Breast radiology: New horizons in times of pandemics
More infoTo compare the diagnostic performance of breast ultrasound and breast magnetic resonance imaging and to correlate the findings on the two techniques that are suggestive of implant rupture.
Material and methodsWe reviewed the images and reports of breast ultrasound and magnetic resonance imaging studies done in our diagnostic and interventional breast imaging unit to evaluate breast implants in 205 patients between January 2015 and December 2017.
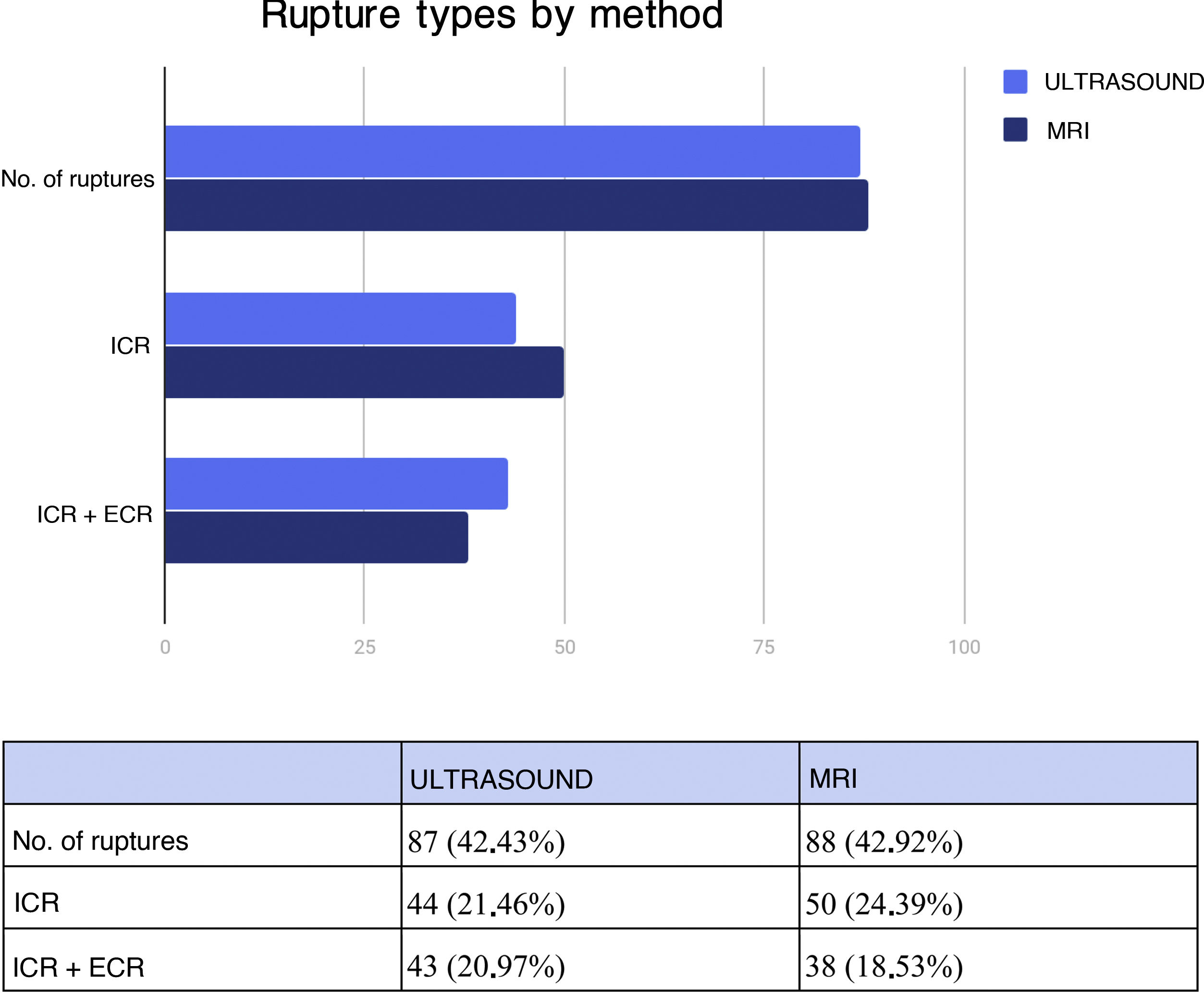
ResultsUltrasound findings were compatible with implant rupture in 87 (42.4%) patients: intracapsular rupture in 44 (21.5%) and intracapsular and extracapsular rupture in 43 (21.0%). Ultrasound yielded 85.2% sensitivity, 89.7% specificity, 86.2% positive predictive value, and 89.0% negative predictive value. Magnetic resonance imaging findings were compatible with implant rupture in 88 (42.9%) patients: intracapsular rupture in 50 (24.4%) and intracapsular and extracapsular rupture in 38 (18.5%). The correlation between positive findings for the location of the rupture on the two imaging techniques was excellent (0.77; p < 0.0001).
