The World Health Organization defines the multisystem inflammatory syndrome in children (MIS-C) as a new syndrome reported in patients aged <19 years old who have a history of exposure to SARS-CoV-2. The onset of this syndrome is characterized by persistent fever that is associated with lethargy, abdominal pain, vomiting and/or diarrhea, and, less frequently, rash and conjunctivitis. The course and severity of the signs and symptoms vary; in some children, MIS-C worsens rapidly and can lead to hypotension, cariogenic shock, or even damage to multiple organs. The characteristic laboratory findings are elevated markers of inflammation and heart dysfunction. The most common radiological findings are cardiomegaly, pleural effusion, signs of heart failure, ascites, and inflammatory changes in the right iliac fossa. In the context of the current COVID-19 pandemic, radiologists need to know the clinical, laboratory, and radiological characteristics of this syndrome to ensure the correct diagnosis.
El síndrome inflamatorio multisistémico pediátrico vinculado a la COVID-19 (SIM-PedS) es, según la Organización Mundial de la Salud, un nuevo síndrome descrito en pacientes menores de 19 años con historia previa de exposición a SARS-CoV-2. La presentación inicial de este síndrome se caracteriza por fiebre persistente que asocia debilidad, dolor abdominal, vómitos y/o diarrea. Menos frecuentemente los pacientes pueden presentar también erupción cutánea y conjuntivitis. El cuadro clínico tiene expresividad y evolución variables, por lo que algunos pacientes pediátricos afectados pueden empeorar rápidamente, desarrollando desde hipotensión y shock cardiogénico a daño multiorgánico. Los hallazgos analíticos característicos del síndrome consisten en elevación de marcadores inflamatorios y disfunción cardíaca. Los hallazgos radiológicos más frecuentes son cardiomegalia, derrame pleural, signos de insuficiencia cardíaca, ascitis y cambios inflamatorios en la fosa ilíaca derecha. En la pandemia actual por COVID-19 es necesario que el radiólogo conozca las características clínico-analíticas y radiológicas de este síndrome para realizar un correcto diagnóstico.
In December 2019, an outbreak of a new coronavirus was reported in Wuhan, Hubei province, China. On 11 February, 2020, the World Health Organization (WHO) renamed the new virus SARS-CoV-2, due to its similarity to the cause of the severe acute respiratory syndrome that broke out in 2003, and the new disease COVID-19 (Coronavirus Infectious Disease 2019). On 11 March, 2020, the WHO declared the outbreak a pandemic.1
Since then, COVID-19 has been described as a disease that affects the paediatric population less than the adult population, both in incidence and severity, with a milder clinical picture and a rapid subsequent recovery in the vast majority of children.2,3 Studies suggest that children have a lower viral load,4 so that while 18.5% of adults with COVID-19 have severe disease, only between 6% and 8% of children present severe symptoms.5–7 The data indicate that 45% of paediatric patients are asymptomatic,8 and when they do show symptoms their most common manifestation is fever in 95%–98% of cases and cough in 86%–95%.9–11 Since April 2020, when the COVID-19 pandemic was already widespread in Western countries, more and more cases of children who have developed a multisystem hyper-inflammatory syndrome associated with SARS-CoV-2 infection have been documented. Most of these patients had IgG antibodies against SARS-CoV-2, with a negative PCR result,12–18 that is, laboratory findings that demonstrate that the infection has been overcome.
Affected patients presented a wide spectrum of clinical findings consisting of fever (38–40 °C), headache and pain in limbs; abdominal pain, vomiting and diarrhoea; skin rash, conjunctivitis and peripheral oedema, with variable severity, with a significant percentage evolving to myocardial damage and cardiogenic, septic or toxic shock.18–23 Laboratory test abnormalities were similar to those observed in Kawasaki disease (KD), toxic shock syndrome (TSS), or macrophage activation syndrome, although more severe.18,19
This systemic inflammatory syndrome of variable expressiveness has been given several names. In the UK/Europe, it has been called “paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2” (PMIS-TS)24 and in the USA, SARS-CoV-2-related multisystem inflammatory syndrome in children (MIS-C),25 coinciding with the name given by the WHO.26 The recent consensus document of the Asociación Española de Pediatría (AEP) [Spanish Paediatric Association] has decided to refer to it as “síndrome inflamatorio multisistémico pediátrico vinculado a SARS-CoV-2” or SIM-PedS [paediatric multisystem inflammatory syndrome associated with SARS-CoV-2].18
In Spain, the paediatric age group is considered to be up to 15 years of age, although several official bodies such as the WHO and the US Centers for Disease Control and Prevention (CDC) have included patients younger than 19 and 21 years, respectively,25,26 in their criteria and some studies also include patients older than 15 years.19 Therefore, the authors propose to consider this syndrome not only in children under 15 years of age, who can be cared for by a paediatrician or paediatric radiologist, but also in patients between 15 and 20 years, who will be evaluated by family or emergency physicians and general radiologists or those not specifically dedicated to paediatric radiology. Since the clinical manifestation of SIM-PedS is nonspecific, imaging tests play a very important role in its diagnosis. This article reviews the clinical and radiological findings of this new syndrome.
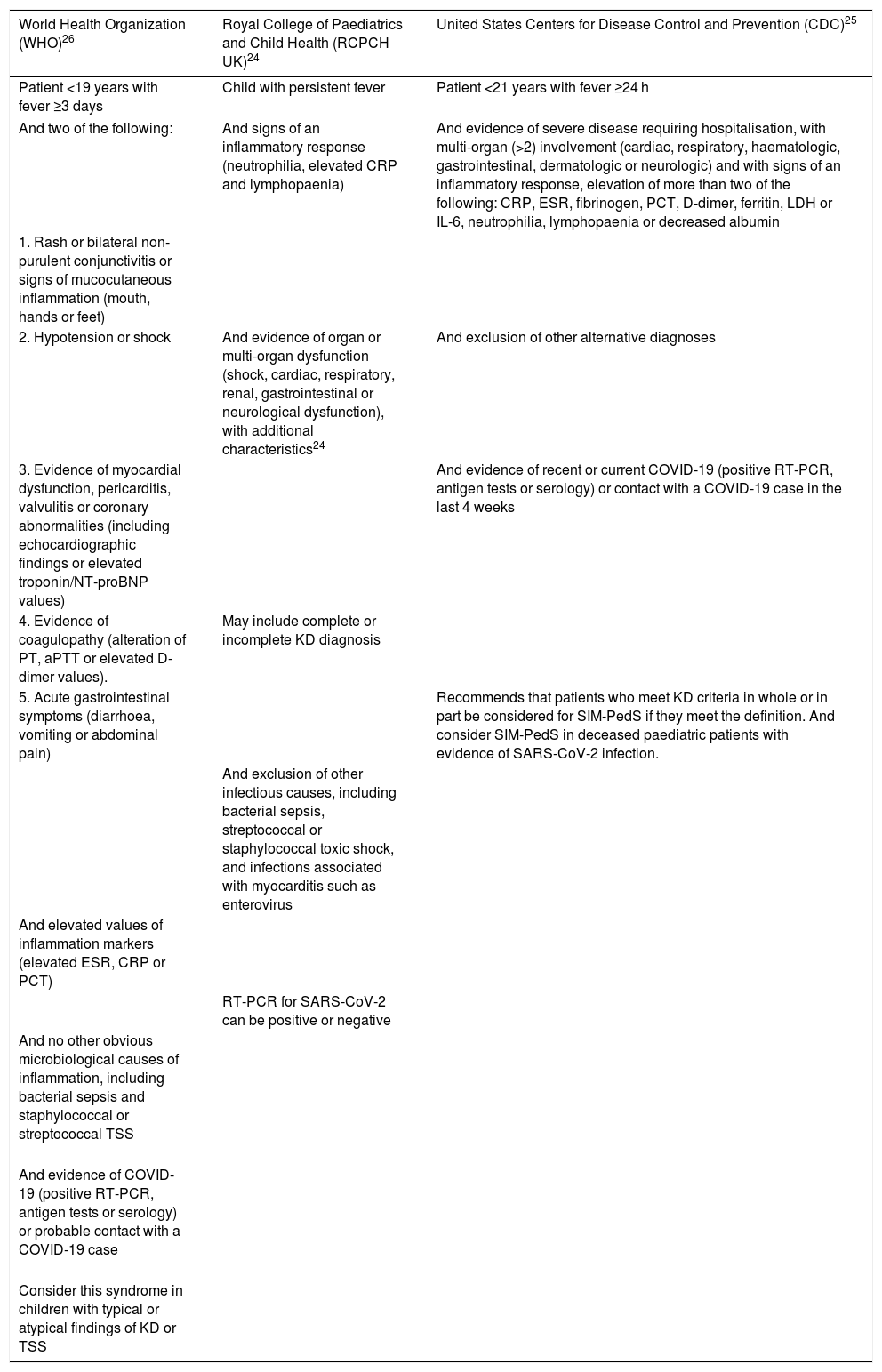
Definitions and clinical-analytical findingsThe inclusion criteria defined by the different health organisations mentioned above to establish the diagnosis of SIM-PedS show slight differences and are summarised in Table 1.
