severe neurological sequelae,1,5–8 which may be explained by MRI findings.
FundingThis study has received no specific funding from any public, private, or non-profit organisation.
The authors observed their centre's protocols for the publication of patient data. The patient gave informed consent for the publication of this case report.