ConclusionWe found high concordance between the two techniques for the detection of intracapsular and extracapsular implant rupture. These results consolidate the use of ultrasound as the first-line imaging technique to evaluate implant integrity in our population; magnetic resonance imaging can be reserved for cases in which the ultrasound diagnosis of implant integrity is uncertain.
El objetivo de este trabajo es evaluar el rendimiento diagnóstico de la ecografía mamaria en comparación con la resonancia magnética mamaria y la correlación entre ambos métodos para la detección de los hallazgos sugestivos de rotura protésica.
Material y métodosEn la Sección de Diagnóstico e Intervencionismo mamario, en el período comprendido entre enero de 2015 y diciembre de 2017 se revisaron las imágenes e informes de ecografía y resonancia magnética mamarias con protocolo para evaluación de prótesis, de 205 pacientes.
ResultadoEl estudio ecográfico fue compatible con rotura protésica en 87 (42,43%) pacientes: rotura intracapsular en 44 (21,46%) pacientes y rotura intra- y extracapsular en 43 (20,97%) pacientes. La ecografía demostró una sensibilidad del 85,22% y una especificidad del 89,74%. El valor predictivo positivo (VPP) fue del 86,20% y el valor predictivo negativo (VPN) del 88,98%. La resonancia magnética mostró hallazgos compatibles con rotura protésica en 88 (42,92%) pacientes: 50 (24,39%) pacientes con rotura intracapsular y 38 (18,53%) con rotura intra- y extracapsular. La coincidencia de los hallazgos positivos entre resonancia magnética y ecografía para la localización de rotura arrojó una excelente correlación: 0,77 (p < 0,0001).
ConclusiónNuestros resultados arrojaron una concordancia alta entre ambos métodos para la detección de rotura intra- y extracapsular de los implantes. Estos resultados consolidan la utilización de la ecografía como primer método de evaluación de integridad protésica en nuestra población, reservando la resonancia magnética para aquellos casos de dudas diagnósticas ecográficas de integridad protésica.
Surgical procedures for breast augmentation with implants for multiple purposes (reconstructive, cosmetic, etc.) have increased in number in recent years. Therefore, it is essential to be familiar with the characteristics of implant integrity on imaging. Implant rupture can go clinically unnoticed. Findings on imaging of signs of early rupture in a consultation are valuable for weighing the possibility of timely surgical replacement.1,2 Statistics on implant rupture vary considerably in the specialised literature. Clinical diagnosis has demonstrated low sensitivity, with non-specific findings.3–5
Ultrasound and magnetic resonance imaging (MRI) are the two methods used for evaluating implant integrity, supported by extensive literature. However, debate still persists about the appropriate use of these methods.6–8 MRI has shown the best diagnostic performance for evaluation of implant integrity, with a sensitivity of 64%–100% and a specificity of 63%–100%. However, its use is limited by its high cost, as well as the fact it is contraindicated in some patients.9 Ultrasound is considered a valuable tool for evaluating implant integrity, due to its low cost and accessibility, and is perhaps the most appropriate first choice in the diagnostic arsenal.10–12
All implants consist of an outer shell made of silicone in the form of an elastomer. This outer shell is a semi-permeable membrane that under normal (intact) conditions can allow for a certain (minimal) amount of microscopic diffusion of silicone gel. This phenomenon, called gel bleed, is almost always negligible. It should not be mistaken for pathological leakage of silicone through a ruptured implant shell.
An intracapsular rupture (ICR) is a rupture that remains contained, as the fibrous capsule is intact. This happens when silicone gel leaks through a crack or tear in the implant membrane, but does not pass through the fibrous capsule. In the absence of a history of implant rupture, surgical implant review or injection of free silicone, the presence of silicone outside of the fibrous capsule and in neighbouring tissues signifies an extracapsular rupture (ECR). Possible findings in this situation include siliconomas, which form as a result of a granulomatous reaction in relation to silicone collections behaving like foreign bodies.
It should be borne in mind that the artefact of echogenic noise within the lymph nodes is not, in itself, sufficient evidence to suggest implant rupture, due to the possibility of ongoing gel bleed.13
Objective: to assess the diagnostic performance of breast ultrasound compared to breast MRI and the correlation between the two methods for detecting findings suggestive of implant rupture.
Material and methodsIn this retrospective study, images and reports from breast ultrasound and MRI performed in 205 patients with implants, with or without symptoms, between January 2015 and December 2017 were reviewed. All patients were examined using both techniques.
This study was conducted in accordance with the principles of the Declaration of Helsinki and approved by the Independent Ethics Committee at our institution, under Protocol No. 5055.
Patients with retropectoral or retroglandular implants filled with saline or silicone gel were enrolled.
Breast MRI was considered the gold standard. The variables evaluated in the sample were: age, implant replacement prior to the conduct of the study, pain, history of trauma, laterality of structural changes, presence of findings of rupture on ultrasound, presence of findings of rupture on MRI and location (intracapsular or extracapsular) of structural changes on ultrasound and/or MRI.