Definitions of SIM-PedS by WHO, RCPCH, CDC.
| World Health Organization (WHO)26 | Royal College of Paediatrics and Child Health (RCPCH UK)24 | United States Centers for Disease Control and Prevention (CDC)25 |
|---|---|---|
| Patient <19 years with fever ≥3 days | Child with persistent fever | Patient <21 years with fever ≥24 h |
| And two of the following: | And signs of an inflammatory response (neutrophilia, elevated CRP and lymphopaenia) | And evidence of severe disease requiring hospitalisation, with multi-organ (>2) involvement (cardiac, respiratory, haematologic, gastrointestinal, dermatologic or neurologic) and with signs of an inflammatory response, elevation of more than two of the following: CRP, ESR, fibrinogen, PCT, D-dimer, ferritin, LDH or IL-6, neutrophilia, lymphopaenia or decreased albumin |
| 1. Rash or bilateral non-purulent conjunctivitis or signs of mucocutaneous inflammation (mouth, hands or feet) | ||
| 2. Hypotension or shock | And evidence of organ or multi-organ dysfunction (shock, cardiac, respiratory, renal, gastrointestinal or neurological dysfunction), with additional characteristics24 | And exclusion of other alternative diagnoses |
| 3. Evidence of myocardial dysfunction, pericarditis, valvulitis or coronary abnormalities (including echocardiographic findings or elevated troponin/NT-proBNP values) | And evidence of recent or current COVID-19 (positive RT-PCR, antigen tests or serology) or contact with a COVID-19 case in the last 4 weeks | |
| 4. Evidence of coagulopathy (alteration of PT, aPTT or elevated D-dimer values). | May include complete or incomplete KD diagnosis | |
| 5. Acute gastrointestinal symptoms (diarrhoea, vomiting or abdominal pain) | Recommends that patients who meet KD criteria in whole or in part be considered for SIM-PedS if they meet the definition. And consider SIM-PedS in deceased paediatric patients with evidence of SARS-CoV-2 infection. | |
| And exclusion of other infectious causes, including bacterial sepsis, streptococcal or staphylococcal toxic shock, and infections associated with myocarditis such as enterovirus | ||
| And elevated values of inflammation markers (elevated ESR, CRP or PCT) | ||
| RT-PCR for SARS-CoV-2 can be positive or negative | ||
| And no other obvious microbiological causes of inflammation, including bacterial sepsis and staphylococcal or streptococcal TSS | ||
| And evidence of COVID-19 (positive RT-PCR, antigen tests or serology) or probable contact with a COVID-19 case | ||
| Consider this syndrome in children with typical or atypical findings of KD or TSS | ||
aPTT: activated partial thromboplastin time; CRP: C-reactive protein; ESR: erythrocyte sedimentation rate; IL-6: interleukin 6; KD: Kawasaki disease; PCT: procalcitonin; PT: prothrombin time; TSS: toxic shock syndrome.
As commented above, SIM-PedS is a syndrome described in relation to COVID-19, therefore this new disease should be considered in areas with a high current or recent incidence of COVID-19. Unlike adult COVID-19, which initially presents with respiratory symptoms and pneumonia, SIM-PedS typically manifests with multi-organ damage, predominantly affecting the cardiovascular system. The onset of SIM-PedS is characterised by persistent fever, which is often associated with gastrointestinal weakness and symptoms. Less commonly, patients may also present with a skin rash, conjunctivitis and other mucocutaneous manifestations.
It has been reported that some affected paediatric patients may show rapid worsening with onset of hypotension, cardiogenic shock and multi-organ damage. The time interval between the first symptoms and these serious cardiovascular manifestations is approximately one week.12–15,18,27
Given the similarity between the various forms of KD and SIM-PedS, and the pandemic context in which we find ourselves, it is recommended that in patients who meet criteria for the various KD variants (classic or complete, incomplete or KD with shock) to consider evaluating a possible diagnosis of SIM-PedS.18,28,29 As a brief reminder, KD is a systemic autoimmune disease characterised by a systemic inflammation of the medium-calibre arteries during the acute febrile phase. It usually affects children under 5 years of age, with the appearance of dilatation or coronary aneurysms being a predominant and characteristic finding.28
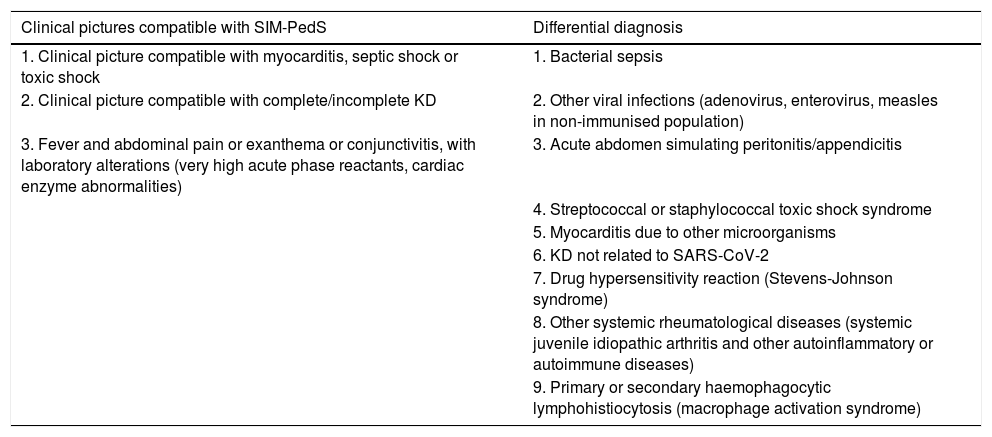
The laboratory findings characteristic of SIM-PedS consist of elevation of inflammatory markers (CRP, ESR, ferritin, fibrinogen, LDH, IL-6), cardiac dysfunction (NT-ProBNP, enzymes), D-dimer and transaminases; hyponatraemia and hypoalbuminaemia.12,16,18 The clinical pictures that could be compatible and the differential diagnosis proposed by the AEP are shown in Table 2.
Clinical pictures compatible with SIM-PedS and differential diagnosis proposed by the Asociación Española de Pediatría in its consensus document.18
| Clinical pictures compatible with SIM-PedS | Differential diagnosis |
|---|---|
| 1. Clinical picture compatible with myocarditis, septic shock or toxic shock | 1. Bacterial sepsis |
| 2. Clinical picture compatible with complete/incomplete KD | 2. Other viral infections (adenovirus, enterovirus, measles in non-immunised population) |
| 3. Fever and abdominal pain or exanthema or conjunctivitis, with laboratory alterations (very high acute phase reactants, cardiac enzyme abnormalities) | 3. Acute abdomen simulating peritonitis/appendicitis |
| 4. Streptococcal or staphylococcal toxic shock syndrome | |
| 5. Myocarditis due to other microorganisms | |
| 6. KD not related to SARS-CoV-2 | |
| 7. Drug hypersensitivity reaction (Stevens-Johnson syndrome) | |
| 8. Other systemic rheumatological diseases (systemic juvenile idiopathic arthritis and other autoinflammatory or autoimmune diseases) | |
| 9. Primary or secondary haemophagocytic lymphohistiocytosis (macrophage activation syndrome) |
KD: Kawasaki disease; SIM-PedS: paediatric multisystem inflammatory syndrome linked to SARS-CoV-2.
