Patients with penetrating wounds with suspected foreign bodies retained in the wound are often seen in emergency departments. Imaging studies are necessary to rule out the presence of retained foreign bodies. Plain-film X-rays, however, are only useful when the foreign bodies contain radiopaque material (metal, glass, stone, and some plastics). In cases with strong diagnostic suspicion and negative plain films, other imaging tests are necessary. Ultrasonography has proven useful in the identification and location of both radiopaque and radiotransparent foreign bodies. Ultrasonography enables excellent assessment of adjacent anatomical structures (muscles, tendons, ligaments, and neurovascular structures) and of associated lesions. The different materials found in foreign bodies have characteristic ultrasonographic patterns that are useful for diagnosis. Finally, it is important to be familiar with the diagnostic pitfalls to avoid false positives.
Los pacientes con heridas penetrantes y sospecha de cuerpos extraños retenidos representan un motivo frecuente de consulta en los servicios de urgencias. Es necesario un estudio radiográfico para descartar la presencia de cuerpos extraños. Sin embargo, las radiografías solo resultan de utilidad en los objetos radiopacos (metal, vidrio, piedra y algunos plásticos). Cuando la sospecha diagnóstica es alta y el estudio radiográfico es negativo, es necesario realizar otras pruebas de imagen. La ecografía ha demostrado su utilidad en la identificación y localización de cuerpos extraños tanto radiopacos como radiotransparentes. La ecografía permite una excelente evaluación de las estructuras adyacentes (músculos, tendones, ligamentos y estructuras neurovasculares) y en la valoración de sus lesiones asociadas. Los diferentes materiales de los cuerpos extraños presentan patrones ecográficos característicos que resultan de utilidad para su aproximación diagnóstica. Por último, es importante estar familiarizado con los potenciales errores diagnósticos para evitar falsos positivos.
A foreign body is defined as any object originating outside the body. Therefore, it can be understood that foreign bodies refer to any body or particle of biological or inert origin, introduced voluntarily or involuntarily into a part of the body to which it does not belong.1,2 Patients with penetrating wounds and suspected retained foreign bodies are a common reason for consultation in accident and emergency departments. The most