Cases with echogenic lymph nodes and intact implants, with no history of implant replacement or handling which would explain these findings, were grouped under the “gel bleed” variable.
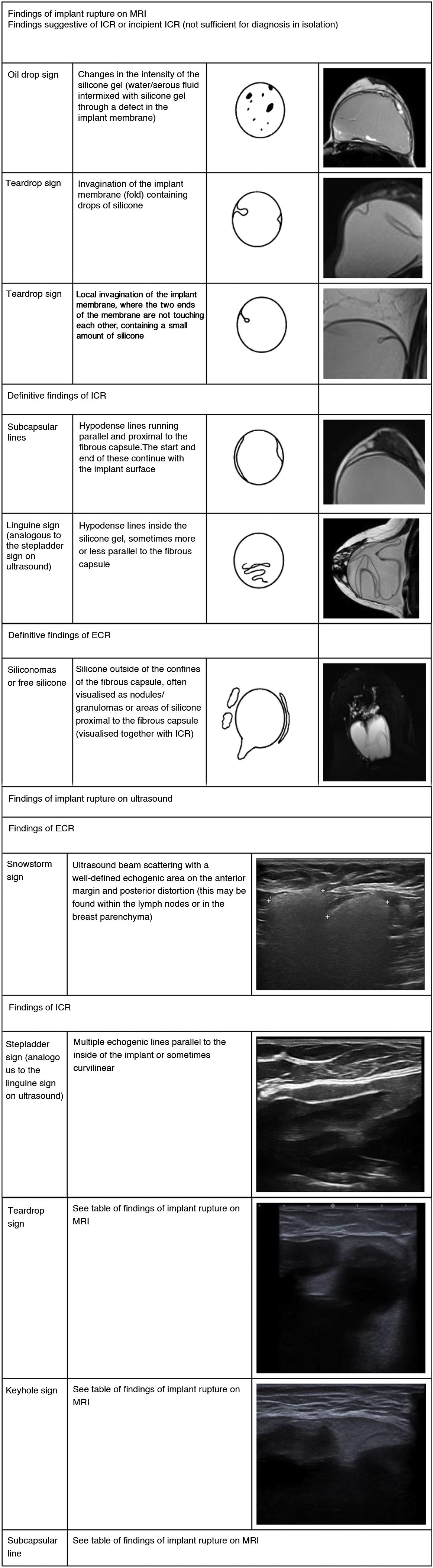
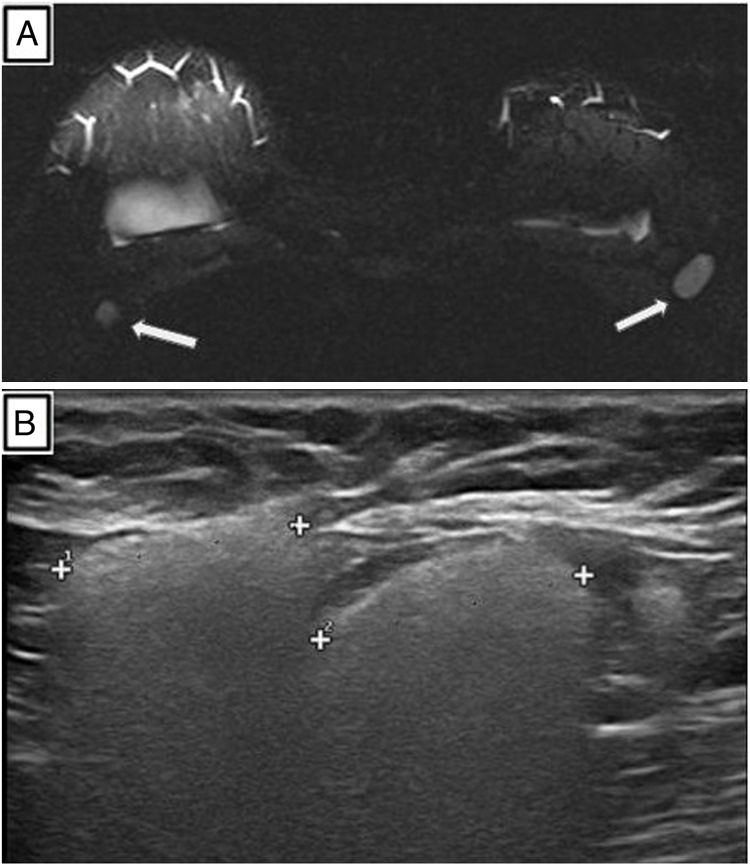
The following were defined as findings consistent with ICR on ultrasound: a) changes in implant echogenicity; b) diffuse medium-intensity echoes outside the membrane but inside the intracapsular space, corresponding to extravasated silicone gel contained by the capsule; c) the stepladder sign; and d) the keyhole sign. The snowstorm sign, in relation to extracapsular silicone corresponding to the formation of granulomas (siliconomas) visualised in the axillary and/or intramammary lymph nodes and in the breast parenchyma, was considered a finding of ECR.