Given that most patients have previous SARS-CoV-2 infection, it has been suggested that SIM-PedS would affect children with a basic genetic susceptibility, not yet characterised,27,30 responsible for a delayed immune response to the virus (both nonspecific and adaptive), in which cytokines would play an important role.12,13,16,20,31 Some authors have described that the findings of patients with SIM-PedS coincide with the cytokine storm, hyperinflammation and multi-organ damage that are observed in the final phase of adults with severe COVID-19.13,31 Thus, the SARS-CoV-2 antibodies would be responsible for causing the syndrome,14 with patients with positive IgG and negative IgM antibodies being predominant, and to a lesser extent those with both positive IgG and IgM.17,32
Cases of affected patients from less than one year old to 20 years old have been described, although it predominates in children aged between 7.3 and 10 years old.13,14,32–34 Some studies have documented a higher frequency of the disease in males, while others show the same affectation in both sexes, and there is no clear predominance in one race or another,13,14,16,33 and no evidence that obesity or asthma are risk factors, despite the results of several studies.12,14,16
Radiological findingsThe most frequent radiological findings on X-ray, ultrasound or computed tomography (CT) scans in patients diagnosed with SIM-PedS are: cardiomegaly, pleural effusion and passive atelectasis, with the incidence of these findings varying depending on the imaging technique used.12,16,27
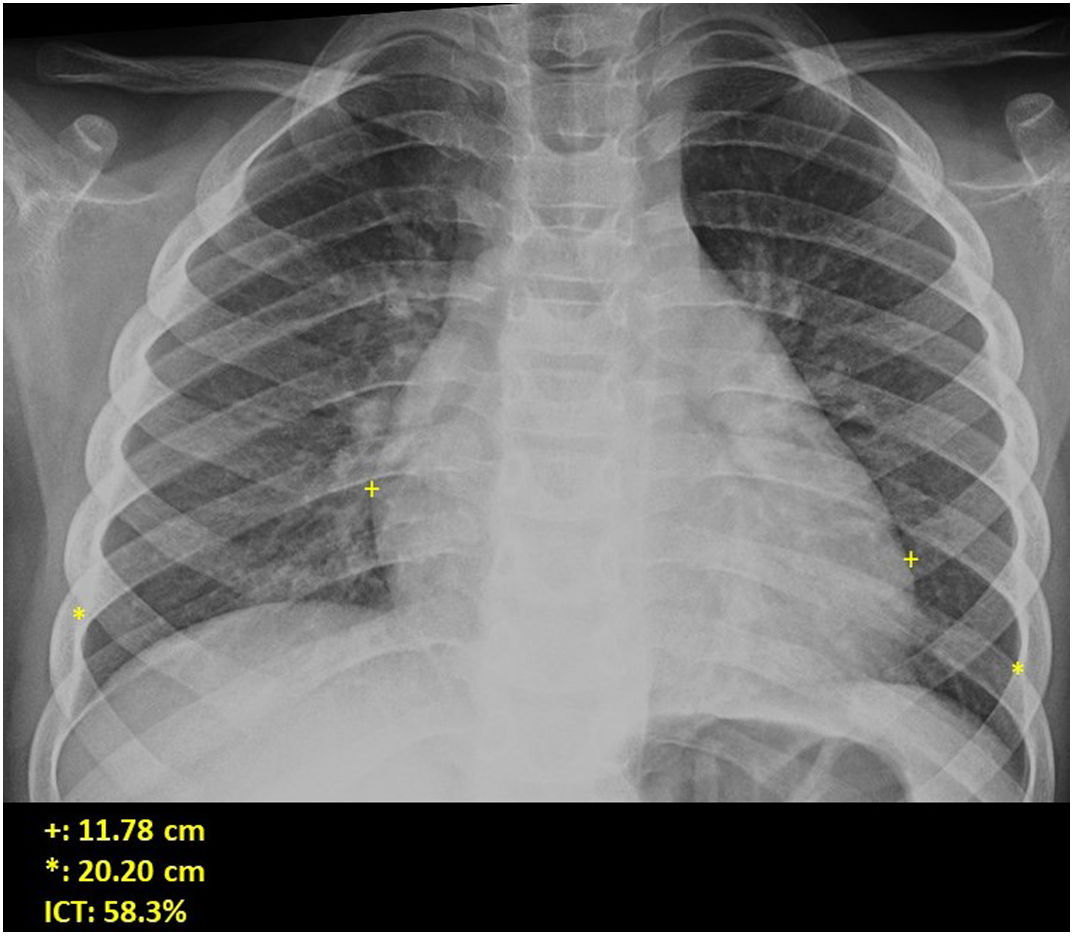
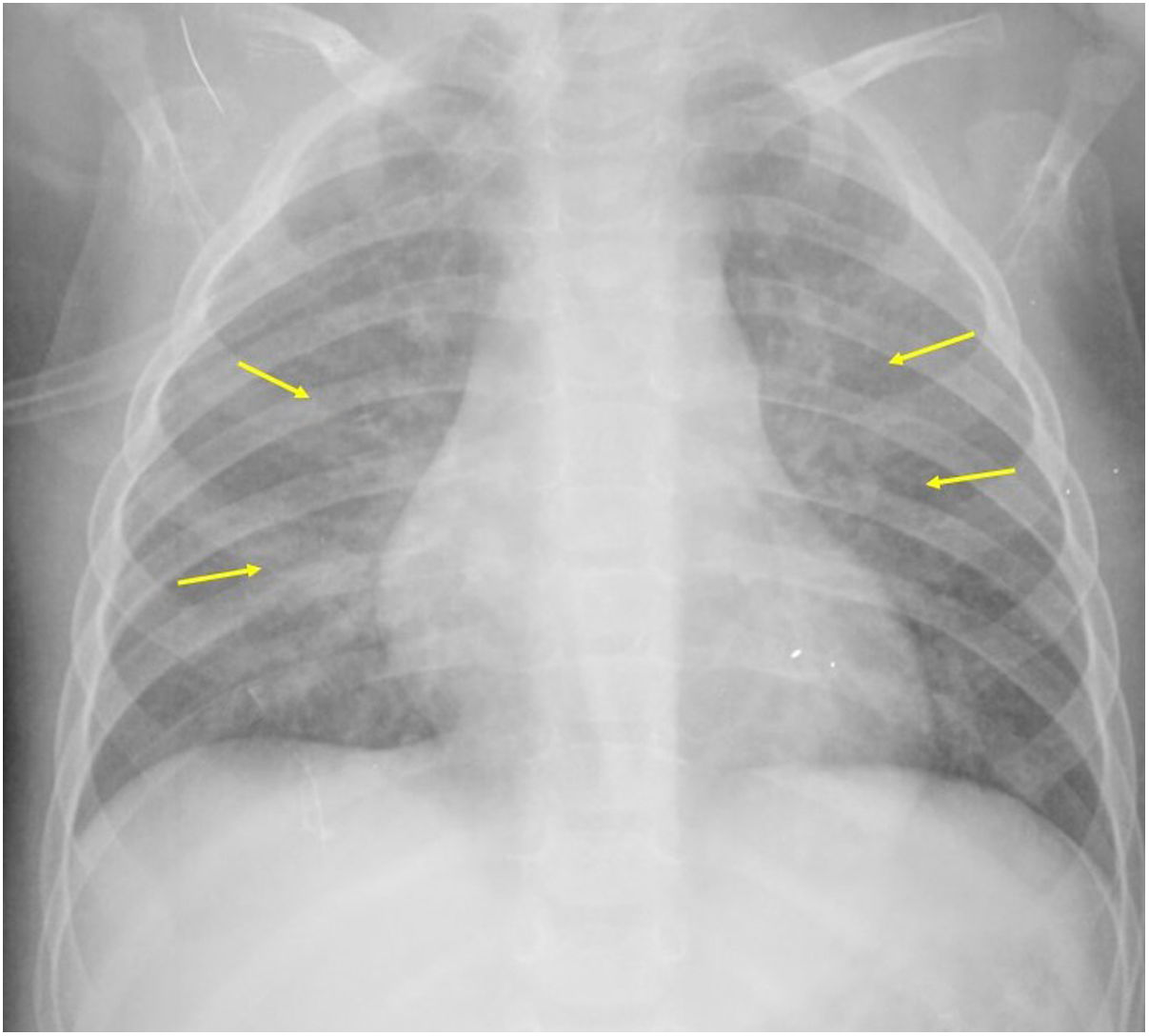
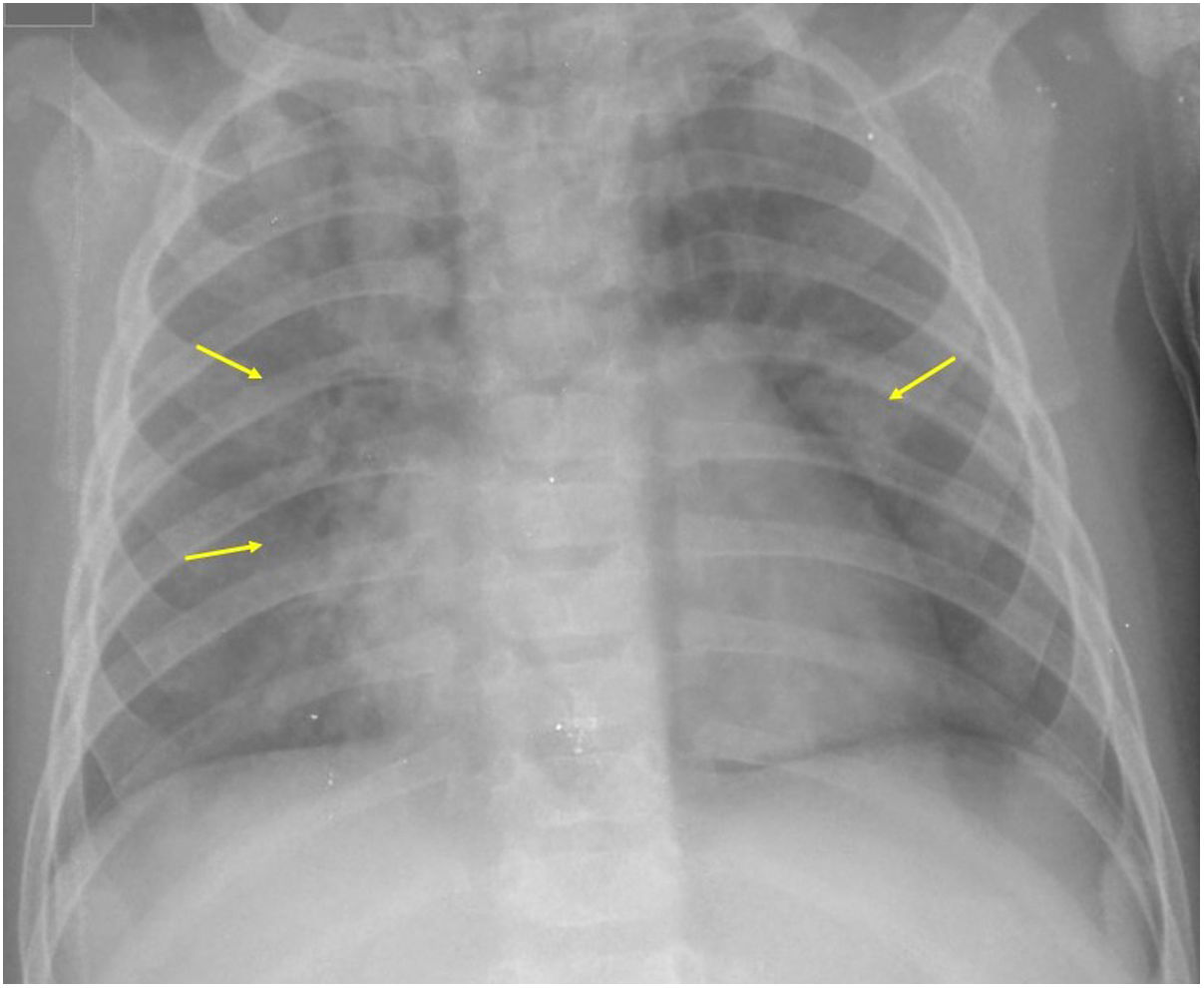