commonly retained materials found in patients who attend A&E departments are wood, glass and metal.1,3–5 The initial assessment of puncture wounds and soft tissue injuries should always include a detailed medical history with a targeted physical examination, without overlooking the X-ray investigation to rule out the presence of foreign bodies. The objectives of this manuscript include the following: description of the main ultrasound findings of subcutaneous foreign bodies and their characteristics depending on their nature, rapid and systematic identification of associated complications and assessment of the main diagnostic errors in the ultrasound assessment of foreign bodies.
Imaging techniquesX-rayX-rays are useful to demonstrate the existence of radiopaque materials such as glass, metal, stone and some plastics. Both plant-based bodies and wood may be radiolucent and, therefore, difficult to identify in X-rays.1,4–7 Up to 38% of retained foreign bodies are missed in the initial examination performed in the A&E department.1,2,5,8 Less than 15% of wooden foreign bodies are seen in X-rays.3,5,8,9
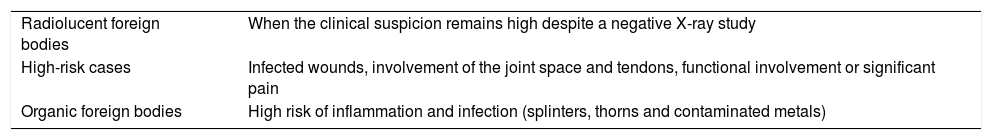
UltrasoundWhen the clinical suspicion of a retained foreign body is high and the X-ray study has come back negative, other imaging tests should be performed. Ultrasound has shown that it has high sensitivity and specificity for identifying and locating both radiopaque and radiolucent foreign bodies.2–5,7,8 High-frequency linear transducers (7.5MHz or more) are needed for the ultrasound examination. Despite its usefulness for the diagnosis, correlation between the ultrasound and X-rays is always recommended. Ultrasound is particularly useful in cases in which the retained foreign body is not seen on the X-ray study, as well as in high-risk cases (primarily infected wounds and functional involvement) and for cases of splinters, thorns and contaminated metals (Table 1).3,9–12 Furthermore, the role of ultrasound is not only limited to diagnosis, as it is also very widely used in the extraction of foreign bodies.13–15 The detection and removal of retained subcutaneous foreign bodies is important due to the risk of superinfection.1,3,6
When is it necessary to perform an ultrasound study?
| Radiolucent foreign bodies | When the clinical suspicion remains high despite a negative X-ray study |
| High-risk cases | Infected wounds, involvement of the joint space and tendons, functional involvement or significant pain |