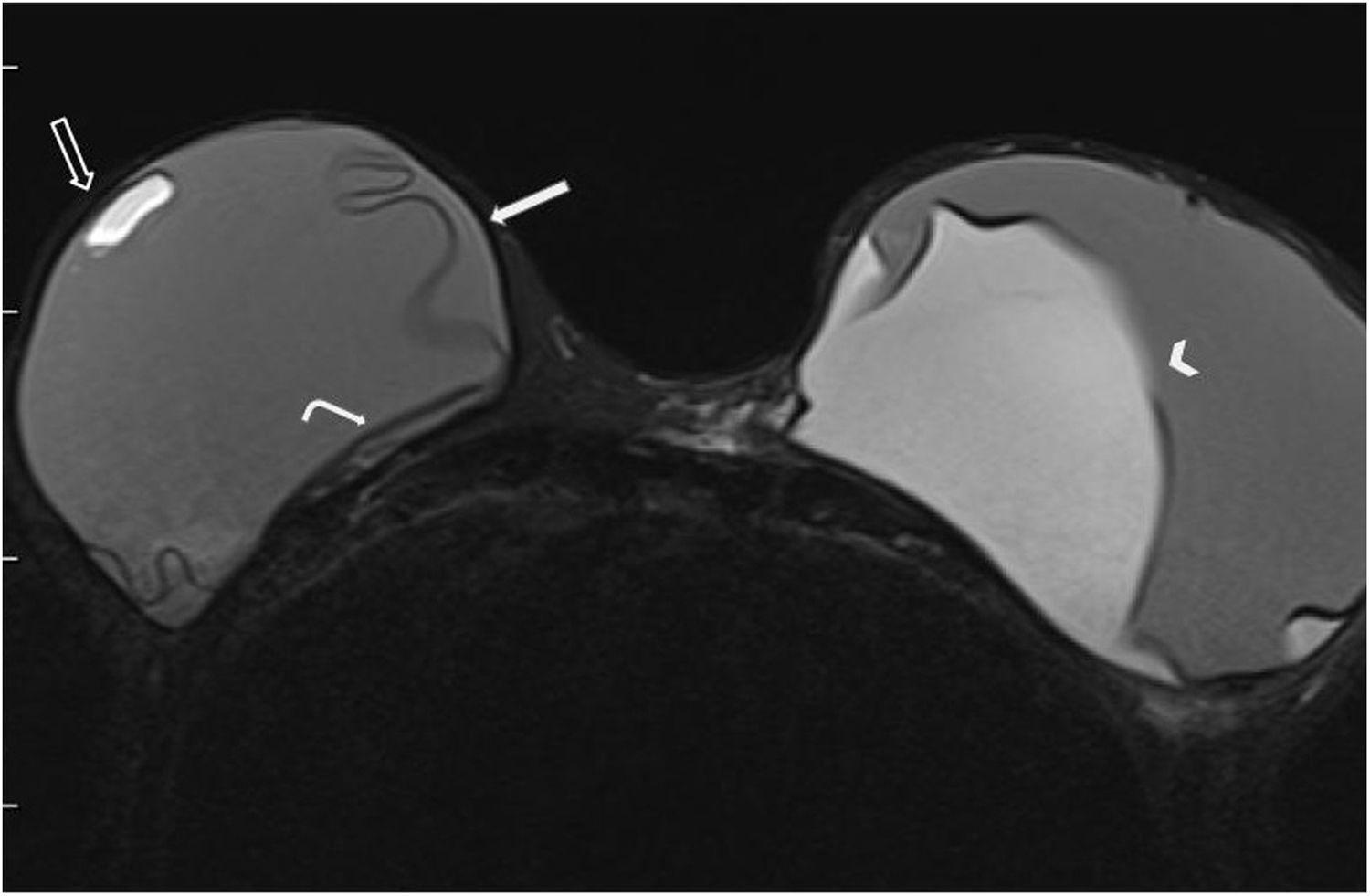
In MRI, silicone-only sequences were used to evaluate parenchymal or lymph node ECR, and T2-weighted sequences were used determine ICR represented by: a) the presence of subcapsular lines, b) the keyhole sign, c) the teardrop sign and d) the linguine sign. Hyperintense images (siliconomas) on silicone-only sequences in the parenchyma or lymph nodes were considered a finding of ECR.