If the findings are analysed according to the imaging technique used, on chest radiograph the following can be observed: cardiomegaly (43%–62.5%) (Fig. 1), signs of congestive heart failure such as peribronchial thickening and perihilar interstitial pattern (34%–56%) (Figs. 1 and 2), with rapid appearance of perihilar consolidations due to cardiogenic pulmonary oedema (31%–56%) (Fig. 3), baseline opacities due to passive atelectasis (20%–56%) and pleural effusion (11%–44%). Less frequently there are confluent areas of ground-glass opacity and consolidations due to acute respiratory distress syndrome (ARDS), which may be asymmetric, and bibasal consolidations corresponding to pneumonia.12,19
Several authors have suggested that these findings are the consequence of heart failure, hypoalbuminaemia, fluid overload or a combination of all of these.19 However, it must be taken into account that an initial chest X-ray may be normal in up to 44%–46% of cases.12,19 Similar findings have also been described in KD, attributable, according to the most accepted theory, to pulmonary arteritis and/or inflammation of the lower respiratory tract.35
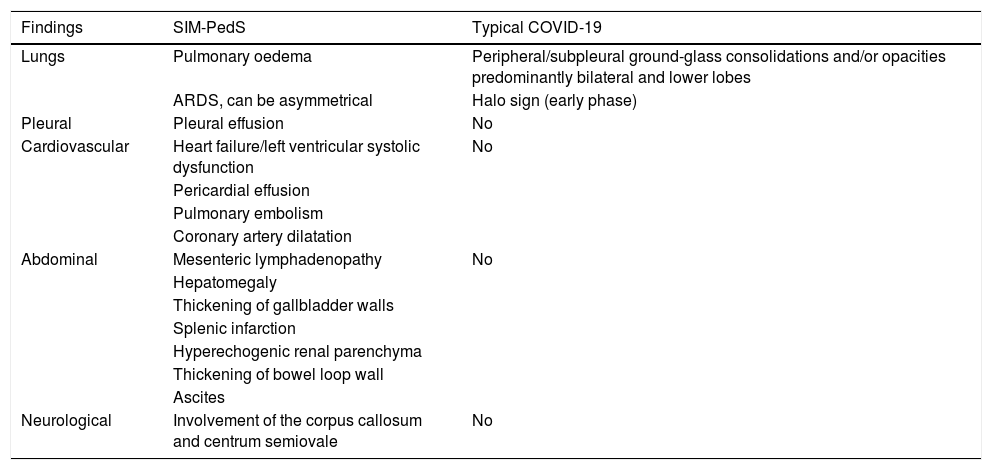
Among these chest findings, it is worth highlighting the much lower incidence of consolidations corresponding to pneumonia in patients with SIM-PedS compared to patients (both adult and paediatric) with COVID-19. Extensive ground-glass opacities are also less common and of atypical distribution with respect to the characteristics of COVID-19, which predominate in a peripheral location,12,36–38 so in patients with SIM-PedS these ground-glass opacities are more suggestive of corresponding to pulmonary oedema.19 The differences between the thoracic manifestations described in SIM-PedS and in COVID-19 in paediatric patients are shown in Table 3.