| Organic foreign bodies | High risk of inflammation and infection (splinters, thorns and contaminated metals) |
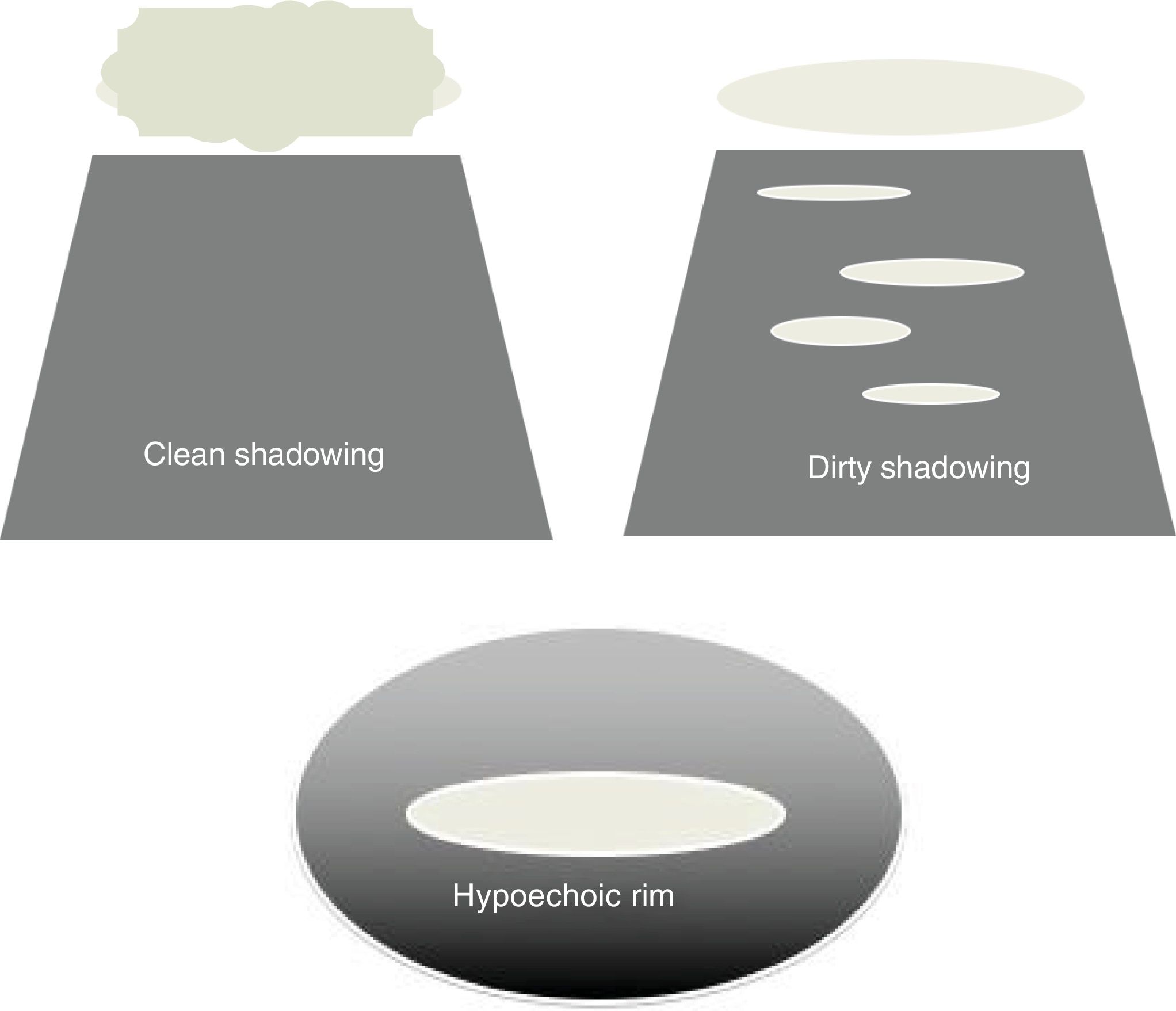
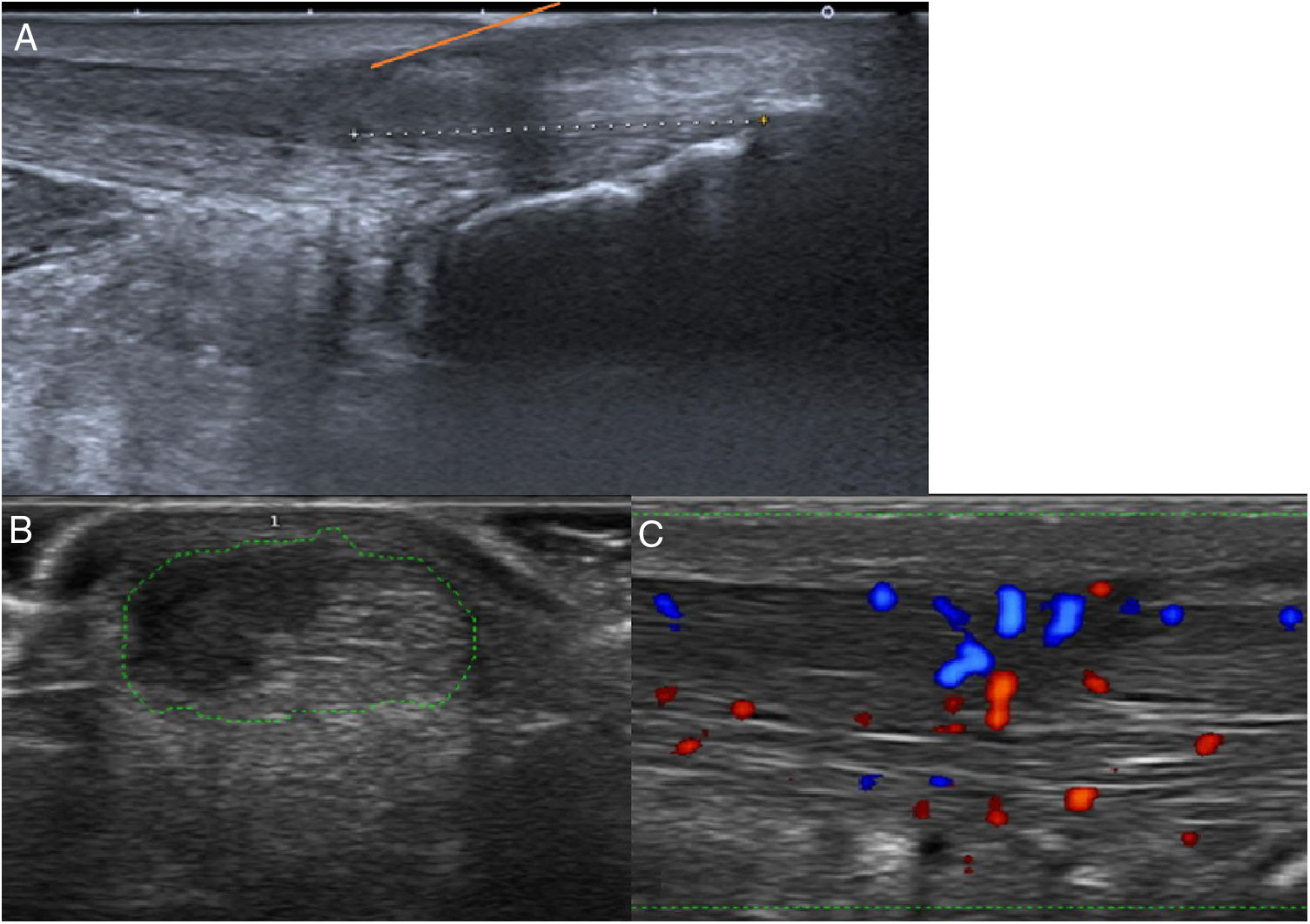
It has been observed that the different materials studied present characteristic ultrasound patterns which are useful for their differentiation.1,3,9 Most foreign bodies present a characteristic linear form and should be viewed both in the long and in the short axis. If doubts arise regarding their existence, it is always recommended to compare with the contralateral side. All foreign bodies appear hyperechogenic compared to adjacent soft tissues.1–3,6 Some of them show artefacts such as posterior acoustic shadowing, reverberation and/or surrounding hypoechoic rim.1,2,6,9 These ultrasound artefacts may be useful to facilitate identification of the foreign bodies. The ultrasound artefacts depend on the characteristics of the foreign body, in particular the appearance of posterior acoustic shadowing (Fig. 1). Objects with a rough and uneven surface create clean posterior acoustic shadowing, while those that have a smooth and flat surface will generate dirty shadowing with reverberation. It is important that the ultrasound beam falls directly onto the object to maximise the acoustic shadowing artefact. In addition, during the ultrasound study, a surrounding hypoechoic rim corresponding with the associated inflammatory process, which normally develops 24h after the penetration of the foreign body, is often seen. The hypoechoic rim may be caused by oedema, abscess or granulation tissue (Fig. 1). This artefact improves sensitivity and specificity in the detection of foreign bodies by ultrasound.3,8
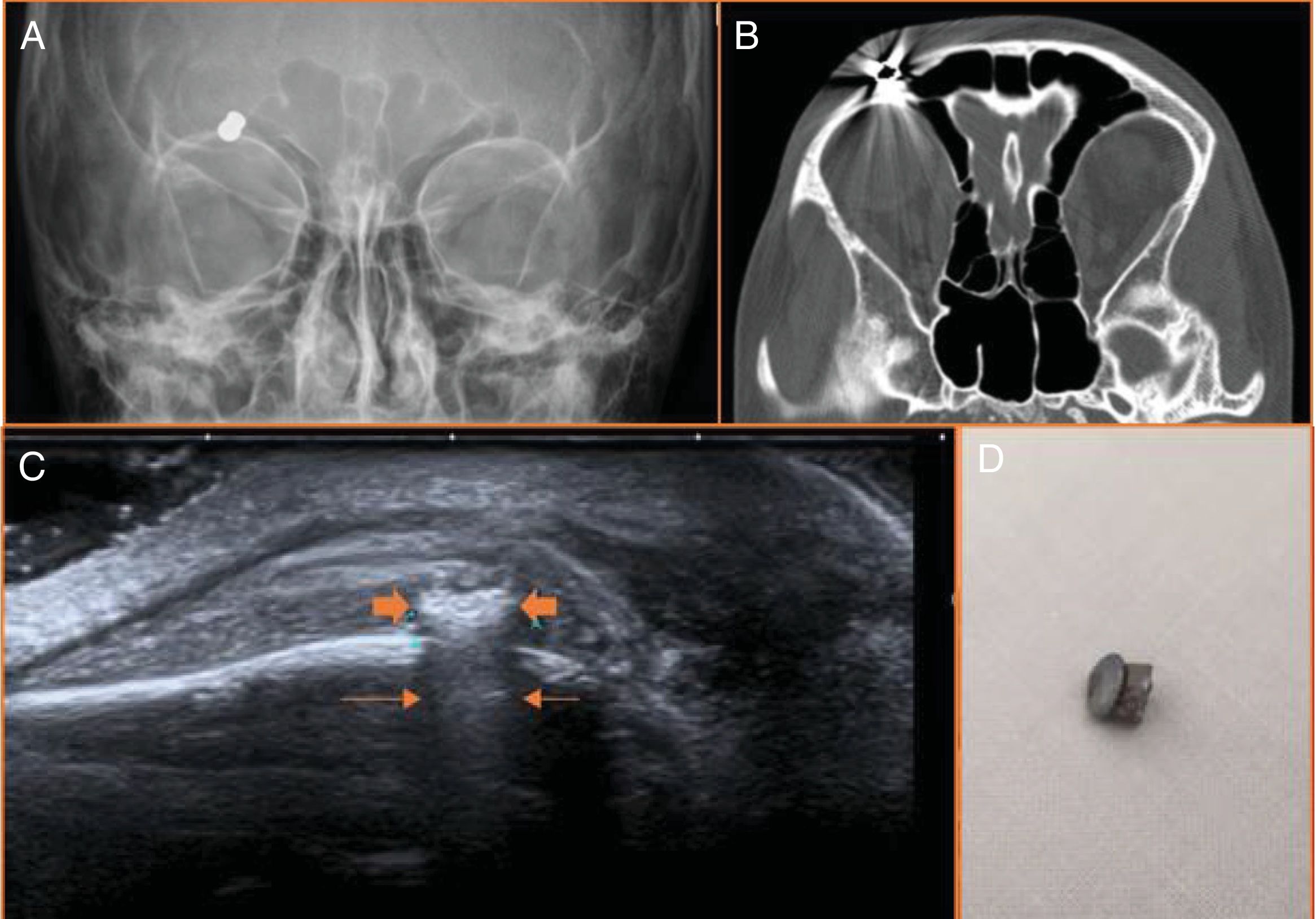
Radiological evaluation of foreign bodies according to their compositionMetalDetection with X-rayMetal objects are detectable in X-rays (Fig. 2). However, the usefulness of X-rays to determine the exact location of radiopaque foreign bodies, their relationship with surrounding structures and the degree of injury of the adjacent soft tissues is limited.1,3,4,12
12-year-old boy with a metal foreign body in the right supraorbital region compatible with a pellet. (A and B) The pellet is radiopaque and easily identifiable ox X-rays and in computed tomography. (C) On ultrasound it is markedly echogenic (thick arrows), with reverberation artefact (thin arrows) and limited associated inflammatory changes (hypoechoic rim).
