Initial studies have shown that old occlusions or those with indeterminate occlusion duration have been associated with percutaneous coronary intervention (PCI) failure and a worse prognosis. This study aimed to determine the impact of occlusion duration on the success and outcomes of contemporary PCI on chronic total occlusion (CTO).
MethodsThe authors analyzed a retrospective cohort of consecutive patients submitted to PCI in CTO, who were compared according to the confirmed occlusion duration (COD) < 12 months, ≥ 12 months, or indeterminate occlusion duration (IOD).
ResultsA total of 168 patients were treated, 122 (72.6%) with COD (80 < 12 months, 42 ≥ 12 months) and 46 (24.7%) with an IOD. Lesion extension was 17.0 ± 13.6mm, in 2.90 ± 0.58mm vessels, and the anterograde approach was used in 98.8% of cases. Angiographic success was attained in 79.2% of patients (80.0% vs. 73.8% vs. 82.6%; p = 0.73). The main cause of failure was the inability to cross the lesion with the guidewire (68.6%). Occlusion duration had no impact on in-hospital events (4.8% vs. 7.1% vs. 6.0%; p = 0.73), which were almost entirely explained by periprocedural myocardial infarction, or on late outcomes (18.8% vs. 7.1% vs. 15.3%; p = 0.23). At the multivariate analysis, lesion length ≥ 20mm (odds ratio - OR = 7.27; 95% confidence interval - 95% IC 1.94-29.1; p = 0.003), calcification (OR = 4.72; 95% CI 1.19-19.1; p = 0.02), and tortuosity of the occluded segment (OR = 15.98; 95% CI 2.18-144.7; p = 0.007) were predictors of failure.
ConclusionsOcclusion duration was not associated with increased failure rate of the procedure or worse PCI outcomes in CTO.
Estudos iniciais mostram que oclusões antigas ou com tempo indeterminado têm sido associadas a insucesso da intervenção coronária percutânea (ICP) e a pior prognóstico. Nosso objetivo foi determinar o impacto do tempo de oclusão no sucesso e nos resultados da ICP contemporânea na obstrução total crônica (OTC).
MétodosAnalisamos uma coorte retrospectiva de pacientes consecutivos que realizaram ICP em OTC, e que foram comparados de acordo com o tempo de oclusão confirmado (TOC) < 12 meses, ≥ 12 meses, ou indeterminado (TOI).
ResultadosForam tratados 168 pacientes, 122 (72,6%) com TOC (80 < 12 meses, 42 ≥ 12 meses) e 46 (24,7%) com TOI. A extensão da lesão foi de 17,0 ± 13,6mm, em vasos de 2,90 ± 0,58mm, e a abordagem anterógrada foi utilizada em 98,8% dos casos. Sucesso angiográfico foi obtido em 79,2% dos pacientes (80,0% vs. 73,8% vs. 82,6%; p = 0,73). A principal causa de insucesso foi a incapacidade de cruzar a lesão com o fio-guia (68,6%). O tempo de oclusão não teve impacto na taxa de eventos cardiovasculares hospitalares (4,8% vs. 7,1% vs. 6,0%; p = 0,73), explicados em sua quase totalidade pelos infartos do miocárdio periprocedimento, ou nos eventos tardios (18,8% vs. 7,1% vs. 15,3%; p = 0,23). Na análise multivariada, comprimento da lesão ≥ 20mm (odds ratio - OR = 7,27; intervalo de confiança de 95% - IC 95% 1,94-29,1; p = 0,003), calcificação (OR = 4,72; IC 95% 1,19-19,1; p = 0,02) e tortuosidade do segmento ocluído (OR = 15,98; IC 95% 2,18-144,7; p = 0,007) foram preditores de insucesso.
ConclusõesO tempo de oclusão não está associado ao aumento da taxa de insucesso do procedimento ou a piores resultados da ICP em OTC.
Chronic total occlusion (CTO) is found in approximately 15 to 30% of patients referred for elective coronary angiography.1 However, percutaneous coronary intervention (PCI) for CTO corresponds to only 10% of the total procedures2,3 and remains one of the most challenging interventions in the field. In fact, the number of percutaneous procedures in CTO has remained stable in recent years,4 despite the development of new techniques such as the retrograde approach, the use of new dedicated devices, and the increased experience of interventionists, resulting in increasingly higher success rates.5–8 It is known that a myocardial area irrigated by an occluded artery may be associated with persistent ischemia, even in the presence of well-developed collaterals,9 and that the successful revascularization of the lesion is associated with reduced ischemic burden and improved ventricular contractility.10 Studies have shown the improvement in late prognosis of patients submitted to successful PCI compared to those with procedural failure.11–14 The main reason for this failure is the inability to cross the lesion with the guidewire or the balloon. Initial studies have shown that a long occlusion duration is associated with failure of the technique.15,16 Similarly, an indeterminate occlusion duration (IOD) is also associated with PCI failure.17 Conversely, a more recent study showed no association between the occlusion duration and the success rate of the procedure.18
The aim of this study was to determine the impact of occlusion duration on the success and outcomes of contemporary PCI in CTO.