Differences between SIM-PedS imaging test findings and typical pediatric COVID-19 findings.
| Findings | SIM-PedS | Typical COVID-19 |
|---|---|---|
| Lungs | Pulmonary oedema | Peripheral/subpleural ground-glass consolidations and/or opacities predominantly bilateral and lower lobes |
| ARDS, can be asymmetrical | Halo sign (early phase) | |
| Pleural | Pleural effusion | No |
| Cardiovascular | Heart failure/left ventricular systolic dysfunction | No |
| Pericardial effusion | ||
| Pulmonary embolism | ||
| Coronary artery dilatation | ||
| Abdominal | Mesenteric lymphadenopathy | No |
| Hepatomegaly | ||
| Thickening of gallbladder walls | ||
| Splenic infarction | ||
| Hyperechogenic renal parenchyma | ||
| Thickening of bowel loop wall | ||
| Ascites | ||
| Neurological | Involvement of the corpus callosum and centrum semiovale | No |
ARDS: acute respiratory distress syndrome; SIM-PedS: paediatric multisystem inflammatory syndrome linked to SARS-CoV-2.
Lung ultrasound is an interesting imaging technique for the study of paediatric patients with COVID-19 and SIM-PedS, given its availability, mobility (it can easily be moved to paediatric ICUs without the need to transfer the patient, sometimes unstable) and safety due to absence of ionising radiation. Pulmonary ultrasound findings are similar to those described in adult patients with COVID-19.39,40 Patterns of pneumonia, increased lung water or pleural effusion with B lines in the lower and posterior lung segments have been described, which may increase (diffuse ultrasound interstitial syndrome), along with subpleural consolidations, thickening and fraying of the pleural line, as well as pleural effusion in variable amounts in the costophrenic sinuses. Established pneumonia shows images of consolidation with an air bronchogram, especially in the bases and posterior segments of the lungs.18,39,40
Routine chest CT is not recommended.18 In several studies, CT was performed, either with a pulmonary angio-CT protocol for suspected pulmonary thromboembolism (PTE)12 or, less frequently, due to sepsis or fever of unknown cause,19 while in the study by Hameed et al., it was decided to perform CT of the coronary arteries in 80% of the patients to rule out coronary involvement, given the similarity of this syndrome to KD, which causes dilatation and coronary aneurysms. Most of the lung parenchyma was included in this study (excluding only the apical and basal ends).19
In Blumfield's study in which pulmonary CT angiography was performed, segmental PTE was identified in 25% of the children, without signs of right ventricular overload or pulmonary infarctions.12 This incidence of PTE is similar to that observed in adults with COVID-19, which according to different studies ranges between 22% and 30%.41–44
Some authors have suggested that the hyperinflammatory state that characterises SIM-PedS, with elevated inflammatory markers such as fibrinogen, D-dimer, ferritin, and IL-6, could predispose to prothrombotic coagulopathy and thromboembolic complications, including PTE, similar to that observed in the later, more serious stages of COVID-19 in adults.13,31,44 However, the clinical importance of segmental PTE is unclear, as some researchers have shown that there are no significant differences in the need for ICU admission, intubation or duration of intubation between COVID-19 adult patients who develop segmental PTE and those who do not.44
In the aforementioned work by Hameed et al., in which a CT scan was performed to study the coronary arteries, no incidental PTE was detected despite the fact that all patients had high levels of D-dimer.19