Metal objects are highly hyperechogenic and generate a comet-tail artefact or reverberation due to their smooth surface (Fig. 2).1,3,8,9
GlassDetection with X-rayGlass is detectable by X-ray. It used to be thought that the visualisation capacity of glass objects on X-rays depended on their lead content. However, it is not necessary for glass to contain lead to be radiopaque, due to the fact that its density (2.4–2.8mg/ml) is greater than that of the soft tissue (1.5mg/ml). Chemically, commercial glass is produced from inorganic oxides, of which silica (sand) is generally the main component. The most common glass objects are glasses, bottles and light bulbs. They do not contain lead, but are radiopaque on X-rays (Fig. 3).3,9
Ultrasound characteristicsGlass foreign bodies are hyperechogenic and sometimes present a reverberation artefact (Fig. 3).3,8,9
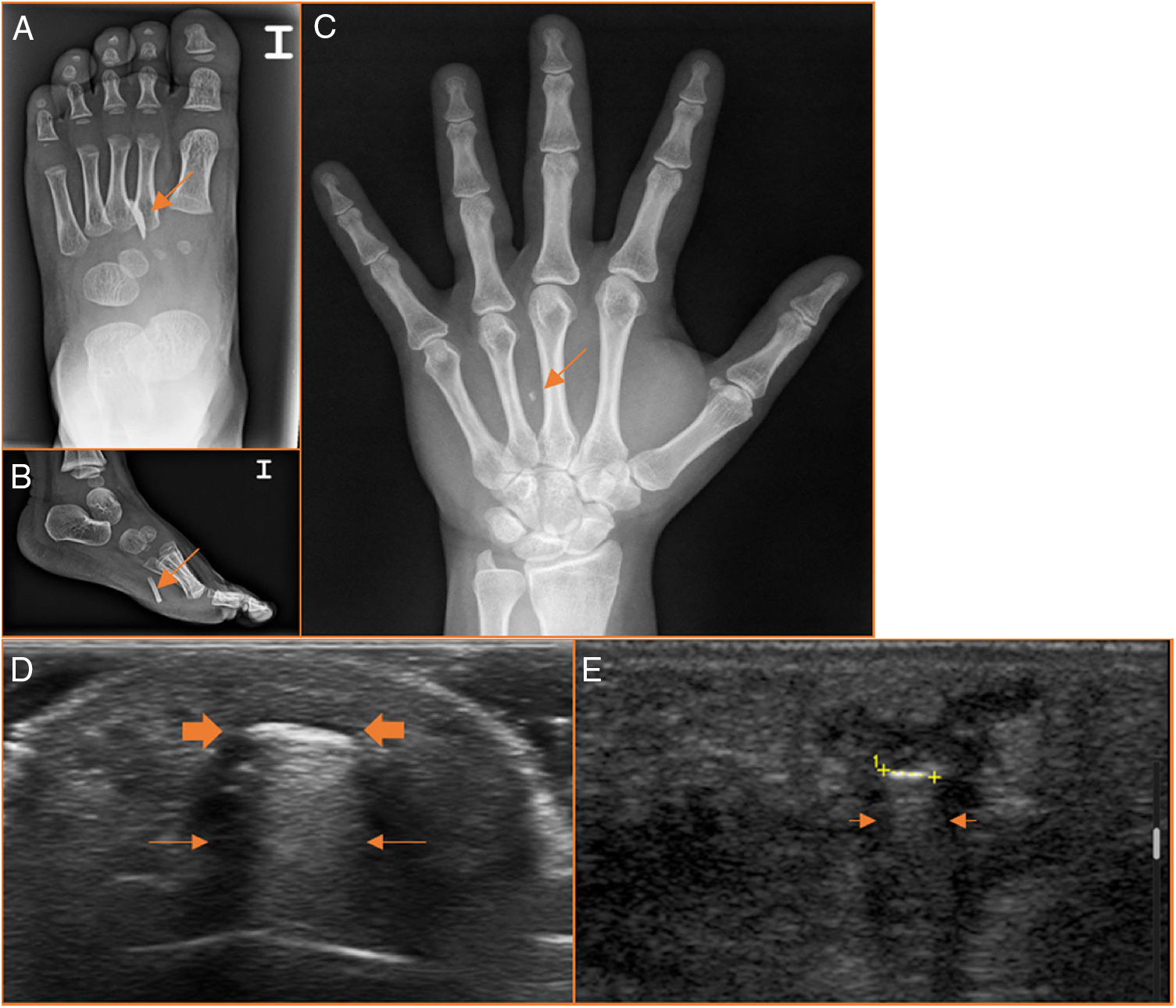
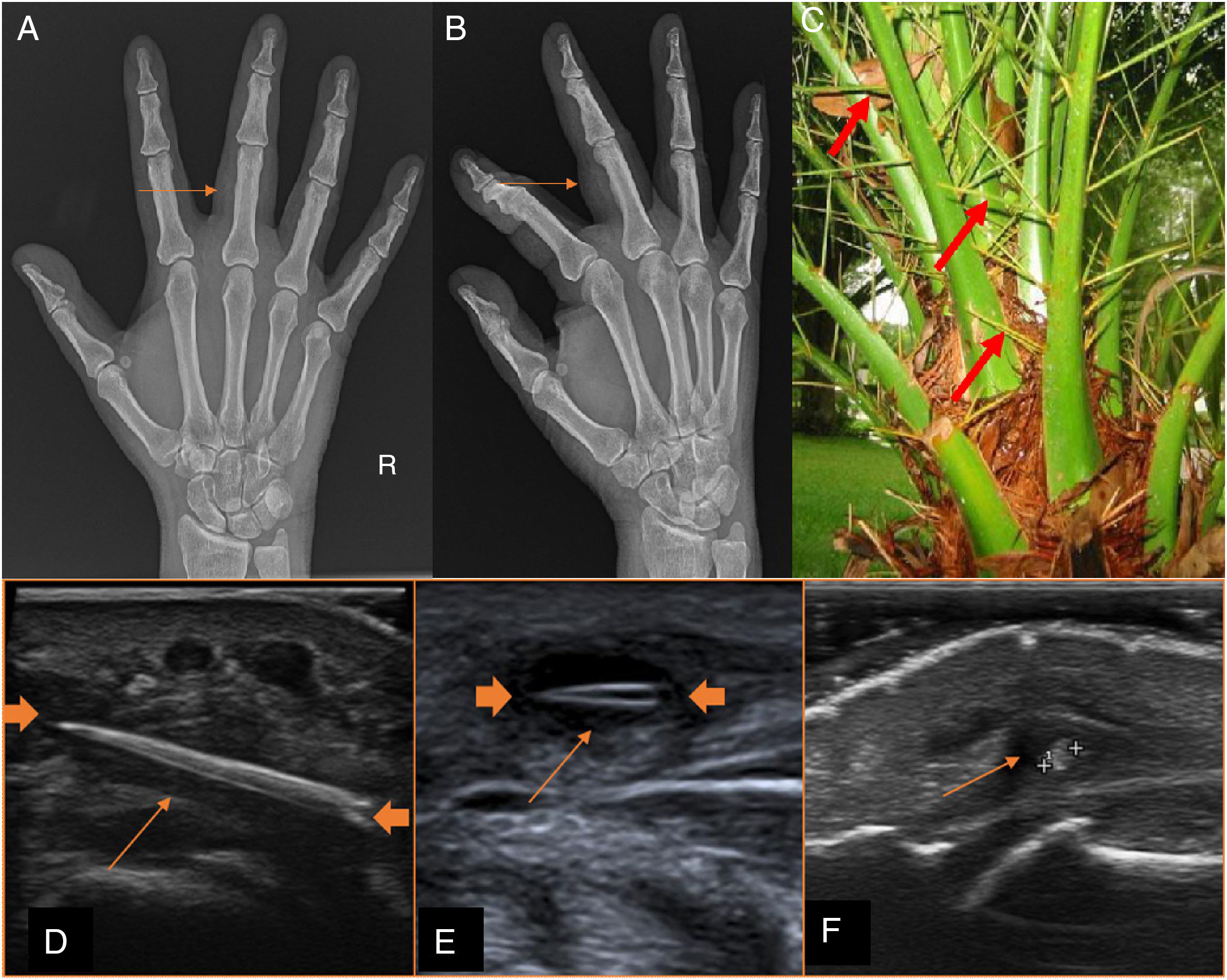
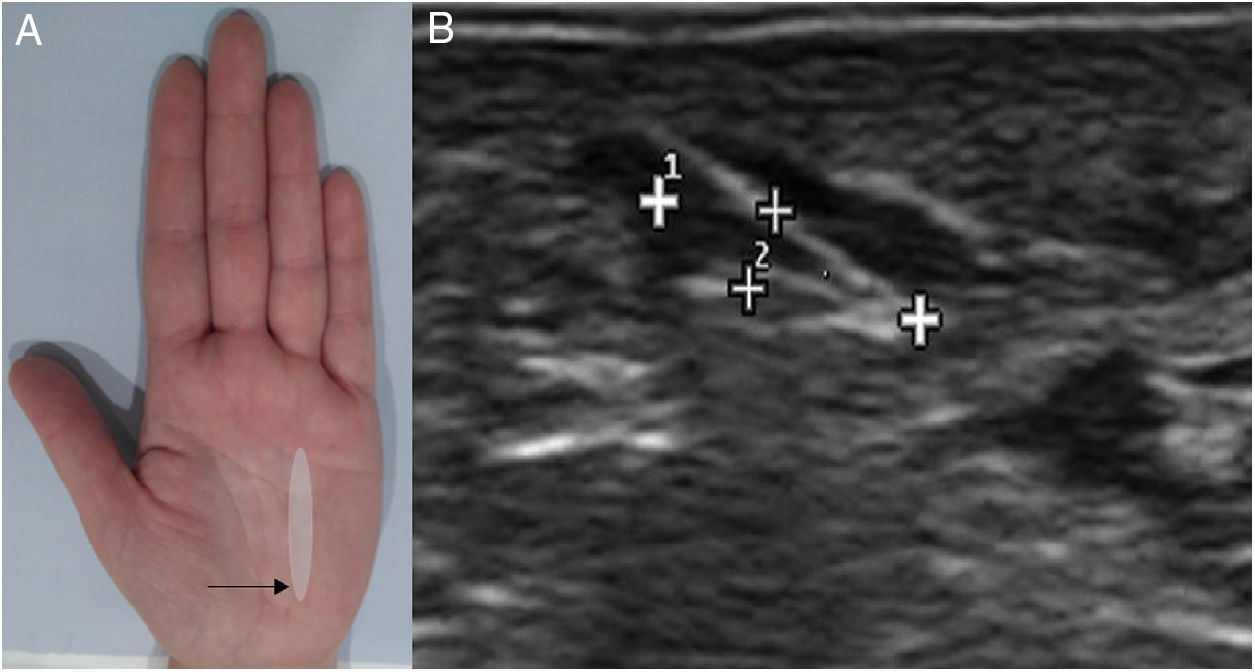
Plant-basedDetection with X-rayWooden splinters and thorns from different plants are not visible on X-rays (Fig. 4).16–19 They can only be suspected due to the increase of associated soft tissue.