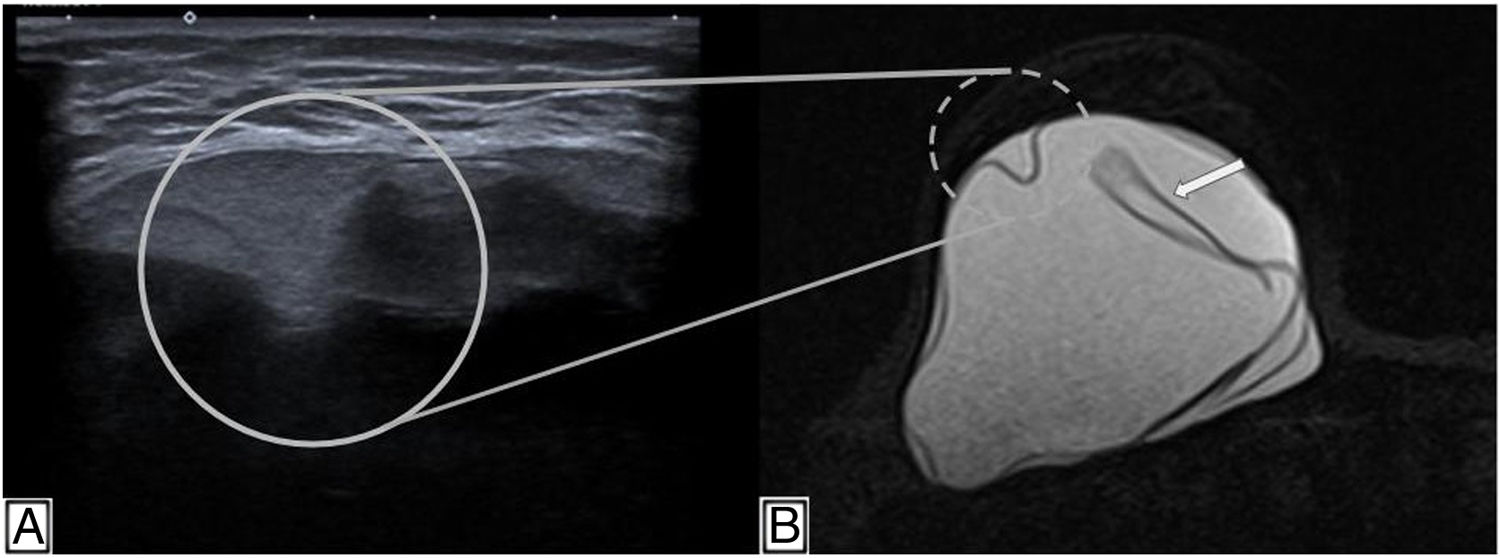
In patients with a history of injection of free silicone or incomplete removal of a ruptured implant, MRI will identify small areas of hyperintensity on sequences sensitive to silicone surrounded by normal parenchyma (Figs. 1–3).
Breast magnetic resonance imaging. (A) Silicone-only sequences showing a posterior and external image with the same signal intensity as silicone as a result of intracapsular silicone gel bleed (white arrow). (B) Sagittal T2-weighted sequence with hypointense lines as a linguine sign in ICR.
MRI studies were performed using two systems, the Siemens Avanto (1.5 T) and the Philips Ingenia (3 T), with specific coils for breasts. The MRIs were done with the patient in prone decubitus with both arms above the head to minimise breast distortion and movement artefacts. Bilateral acquisition included a multiplanar locator sequence, an axial T1-weighted sequence, an axial T2-weighted sequence with and without fat suppression, a sagittal T2-weighted sequence, and silicone-only sequences. All MRIs were evaluated by radiologists with four to seven years of experience in breast MRI.
Ultrasounds were performed using Esaote MyLab Class ultrasound systems, with linear matrix transducers with a frequency range of 7.5–15 MHz. The ultrasounds were performed by radiologists specialising in breast imaging, with four to 19 years of experience.
Patients under 18 years of age and patients with indications other than evaluation of implant integrity were excluded.
Data were recorded in a database developed in the Excel 2007 software program using a form designed for the study.
Data were analysed using the SPSS 17.0 software program. Medians as well as minimum and maximum values were used as units of distribution and central tendency. The χ2 test was used to determine differences between categorical variables, and the Mann–Whitney test was used for continuous variables. The level of significance was set at p ≤ 0.05. The odds ratio was used as a measure of association, with 95% confidence intervals.
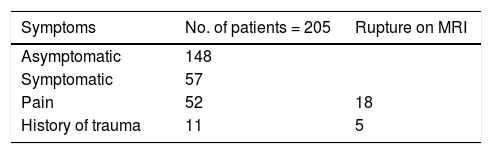
ResultsA total of 205 patients with a mean age of 51.4 years (standard deviation [SD]: 13.3) were included in the analysis. Of these, 72.19% (148/205) were asymptomatic and 27.8% (57/205) were symptomatic (Table 1).
Our series did not find a statistically significant difference in patients with a diagnosis of implant rupture who sought care due to pain or had a history of prior trauma (pain [p: 0.1] and trauma [p: 0.5]).
A history of implant replacement was found in only 20 patients (9.76%).
In 12 patients (6.49%), we found lymph nodes with the presence of silicone on ultrasound and intact implants on MRI. These findings were interpreted as gel bleed, as these patients had no history of implant replacement that would account for silicone infiltration of the lymph nodes or intracapsular rupture that would account for an associated extracapsular rupture.