The most frequently observed findings in the lung parenchyma by CT were: lower lobe atelectasis (50%),12 the association of consolidations and atelectasis (39%), ground-glass opacities associated with patchy consolidations (9%) and only one patient with small foci of consolidations with peripheral ground-glass halo has been described,19 a finding that is considered typical of COVID-19 and most frequently described in children.37 The possibility that these findings may be secondary to KD-like vasculitis has been suggested.19 Pleural effusion was observed in 17%–30% of cases. The presence of hilar adenopathies of significant size detected by CT varies between 0% and 15% according to various studies,12,19 and no thymic alterations have been identified.19
The most frequent cardiological alterations are those of heart failure (in some series they are described in up to 51% of cases),19 with acute myocarditis that usually manifests a week after onset of fever and gastrointestinal symptoms.17 In echocardiography, the most common finding is left ventricular systolic dysfunction, observed in several studies in between 25% and 63% of cases.12,13,16,27 In 71% of these patients, ejection fractions between 30% and 50% are described, and fractions lower than 30% in 28% of cases.16 Other findings detected by echocardiography are dilatation of the coronary arteries observed in between 17% and 25% of cases and pericardial effusion in between 9% and 40% of cases,12,14,16,17 as well as signs of pancarditis and mitral regurgitation.17,19 A possible cause of the variability in the detection of coronary anomalies in the different studies is the different imaging technique used for their detection - ultrasound, CT or magnetic resonance imaging (MRI) - with the result that, in the studies in which coronary artery CT was performed, aneurysms were detected in 20% of patients,19 while they were not detected by MRI.17
On cardiac MRI, signs of hyperaemia and diffuse myocardial oedema can be observed in T2 and in the native T1 map, without associating late gadolinium enhancement that suggests replacement fibrosis or focal necrosis.17 These data suggest that the cardiovascular involvement of SIM-PedS is more aggressive than that observed in KD13,14,19,20 and more frequent than in COVID-19, although it has also been described in severe acute infection by SARS-CoV-2, both in adults and in children, with the development of myocardial damage and heart failure.17,45,46 The most widely accepted explanation for these findings is that viral myocarditis causes damage by viral infiltration and an immune response to it,47,48 while postinfectious myocarditis related to SIM-PedS would correspond to an inflammatory infiltration of the myocardial interstitium in response to the immunological cascade triggered against an antigen and not against SARS-CoV-2 itself.17 Cytokines (cytokine storm syndrome) would play an important role in this,49 similar to what occurs in KD, in which histopathological analyses of the heart demonstrate a predominance of infiltration by macrophages and neutrophils in the myocardial interstitium with little myocardial cell degeneration or necrosis.50 The relatively rapid recovery of cardiac function that patients show after receiving the correct treatment, with MRI signal normalisation, supports the theory previously offered and by which several researchers suggest that ventricular systolic dysfunction is due more to myocardial stunning or oedema than myocardial damage.16,17
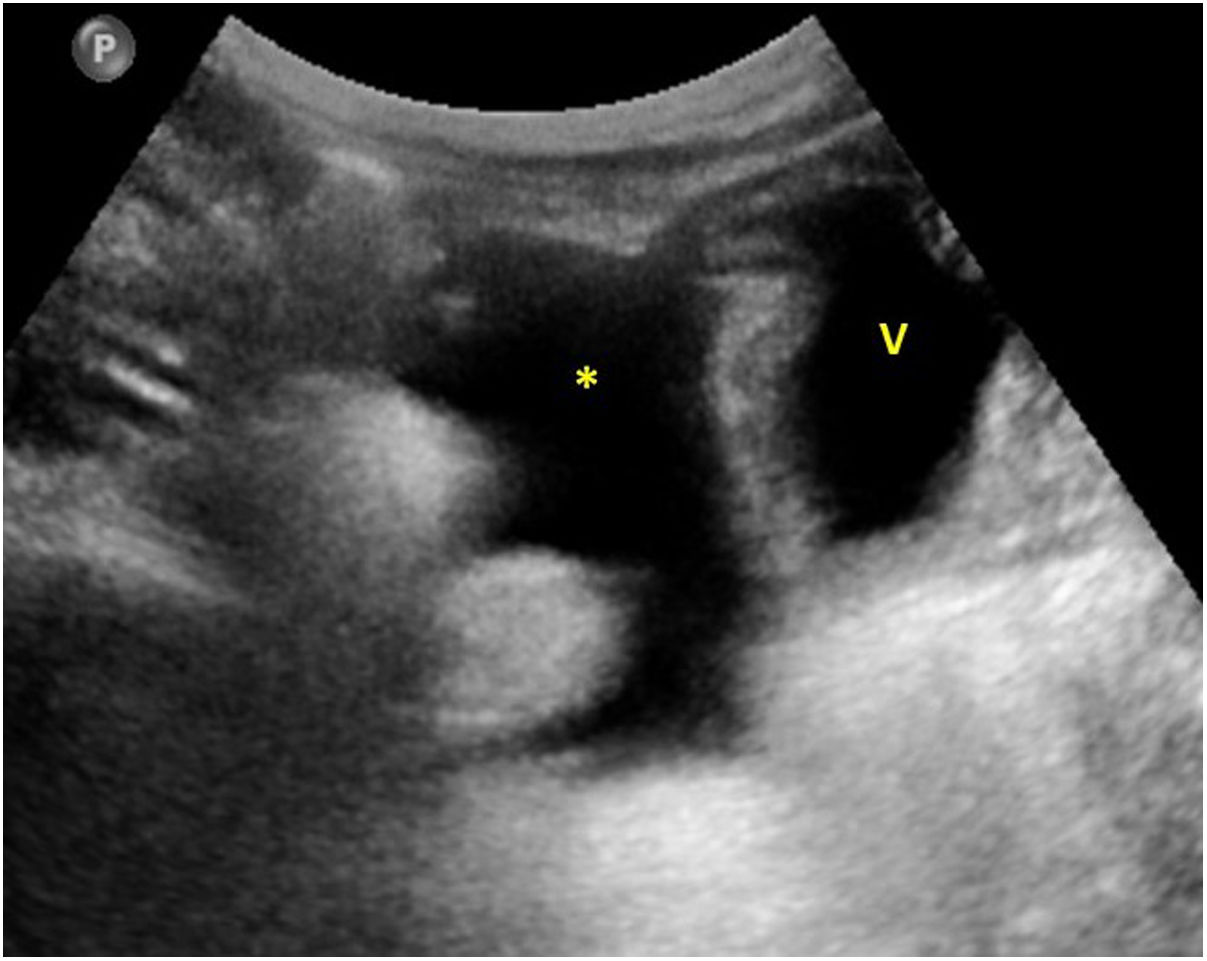
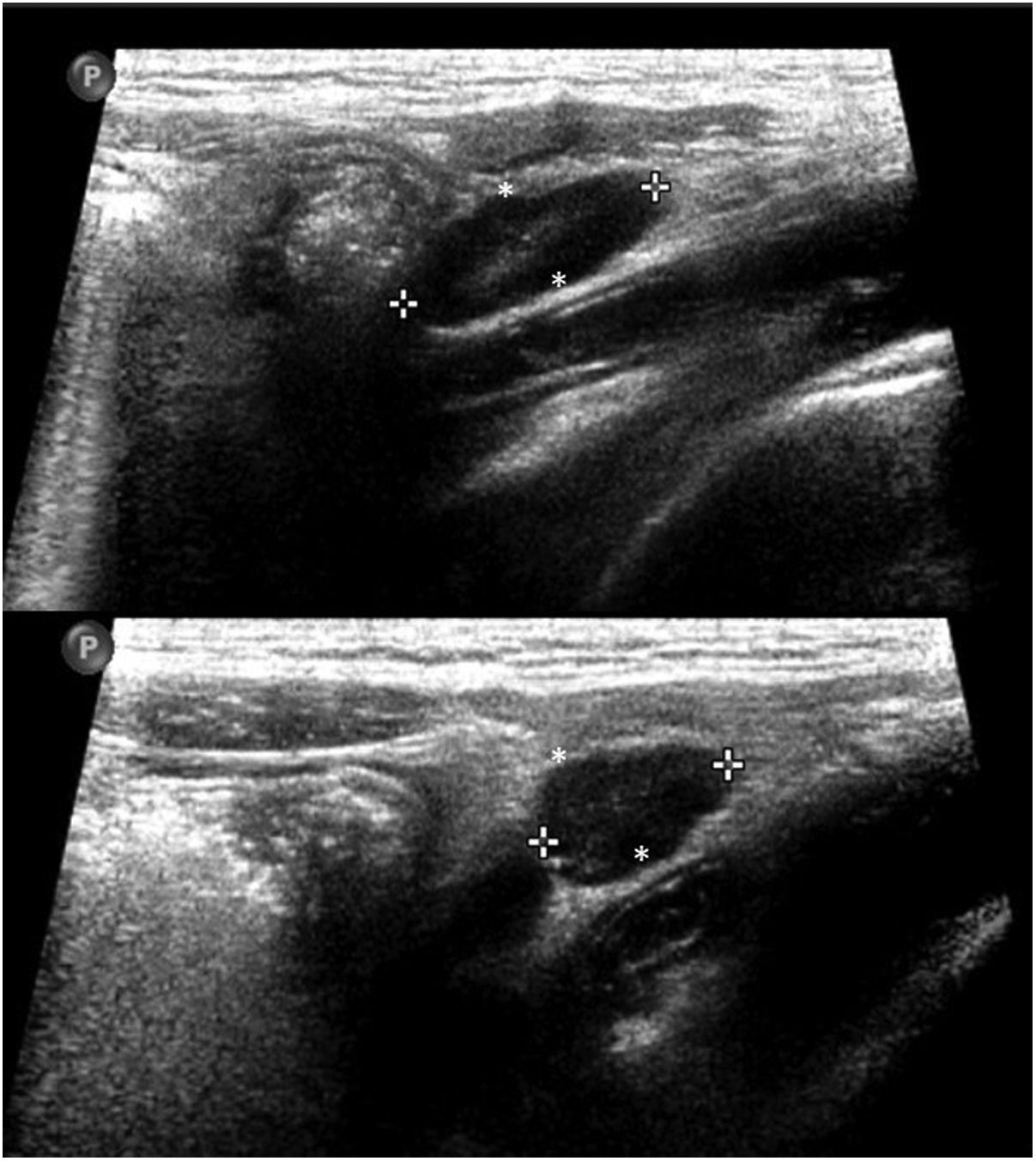
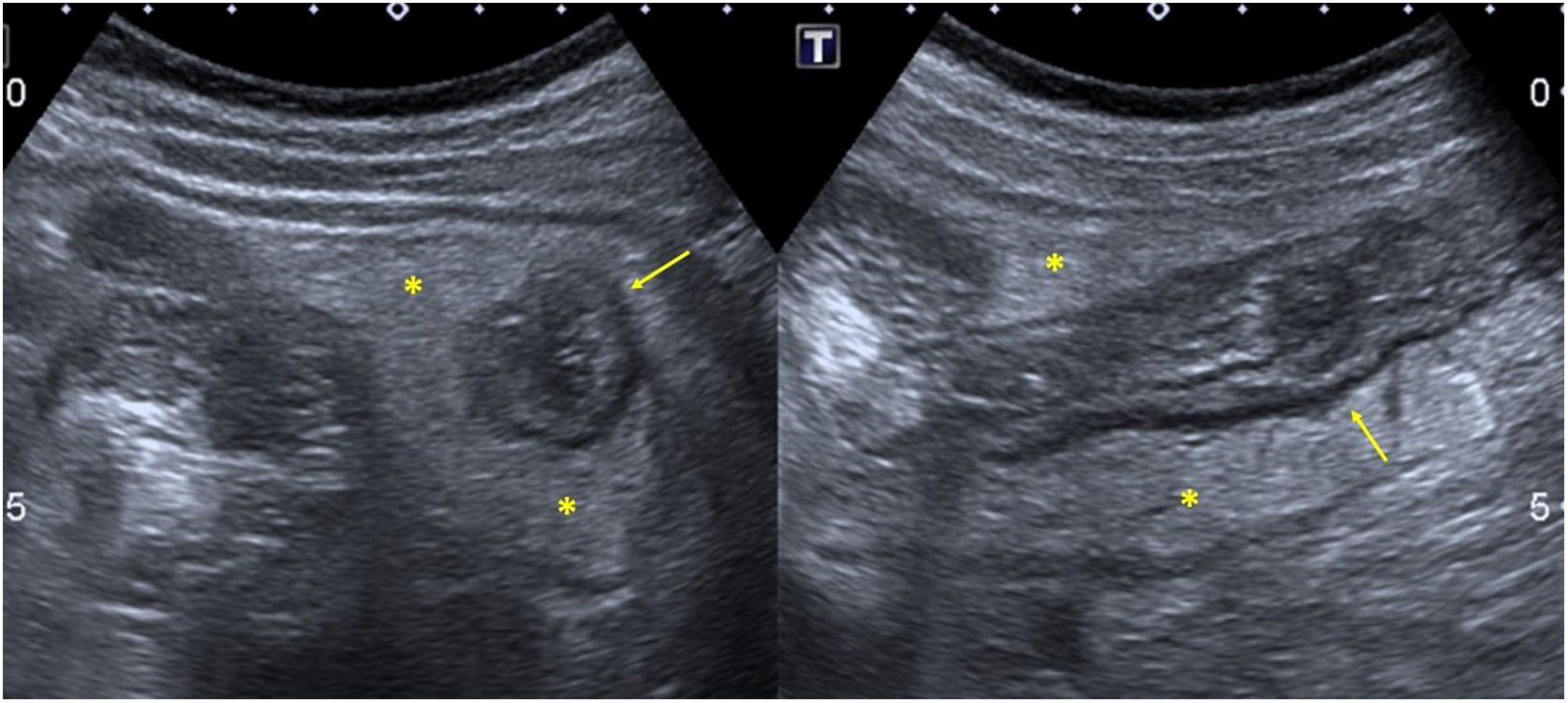
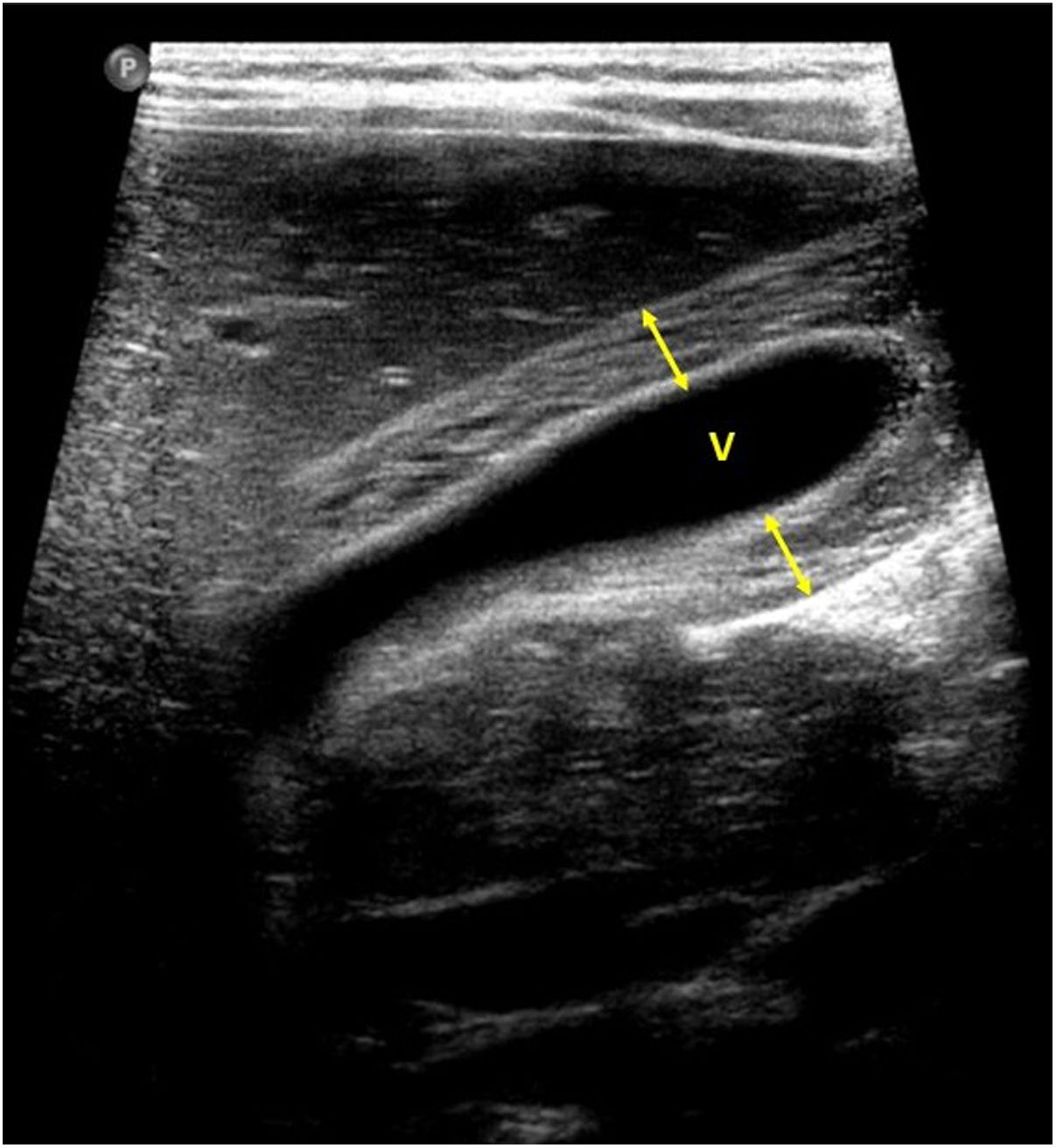
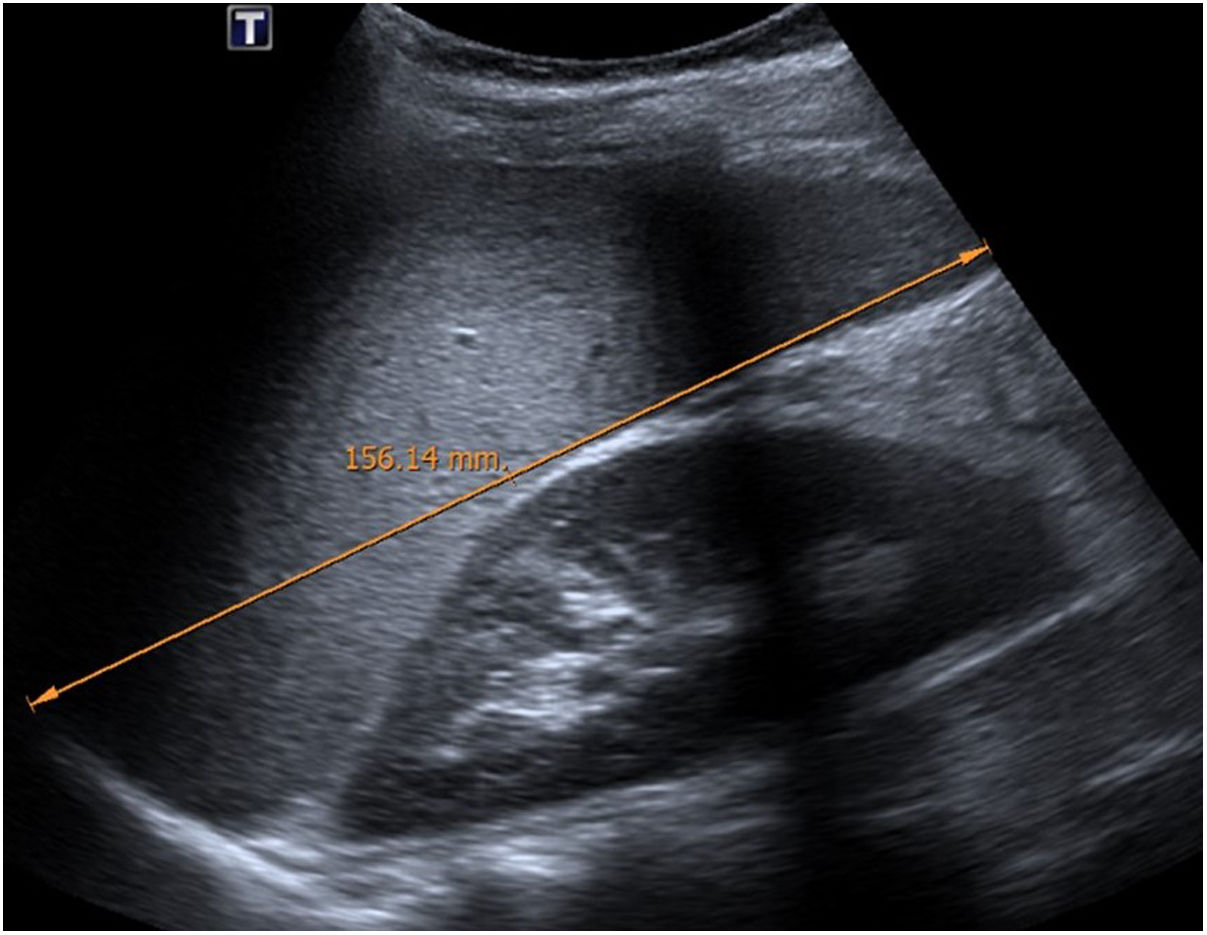