Plant-based foreign bodies are radiolucent. (A and B) The palm tree thorn is not visible on X-ray, but there is an increase of soft tissue (arrows) in the proximal phalanx of the third finger. (D–F) On ultrasound, they are slightly hyperechogenic (thick arrows in D and E) and their echogenicity reduces over time (cursors in F). The surrounding hypoechoic rim is very pronounced in plant-based foreign bodies (thin arrows).
Splinters and thorns are generally hyperechogenic, although less so than the other foreign bodies already discussed. They present deep posterior acoustic shadowing and of variable density (Fig. 4).17,20,21 Wood and other organic foreign bodies lose echogenicity over time.3,16,19 The secondary inflammatory process, reflected in the surrounding hypoechoic rim and the increase of the Doppler signal, is more evident and develops more quickly with organic materials (plants, wood) and with contaminated inorganic materials (metal, glass).3,16,20
Other foreign bodies, such as plastic, appear hyperechoic with posterior acoustic shadowing. Sand and gravel (Fig. 5) produce marked posterior acoustic shadowing (such as cholelithiasis).3,9
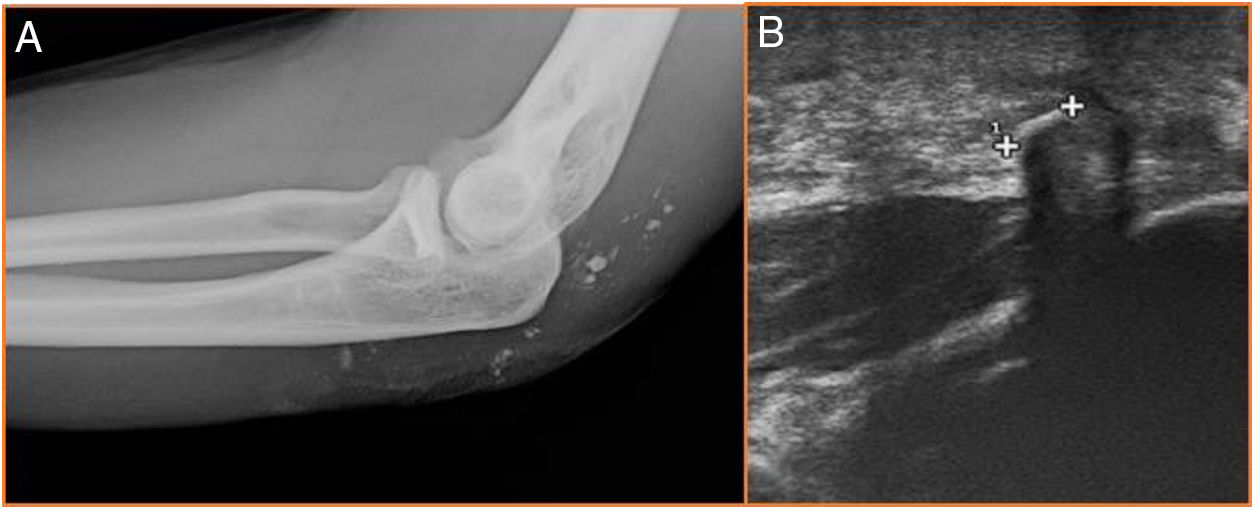
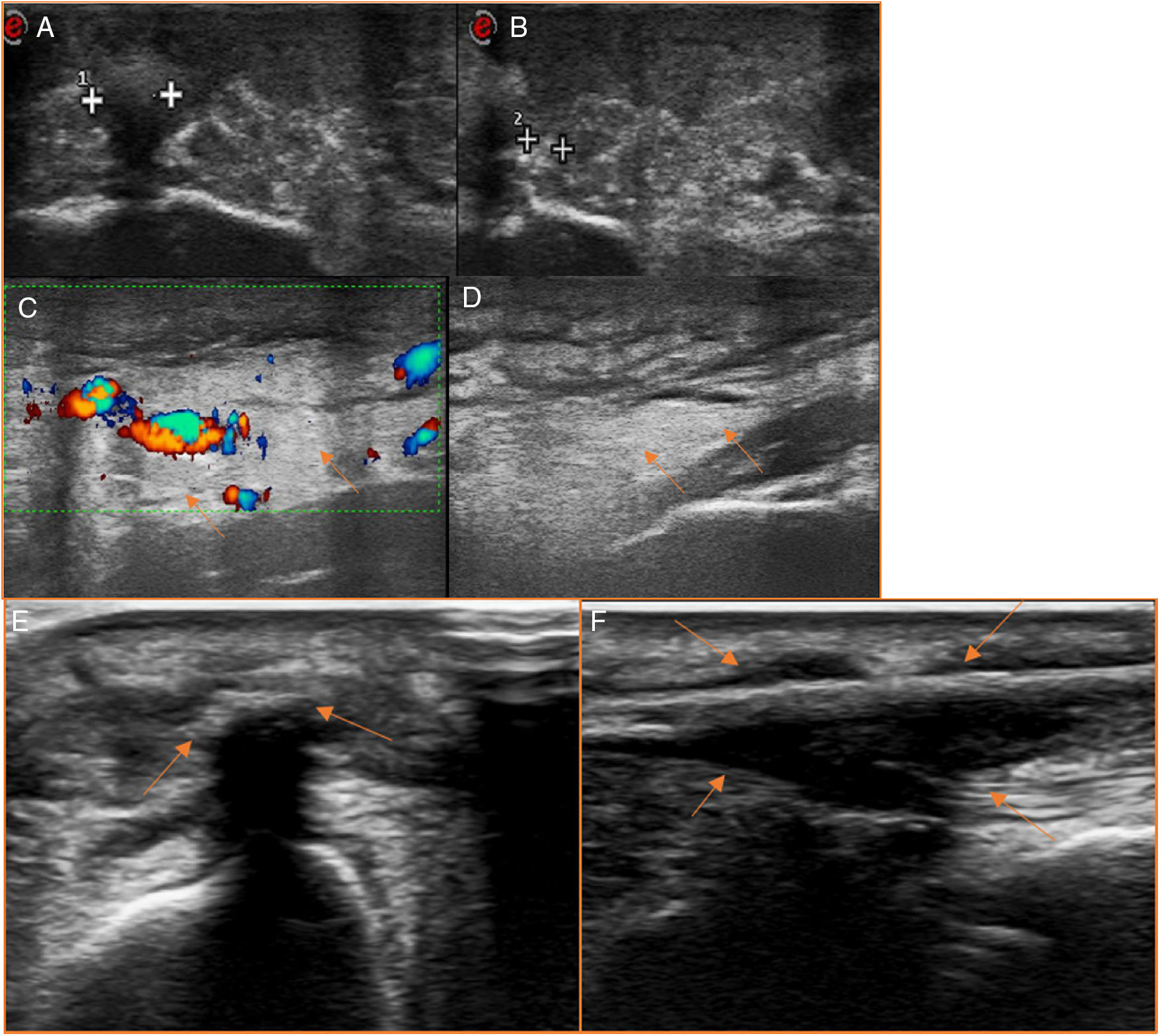
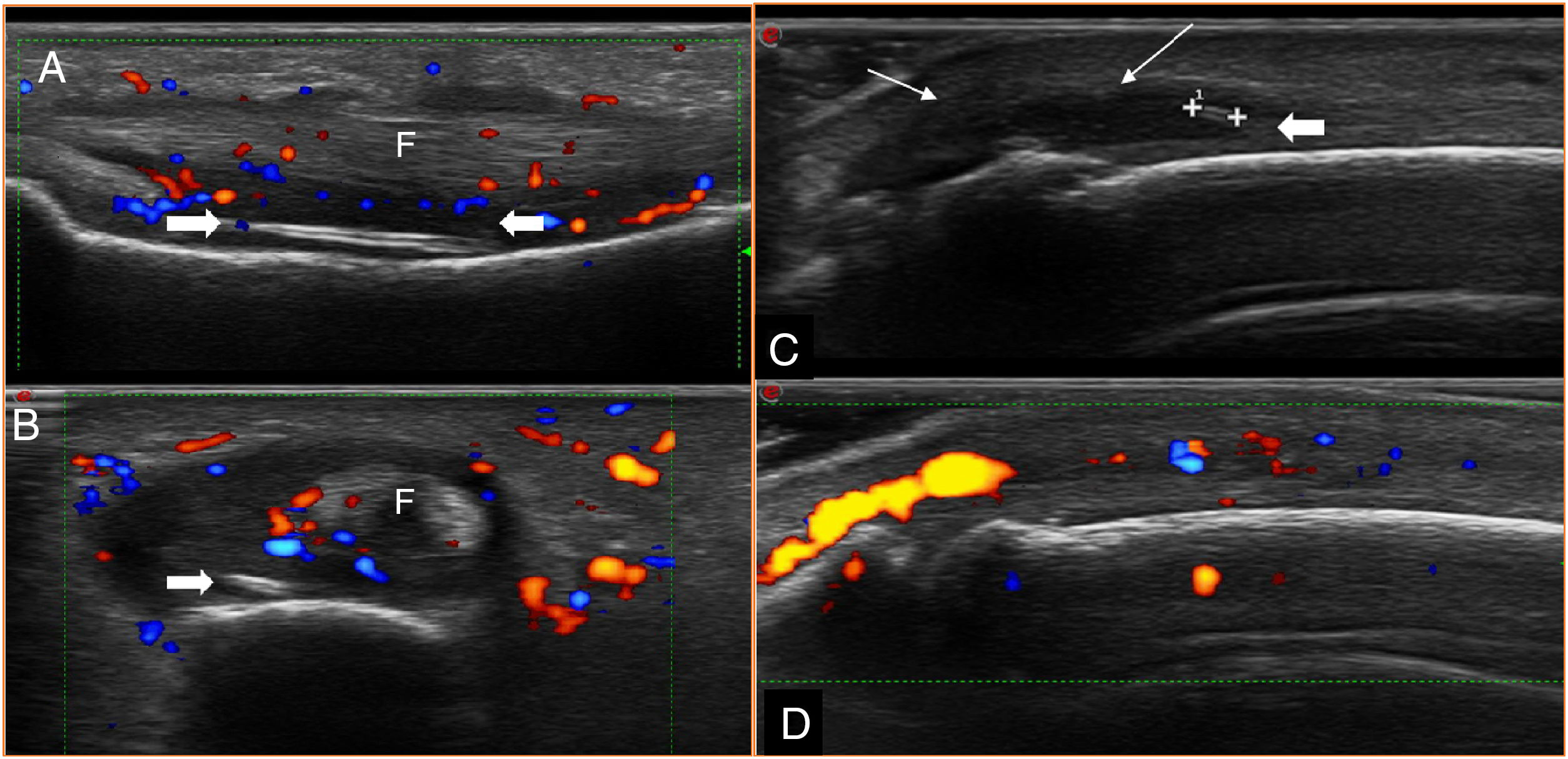
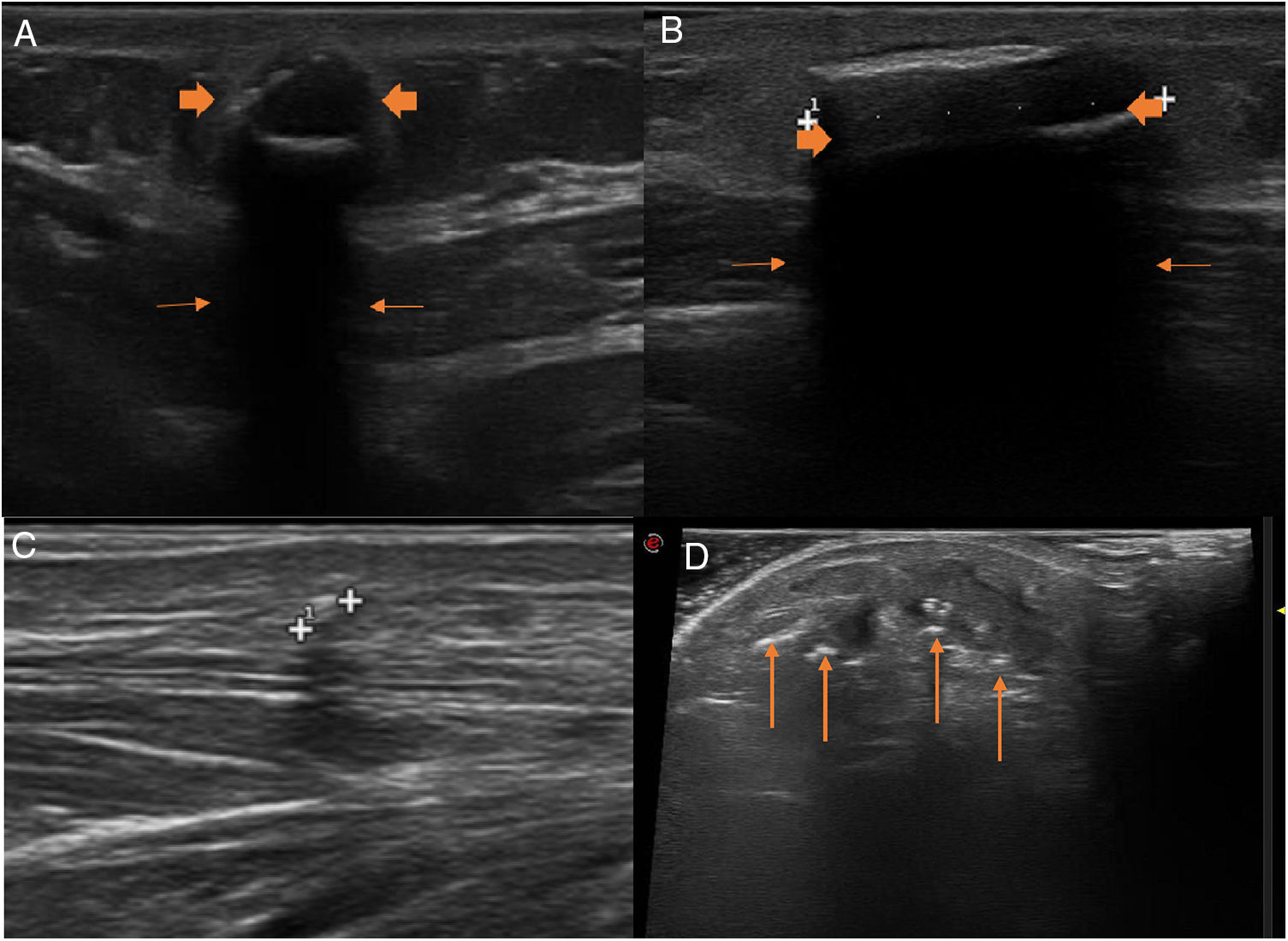