MethodsStudy populationA retrospective cohort of consecutive patients submitted to PCI in occlusive lesions was assessed from June 2008 to December 2014 in a tertiary cardiology reference hospital linked to the Brazilian Unified Health System (SUS, acronym in Portuguese). After the review of medical records and analysis of coronary angiography, patients who had estimated occlusion duration < 3 months or antegrade coronary flow, with Thrombolysis in Myocardial Infarction (TIMI) > 0, were excluded.
DefinitionsCTO was defined as TIMI grade 0 flow in the occluded segment, with estimated occlusion duration > 3 months.19,20 The levels of certainty of occlusion duration followed the definitions of the European Consensus Euro CTO Club:19 confirmed occlusion duration (COD) in patients with angiographic evidence of occlusion > 3 months or objective evidence of acute myocardial infarction (AMI) in the occluded coronary > 3 months before the coronary angiography; or IOD in patients with coronary occlusion with TIMI grade zero flow and anatomy suggestive of long-term occlusion (presence of collaterals or absence of contrast retention) with ischemic symptoms unaltered in the last 3 months or evidence of silent ischemia.
Collateral circulation was classified according to Rentrop et al.:21 grade 0, if there was no visible collateral filling; grade 1, if there was filling of lateral branches of the infarct-related artery, without reaching the epicardial segment; grade 2, if there was partial filling of the epicardial vessel; and grade 3, if there was complete filling of the collateral vessel promoted by the collaterals.
Angiographic success was defined as final residual stenosis < 20% with distal TIMI 3 flow. AMI was defined as an increase in creatine kinase MB isoenzyme (CK-MB) > 3 times the upper limit of normal, associated with electrocardiographic findings and/or symptoms suggestive of ischemia (periprocedural AMI) or increased CK-MB or troponin levels above the 99th percentile of a reference control population (spontaneous AMI). New target vessel revascularization (TVR) was defined as repeat PCI or bypass graft placement for restenosis at the lesion treated during index PCI due to symptoms and/or functional tests, with demonstration of ischemia in the corresponding territory. Contrast-induced nephropathy was defined as an absolute increase in serum creatinine level of 0.5mg/dL or a 25% increase compared to basal level within 48hours of the procedure.22
ProcedurePCI was performed according to standardized techniques.19,20 The procedure was indicated for patients with angina or ischemic equivalent and/or ischemia proven in functional tests, being elective in all cases. All patients received acetylsalicylic acid (loading dose of 200mg and maintenance dose of 100mg daily) and clopidogrel (loading dose of 300mg and maintenance dose of 75mg daily). Unfractionated heparin, at a dose of 100 U/kg, was used to maintain an activated clotting duration > 250seconds throughout the procedure. The use of glycoprotein IIb/IIIa inhibitors during the procedure was at the discretion of the interventionist, as well as the selection of access route and type of stent. Low-osmolality ionic contrast medium (ioxaglate) was used in all cases, and patients with clearance < 60mL/minute received isotonic (0.9%) saline for at least 6hours before and 12hours after the intervention. Acetylsalicylic acid was maintained indefinitely and clopidogrel was maintained for at least 1 month after bare-metal stents, or 12 months after acute coronary syndrome or when a drug-eluting stent was implanted.
Analyzed outcomesThe primary objective was to evaluate the success rate of the procedure, according to the estimated occlusion duration. The patients were divided into three groups for analysis: < 12 months, ≥ 12 months, or indeterminate. The analyzed secondary outcomes included in-hospital complications and combined major adverse cardiovascular events (MACE), defined as occurrence of death from all causes, AMI, or new TVR, both in-hospital and at the follow-up. Additionally, the authors analyzed MACE at the end of follow-up, according to procedural success or failure.
Coronary angiography was reviewed by two independent interventional cardiologists to determine the anatomical characteristics of lesions and vessels using QAngio® XA software, version 7.3 (Medis Medical Imaging Systems BV, Leiden, the Netherlands) for the quantitative angiography analysis.
Statistical analysisContinuous variables are shown as mean ± standard deviation or median and interquartile range, and compared using analysis of variance (ANOVA) or Kruskal-Wallis test, when they showed non-normal distribution. Categorical variables are shown as absolute numbers and percentages and compared using the chi-squared test or Fisher's exact test, as appropriate. The cumulative probability of MACE was obtained using Kaplan-Meier curves and the difference between groups was calculated by the log-rank test.