Regarding abdominal involvement, the most frequently observed findings on ultrasound are: ascites (38%–53%) (Fig. 4), inflammatory changes in the right iliac fossa (RIF) with lymphadenopathies of morphology similar to those observed in mesenteric adenitis (13%–47%) (Fig. 5), hepatomegaly (10%–38%) (Fig. 6), increased cortical echogenicity of the kidney parenchyma (5%–31%), intestinal parietal thickening (19%–21%) (Fig. 7), primarily of the distal ileum and secondly of the cecum, increased periportal echogenicity (16%), perivesicular oedema and thickening of the gallbladder walls (16%–19%) (Fig. 8), biliary sludge (16%), splenic infarcts (10%), splenomegaly (6%) (Fig. 9), and thickening of the bladder walls (6%).12,14,16,19
It has been hypothesised that gastrointestinal symptoms may be explained by mesenteric lymphadenopathy27 and by intestinal parietal ischaemia secondary to vasculitis, while heart failure and/or shock would contribute to the thickening of the ileocecal walls as the ileocolic artery is the most distal branch of the superior mesenteric artery.19 One of the theories proposed to explain the pathophysiology of mesenteric lymphadenitis is that it is secondary to lymphoid hyperplasia.51 The RIF would be more frequently affected by its abundant lymphatic tissue and by the presence of Peyer's patches in the distal ileum. In this way, the cases of mesenteric adenitis observed would correspond to the patients described with SIM-PedS who presented with simulating acute appendicitis.52
In patients with gastrointestinal symptoms and inconclusive ultrasound studies, in whom appendicitis or intra-abdominal collections have not been excluded, it may be decided to perform an abdominal CT scan based on clinical suspicion, preferably with intravenous contrast administration,18,19 with the benefit that the use of oral contrast can provide being more doubtful. In the cases in which CT was performed, the following were observed: ascites (80%), inflammatory changes in RIF with increased attenuation of fat and lymphadenopathy (60%), periportal and perivesicular oedema (40%), thickening of the intestinal wall (20%) and splenic infarction (20%).19 Splenic infarction has been described in patients with KD and other inflammatory vasculitis, which is why in SIM-PedS it is also attributed to inflammation of the splenic artery.19,53 The difference in its detection - 10% of the patients through abdominal ultrasound and in up to 20% of the cases in which CT was performed - could justify performing CT only if massive or complicated splenic infarction (abscesses, haemorrhage or rupture) that would need a different therapeutic management is suspected,18,54 which has not been described in the cases of SIM-PedS.19 It is also suggested that ascites, thickening of the gallbladder walls, periportal and perivesicular oedema are secondary to systemic inflammation, hypoalbuminaemia, serositis, fluid overload and/or heart failure.19
In patients with SIM-PedS who underwent imaging tests for presenting neurological manifestations, alterations have been observed in the splenium and genu of the corpus callosum and in the centrum semiovale, with hypodensity on CT, and hyperintensity on MRI in T2 and diffusion restriction in 75% of cases.55 However, other investigators have reported that no pathological findings were seen on CT or MRI.19 Given its similarity to KD, the development of ischaemic infarction as a complication of vasculitis remains a possibility, and it has also been described as a complication in patients with COVID-19 receiving treatment with intravenous immunoglobulins.56