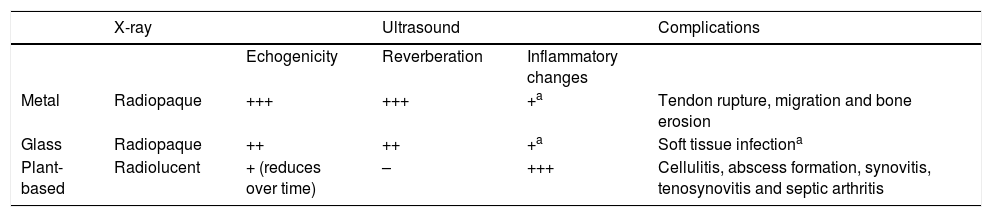
Associated complicationsAssociated complications depend on the depth and location of the foreign body. The ultrasound examination allows for excellent visualisation and assessment of the adjacent structures of the foreign body (subcutaneous cell tissue, muscles, tendons, ligaments and neurovascular structures). The main complications associated with the existence of a retained object are as follows: cellulitis, formation of abscesses, tenosynovitis, rupture of tendons, septic arthritis, bone erosion and migration.22–26 Cellulitis is the most commonly found complication.3,9,27 Infection can occur as a result of development of an abscess, which will appear as an anechoic collection on ultrasound, with increased Doppler signal in the periphery. Furthermore, air bubbles can be detected within the soft tissue or abscesses in cases of infection due to gas-producing microorganisms. It has been observed that some of the complications mentioned tend to be associated with some foreign bodies of specific materials. For example, inflammation and infection of the adjacent soft tissue are more significant when the foreign body is organic, i.e. plant-based, or even when it is a contaminated metal: cellulitis (Fig. 6), formation of abscesses (Fig. 6), tenosynovitis (Fig. 7), septic arthritis (Fig. 7). A resistant and hard material, such as metal, is needed to cause bone erosion. Tendon ruptures tend to be associated with foreign bodies from metal and glass (Fig. 8). Migration, a rare phenomenon, has been described mainly in metal and glass materials, although there are also published cases of palm tree thorns and toothpicks (Fig. 9).22,27–29 The following table summarises the main characteristics of subcutaneous foreign bodies in X-ray and ultrasound, as well as their associated complications (Table 2). The optimal time window for the treatment of subcutaneous objects is within the first 24h. Within this time frame there is better visualisation of the injuries from the entry and/or exit of the foreign body, thanks to the lower degree of inflammation, induration and scarring.14,15 A delay in the treatment may cause complications, such as infections, healing problems and loss of function in the most severe cases. It is also necessary to consider that attempts to extract the foreign bodies can cause increased tissue inflammation, migration or retention of the foreign bodies, infection, and vascular and nerve damage.