Just 13 patients (6.34%) represented false negatives. In them, ultrasound did not manage to detect ICR or combined (intracapsular and extracapsular) rupture, but MRI later yielded positive results (p < 0.0001). In addition, 12 patients (5.85%) showed findings of ICR on ultrasound that were later not confirmed by MRI (false positives) (p < 0.0001). A total of 75 patients (36.59%) were found to be true positives, with both studies showing findings of rupture, and a total of 105 patients (51.22%) were found to be true negatives, with both studies showing implant integrity.
Ultrasound yielded a sensitivity of 85.22% and a specificity of 89.74%. The positive predictive value (PPV) was 86.20%, and the negative predictive value (NPV) was 88.98%.
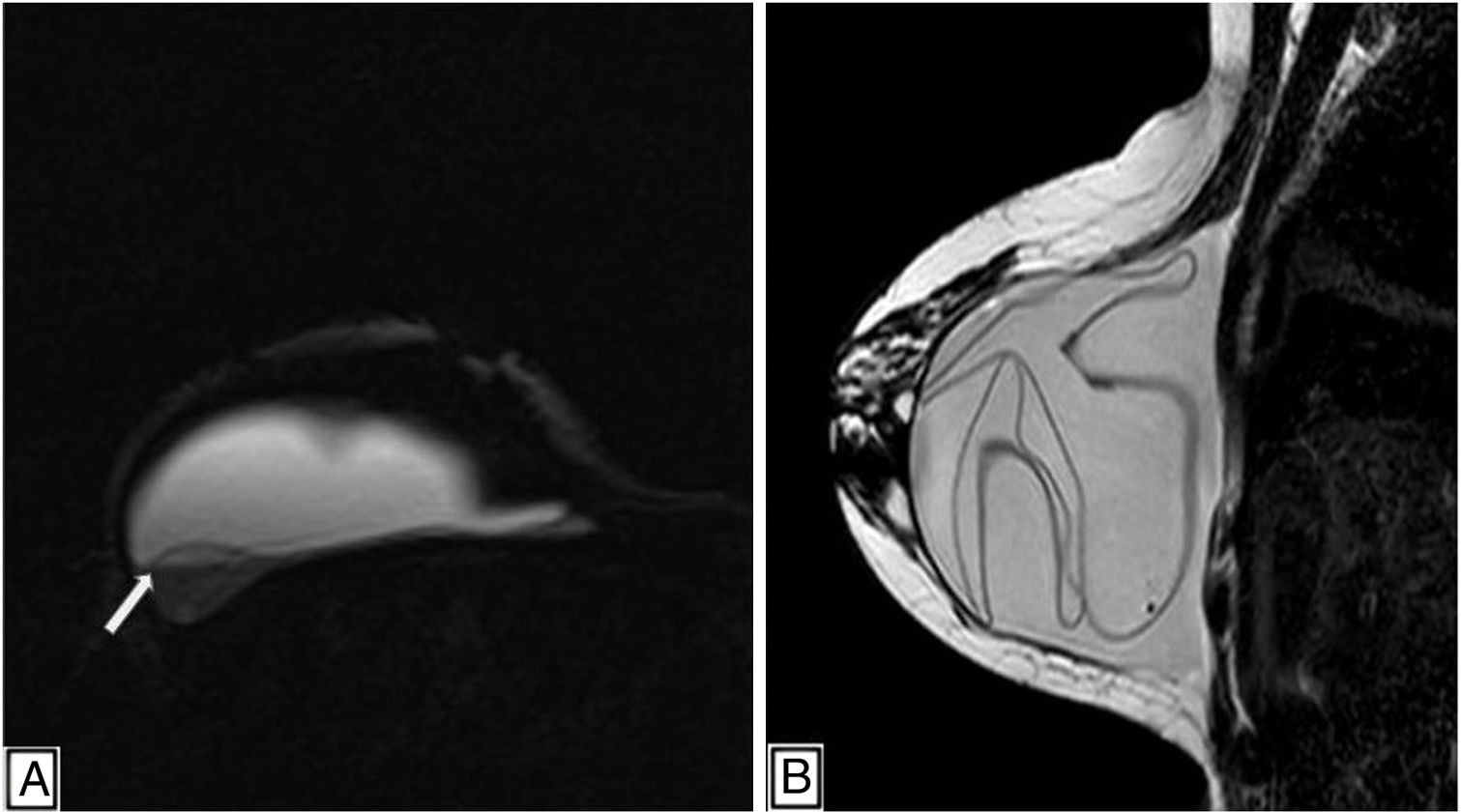
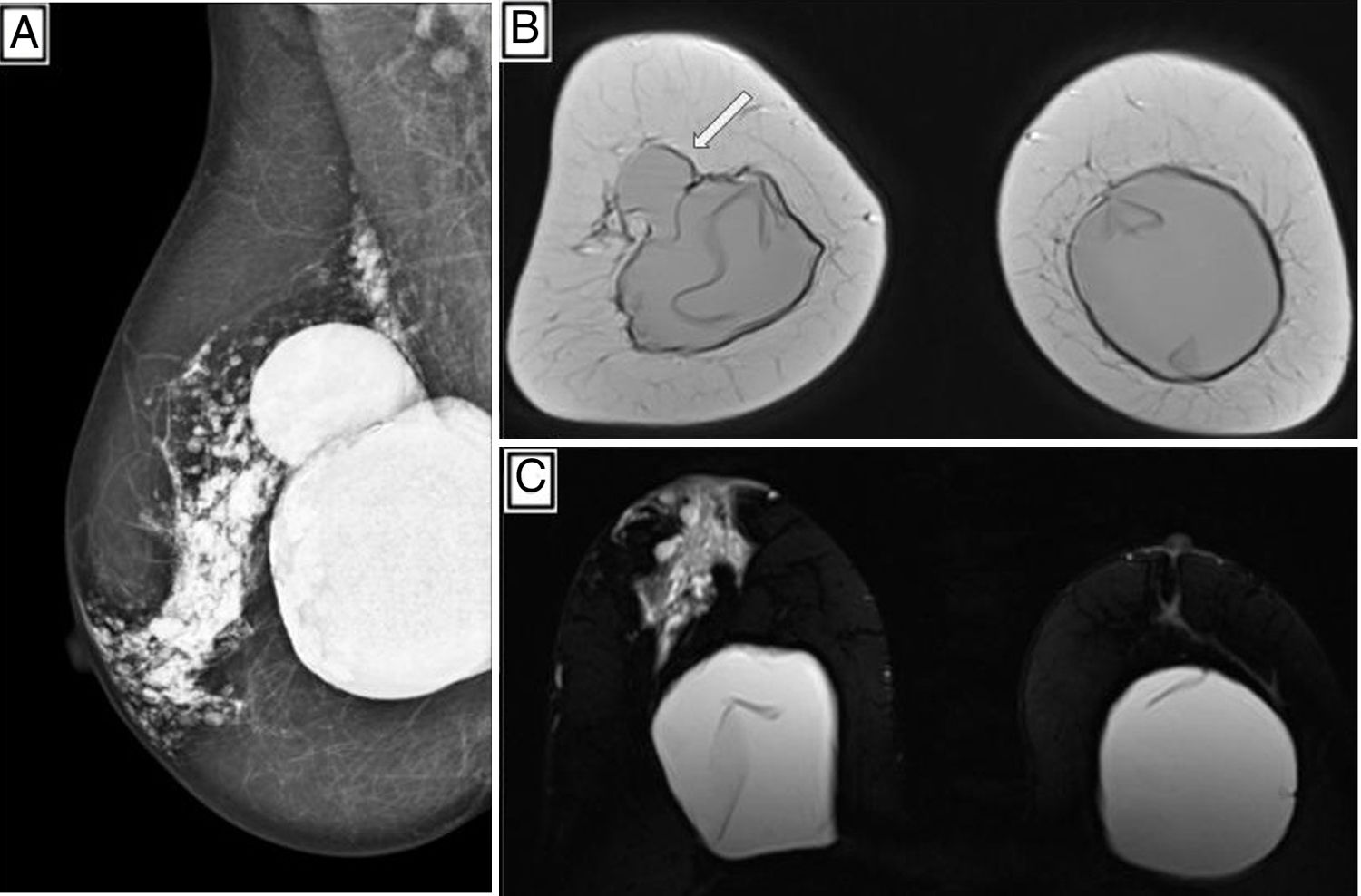
Among the patients, 42% (87/205) showed signs of implant rupture on ultrasound and 42.92% (88/205) showed signs of implant rupture on MRI (Figs. 4–6).
(A) MLO mammographic view of right breast with multiple hyperdense nodular images in the central region and towards the posterior plane. (B) MRI: Coronal T2-weighted sequence. Herniation of the right implant towards the UOQ (white arrow). (C) Bilateral ICR. MRI: Axial silicone-only sequence with hyperintense images in the central region of the breast extending towards the nipple, as a sign of ECR. MLO: mediolateral oblique; UOQ: upper outer quadrant.
MRI showed unilateral rupture in 43 patients (48.86%) and bilateral rupture in 45 patients (51.13%). Meanwhile, in the ultrasound examinations, 51 patients (58.62%) with unilateral rupture and 36 patients (41.38%) with bilateral rupture were registered.
There was good correlation between the two methods in detecting implant rupture, as this was found in 87 patients in ultrasound examinations and in 88 patients in MRI examinations, with a correlation of 0.73 (p < 0.0001).
Good correlation was also observed between the two methods in terms of type of rupture detected.
Of the 50 cases of ICR detected on MRI, 44 were also found on ultrasound examinations. Similarly, the finding of combined (intracapsular and extracapsular) rupture showed good correlation between the two methods. Ultrasound detected combined rupture in 43 patients and MRI detected the same in 38 of them [0.77 (p < 0.0001)] (Fig. 7).