Predictors of angiographic failure were identified using binary logistic regression, including the following variables: diabetes mellitus, chronic renal failure, left ventricular dysfunction, multivessel coronary disease, tortuosity in the occlusion segment, presence of calcification, blunt stump, presence of bridge collaterals, presence of lateral branch at the site of occlusion, occlusion length ≥ 20mm, vessel diameter ≤ 2.5mm, ostial location, occluded coronary artery, and estimated occlusion duration. Variables that showed p < 0.10 in the univariate analysis were used in the multivariate model.
Two-tailed p-values < 0.05 were considered statistically significant. Analyses were performed using the R software, version 3.1 (The R Foundation for Statistical Computing, 2014, Vienna, Austria).
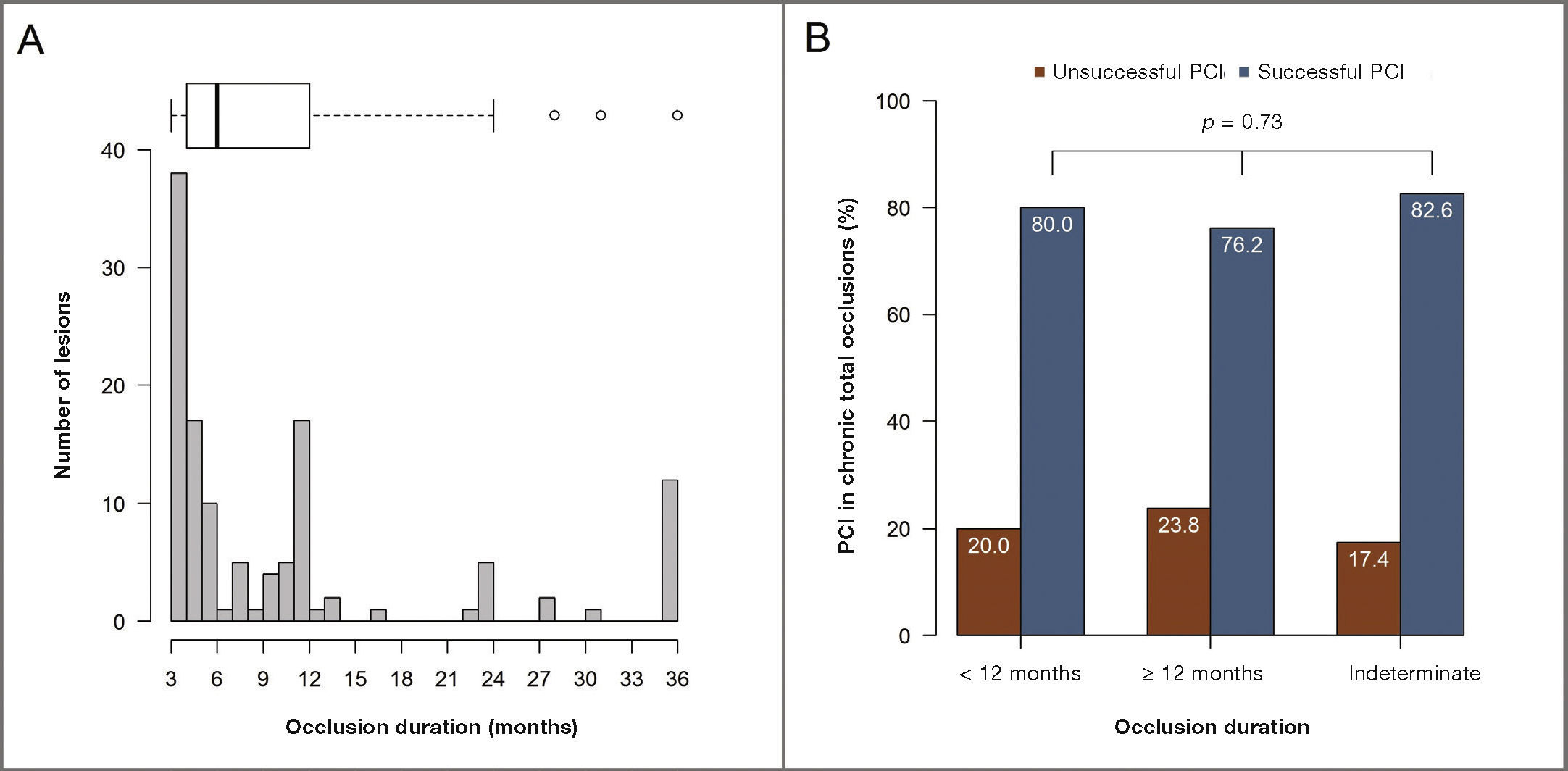
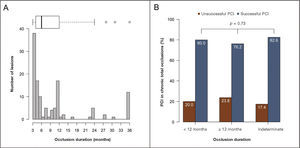
ResultsOf the 328 analyzed patients with occlusive lesions, 168 met the criteria established for COD > 3 months and were selected. A total of 122 patients (72.6%) met the definitions for COD, of whom 80 had duration < 12 months and 42 ≥ 12 months, whereas 46 (27.4%) met the definitions for IOD. The occlusion duration in the group with COD showed a median of 6.0 months (interquartile range: 4.0 to 12.0 months) and ranged from 3 to 144 months (Fig. 1A). The mean age of the population was 59.2 ± 9.5 years, with a predominance of males (70.2%), presence of diabetes mellitus in 29.8% of patients, and 18.5% had chronic renal failure.