Infectious complications. (A–D) Cellulitis on the posterior side of the elbow (arrows in C and D) due to the presence of retained gravel in the subcutaneous cell tissue (cursors in A and B) after a motorbike accident. (E and F) Wooden splinter (arrows in E) on the dorsal side of the wrist associated with the formation of an abscess (arrows in F).
Wooden splinter (thick arrows) within the flexor tendon (F) of the third finger, which causes tenosynovitis in the longitudinal (A) and short (B) axes. (C and D) Palm tree thorn (thick arrow) in the interphalangeal joint of the third finger that causes septic arthritis (thin arrows) both in the longitudinal axis (C) and in the short axis (D), which is characterised by the presence of joint effusion with increased surrounding vascularisation in the colour Doppler.
Partial rupture of the Achilles tendon by a cut with a glass bottle (not shown). (A) Changes in the soft tissue one week after the accident (the orange line indicates the route of the glass). Figures B (short axis) and C (long axis) show the changes in the tendon one month after the accident.
48-year-old woman with a history of a cut with a glass bottle 6 years ago. The patient reported that the small lump secondary to the accident had changed location within her palm over time. (A) Route of migration of the foreign body (thin arrow: final location). (B) Small piece of glass retained for years (cursors).
Foreign bodies: differentiating features.
| X-ray | Ultrasound | Complications | |||
|---|---|---|---|---|---|
| Echogenicity | Reverberation | Inflammatory changes | |||
| Metal | Radiopaque | +++ | +++ | +a | Tendon rupture, migration and bone erosion |
| Glass | Radiopaque | ++ | ++ | +a | Soft tissue infectiona |
| Plant-based | Radiolucent | + (reduces over time) | – | +++ | Cellulitis, abscess formation, synovitis, tenosynovitis and septic arthritis |
There are several ultrasound findings, both normal and pathological, which may mimic the presence of a foreign body, resulting in false positives. The diagnostic errors most commonly found during ultrasound assessment are the following: calcifications, sesamoid bones, scar tissue, acute haematomas, intermuscular septa, hyperechogenic muscle fibres and air trapped in the soft tissue. All these findings can interrupt the normal and homogeneous echotexture of the soft tissue and this is where its importance lies as potential sources of error. Calcifications and sesamoid bones (Fig. 10) typically appear as echogenic foci accompanied by significant posterior acoustic shadowing. Scar tissue, in particular fibrosis secondary to traumas or prior surgery, may result in the suspicion of the presence of small foreign bodies in the skin and in the subcutaneous cell tissue. Haematomas, according to the oldest scientific literature, can be confused with foreign bodies given that they have a variable echogenicity depending on the phase in which they are found. When haematomas have a solid appearance, they can give rise to diagnostic errors. However, in our experience, with current ultrasound machines and in expert hands, they are not a cause of false positives. Intermuscular septa (Fig. 10) represent a challenge in ultrasonography and can often mimic the presence of a foreign body, especially in the smallest and most complex regions of the body, such as the hands and the feet. In these locations, the interruption of the normal echotexture is less useful as an indicator for the detection of foreign bodies. One of the biggest limitations in the ultrasound assessment of retained foreign bodies occurs in the surgical assessment of the wound prior to performing the ultrasound. In these cases, air may enter the adjacent tissue, very significantly limiting the visualisation of the object and generating false images (Fig. 10).1,3,9
Potential diagnostic errors in ultrasound. In a patient with a recent history of cardiopulmonary resuscitation, the presence of a superficial lump on the left floating ribs was observed. In light of a suspected retained foreign body, an ultrasound was performed where the chondral fragment of the 10th rib (thick arrows) was observed both in the short (A) and longitudinal (B) axes, accompanied by significant posterior acoustic shadowing (thin arrows). (C) The intermuscular septa can hinder the identification of a foreign body (cursors), and even mimic it, particularly if the wound is recent and the hypoechoic rim is not yet present. (D) Patient with rupture of the tibialis anterior muscle with a plate in whom a surgical review of the wound was performed. On the ultrasound, distal bubbles were found in the subcutaneous cell tissue, limiting the visualisation of the foreign body and generating false images.
Ultrasound has been proven to be the best tool for the diagnosis of superficial foreign bodies, which translates into faster access to treatment and, therefore, a lower risk of associated complications. In our experience, familiarity with the ultrasound appearance of the different retained objects according to their composition may help the diagnostic approach. Systematic evaluation of the potential associated complications is crucial to avoid delays in treatment. In addition, ultrasound can also help in the removal of retained subcutaneous foreign bodies.
AuthorshipResponsible for the integrity of the study: EMD, EGA.
Study conception: EMD, EGA.
Study design: EMD, EGA, RMLÁ.
Data collection: EMD, ALO, RL, MPE, EGA.
Data analysis and interpretation: EMD, EGA, MPE, ALO.
Statistical processing: not applicable.
Literature search: EMD, ALO.
Drafting of the paper: EMD, ALO, RMLÁ, MPE.
Critical review of the manuscript with intellectually relevant contributions: EMD, EGA, RMLÁ, ALO, MPE.
Approval of the final version: EMD, EGA, RMLÁ, ALO, MPE.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Marín-Díez E, Landeras Álvaro RM, Lamagrande Obregón A, Pelaz Esteban M, Gallardo Agromayor E. Ecografía de los cuerpos extraños subcutáneos: diferencias según naturaleza, complicaciones y potenciales errores diagnósticos. Radiología. 2020;62:3–12.