Evolution and prognosisPatients with SIM-PedS may develop cardiogenic shock and require admission to the paediatric ICU, with a mean stay of between 4 and 7 days. In this group, between 80% and 100% will require inotropic/vasopressor support, and up to 66%–88% will need mechanical ventilation to achieve cardiovascular stabilisation.14,16,33 Approximately 25% of patients with heart failure will require mechanical ventilation with an extracorporeal membrane oxygenation (ECMO) system.16,34 Despite this, the vast majority of patients improve clinically with appropriate treatment after a correct diagnosis, and the response of cardiac dysfunction to treatment with intravenous immunoglobulins has been very satisfactory, with complete recovery of ventricular function in 71% of patients.16,17 This recovery of cardiac function supports the theory that heart failure is not caused by myocardial damage as in adults with COVID-19. Although pulmonary or neurological sequelae have not been described, more studies are needed to evaluate the possible long-term sequelae that this syndrome could cause.12,16,55
LimitationsThe studies published up to the time of this work have limitations. The most significant is the small number of paediatric patients presented in many of them, so generalisation of the results can lead to error. The clinical manifestations of this syndrome vary in severity, and in published studies there may be an over-representation of the most severe cases.32 Future studies would need to include a greater number of patients and ideally be multicentre, to be able to correlate the radiological findings with the complex clinical course of these patients and pinpoint their specificity and the underlying pathogenesis.19,57
ConclusionsSIM-PedS is a postviral multisystem inflammatory syndrome in which patients present with sustained high fever, gastrointestinal and mucocutaneous symptoms, with rapid progression to cardiogenic shock and multisystem damage.12–15 Given that the clinical manifestation of SIM-PedS is not specific, imaging tests play a very important role in its diagnosis,12 and radiological findings correlate well with the clinical presentation of SIM-PedS and with laboratory data. Gastrointestinal symptoms, including abdominal pain, vomiting and diarrhoea, are probably a reflection of the multi-organ involvement of SIM-PedS.16 In this group of patients, abdominal ultrasound may be the first imaging technique requested, aimed at excluding appendicitis or some other acute abdominal pathology.12 Although the imaging findings are not specific and the initial chest X-ray is often normal, the presence of hepatomegaly, hyperechoic kidneys, ascites, pleural effusion, thickening of the intestinal walls or of the gallbladder, or mesenteric lymphadenopathy in patients with a previous history of exposure to SARS-CoV-2, should alert radiologists to a possible diagnosis of SIM-PedS, as patients can quickly worsen.12 Both paediatric and non-paediatric radiologists should be aware of and suspect this syndrome since cases have been described in young people between 15 and 20 years of age.
Although many children with SIM-PedS are seriously ill and require admission to the paediatric ICU, a large majority improve clinically with appropriate treatment after correct diagnosis. However, the possible long-term sequelae of this syndrome are yet to be determined.12
Authorship- 1
Responsible for study integrity: RSO, MLFB, EGM.
- 2
Study concept: RSO, MLFB.
- 3
Study design: RSO, MLFB, EGM, MÁEP, EMAM.
- 4
Data collection: N/A.
- 5
Data analysis and interpretation: N/A.
- 6
Statistical processing: N/A.
- 7
Literature search: RSO, EGM, MÁEP, EMAM.
- 8
Drafting of the work: RSO, MLFB, EGM, MÁEP, EMAM.
- 9
Critical review of the manuscript with intellectually relevant contributions: RSO, MLFB, EGM, MÁEP, EMAM.
- 10
Approval of the final version: RSO, MLFB, EGM, MÁEP, EMAM.
The authors declare that they have no conflicts of interest.
The authors would like to express gratitude to Drs J. Torres Nuez, G. Martínez Sanz, S.P. Alandete Germán, M.A. Meseguer Ripollés and L. Oro.
Please cite this article as: Sánchez-Oro R, Fatahi Bandpey ML, García Martínez E, Edo Prades MÁ, Alonso Muñoz EM. Revisión de los hallazgos clínicos y radiológicos del nuevo síndrome inflamatorio multisistémico pediátrico vinculado a la COVID-19. Radiología. 2021;63:334–344.