DiscussionDue to its sensitivity and specificity, MRI has become the study of choice in detecting implant rupture. However, the lack of availability of MRI at many centres has rendered breast ultrasound the leading method of evaluation of implant integrity.9,11,14
According to the results obtained, it can be affirmed that both ultrasound and MRI are excellent methods for evaluating implant integrity. These results were consistent with those published by other working groups.9,13,15,16 MRI proved to be the method with the greatest power of discrimination for findings of ICR and ECR.
We found that ultrasound and MRI had high concordance in the detection and laterality of findings of rupture, as well as in the type of rupture found (ICR and ECR).
The percentages of implant rupture found in our series were approximately 42% for each of the techniques used. However, the results in the scientific literature have shown extreme variability (between 0% and 71%), which can be attributed to implant placement time, among other factors.17
The primary objective of this study was to report findings related to signs of breast implant rupture. However, there may be differential diagnoses other than rupture. Some examples are infection, seroma and even, in some cases, breast parenchyma disease not related to the presence of implants. In these cases, ultrasound, as a dynamic study, can contribute valuable information and have advantages over MRI with regard to cost, availability and accessibility.5,12,18,19
Although one of the weaknesses of breast ultrasound as a diagnostic method is its operator dependence, it should be noted that our analysis did not find any statistically significant differences in the number of patients with a diagnosis of implant rupture on ultrasound and on MRI. This may be explained by the fact that the team of specialists in our study belongs to a specialised unit exclusively dedicated to breast diagnosis that has uniform diagnostic criteria and holds regular update meetings.20
We believe that ultrasound is a very useful tool in implant evaluation, and the sensitivity and specificity obtained in this series support this belief. We did not find any references for comparison in the literature.
Our series did not find any association between symptoms and implant rupture — an association that has been reported in the majority of the series reviewed.4 Prior publications that also evaluated implant integrity reported that common reasons for studies in patients with implants are pain and a history of recent trauma.21,22 This is inconsistent with our series, in which these patients represented only 27.8% of the sample (57/205).
This difference could be attributed to the fact that the population enrolled in other studies was symptomatic, whereas 72.19% of the patients included in our sample were asymptomatic (148/205).10,21,22 These results indicate that symptoms and a history of trauma are insufficient variables as a sole reason for suspecting rupture.
Axillary lymph node hyperintensity on MRI or snowstorm signs in the lymph nodes on ultrasound, interpreted as silicone infiltration when seen as an isolated finding, did not prove useful for determining implant integrity.
Silicone may be found in the lymph nodes both in patients with intact implants and in patients with damaged implants.18,23 For this reason, the presence of ultrasound findings of silicone in the lymph nodes accompanied by ultrasound findings of normal breast implants, predicts a correlation of normal findings on MRI.
False positives on ultrasound are correlated with echoes caused by folds in implants that are difficult to assess or by reverberation artefacts that simulate ICR.24 Regarding false negatives, ultrasound may show a limitation in ICR assessment if the technical settings of the ultrasound system are not suitably adjusted for implant evaluation. This does not apply to the investigation of ECR.
The main limitation of this study was that only 20 patients had a history of implant replacement and therefore there was no correlation between surgery and findings of rupture.
In conclusion, our results showed high concordance between the two methods for detecting implant rupture, rupture type and rupture location. Breast ultrasound, unlike MRI, is a low-cost, widely available study.
Our results consolidate the role of ultrasound as a first method of evaluation of implant integrity, and propose reserving MRI for cases of uncertain ultrasound diagnosis.
The mere presence of silicone in the lymph nodes is not useful as an isolated finding to determine implant integrity, as it does not indicate rupture.
Authorship- 1.
Responsible for study integrity: GMS, PAG, VLS, MJC, RAS, KAP.
- 2.
Study concept: GMS, PAG, VLS, MJC, RAS, KAP.
- 3.
Study design: GMS, PAG, VLS, MJC, RAS, KAP.
- 4.
Data collection: GMS, PAG, VLS, MJC, RAS, KAP.
- 5.
Data analysis and interpretation: GMS, PAG, VLS, MJC, RAS, KAP.
- 6.
Statistical processing: GMS, PAG, VLS, MJC, RAS, KAP.
- 7.
Literature search: GMS, PAG, VLS, MJC, RAS, KAP.
- 8.
Drafting of the article: GMS, PAG, VLS, MJC, RAS, KAP.
- 9.
Critical review of the manuscript with intellectually significant contributions: GMS, PAG, VLS, MJC, RAS, KAP.
- 10.
Approval of the final version: GMS, PAG, VLS, MJC, RAS, KAP.
The participating researchers declare that they have no conflicts of interest.
This manuscript was evaluated by the Independent Ethics Committee of the Hospital Italiano de Buenos Aires [Buenos Aires Italian Hospital], under Protocol No. 5055.
Please cite this article as: Secco GM, Gutierrez PA, Secco VL, Chico MJ, Secco RA, Pesce KA. ¿Es la ecografía mamaria una buena alternativa a la resonancia magnética en la evaluación de la integridad protésica? Radiología. 2022;64:20–27.