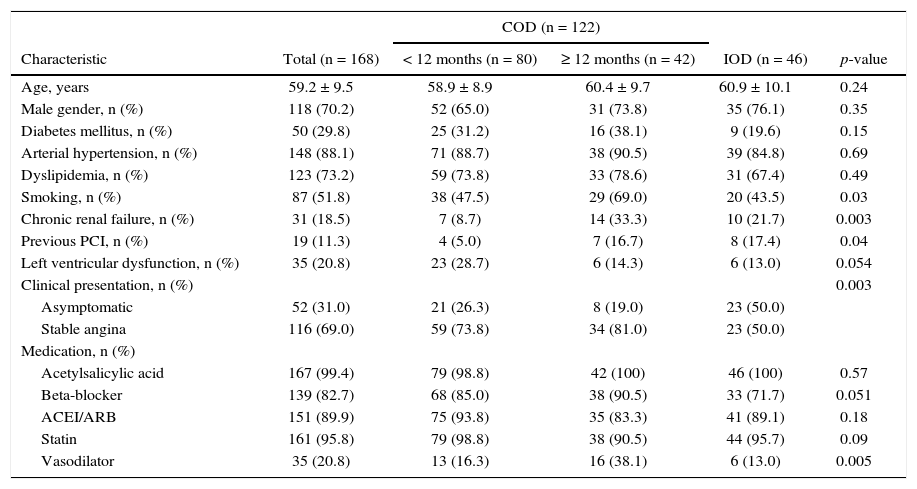
Patients with COD ≥ 12 months had a higher prevalence of smoking and chronic renal failure, whereas patients in the group with COD < 12 months had lower prevalence of previous PCI. Most patients were receiving drug therapy for stable coronary disease, with a higher rate of vasodilators in the group with COD ≥ 12 months (Table 1).
Clinical and demographic characteristics.
| COD (n = 122) | |||||
|---|---|---|---|---|---|
| Characteristic | Total (n = 168) | < 12 months (n = 80) | ≥ 12 months (n = 42) | IOD (n = 46) | p-value |
| Age, years | 59.2 ± 9.5 | 58.9 ± 8.9 | 60.4 ± 9.7 | 60.9 ± 10.1 | 0.24 |
| Male gender, n (%) | 118 (70.2) | 52 (65.0) | 31 (73.8) | 35 (76.1) | 0.35 |
| Diabetes mellitus, n (%) | 50 (29.8) | 25 (31.2) | 16 (38.1) | 9 (19.6) | 0.15 |
| Arterial hypertension, n (%) | 148 (88.1) | 71 (88.7) | 38 (90.5) | 39 (84.8) | 0.69 |
| Dyslipidemia, n (%) | 123 (73.2) | 59 (73.8) | 33 (78.6) | 31 (67.4) | 0.49 |
| Smoking, n (%) | 87 (51.8) | 38 (47.5) | 29 (69.0) | 20 (43.5) | 0.03 |
| Chronic renal failure, n (%) | 31 (18.5) | 7 (8.7) | 14 (33.3) | 10 (21.7) | 0.003 |
| Previous PCI, n (%) | 19 (11.3) | 4 (5.0) | 7 (16.7) | 8 (17.4) | 0.04 |
| Left ventricular dysfunction, n (%) | 35 (20.8) | 23 (28.7) | 6 (14.3) | 6 (13.0) | 0.054 |
| Clinical presentation, n (%) | 0.003 | ||||
| Asymptomatic | 52 (31.0) | 21 (26.3) | 8 (19.0) | 23 (50.0) | |
| Stable angina | 116 (69.0) | 59 (73.8) | 34 (81.0) | 23 (50.0) | |
| Medication, n (%) | |||||
| Acetylsalicylic acid | 167 (99.4) | 79 (98.8) | 42 (100) | 46 (100) | 0.57 |
| Beta-blocker | 139 (82.7) | 68 (85.0) | 38 (90.5) | 33 (71.7) | 0.051 |
| ACEI/ARB | 151 (89.9) | 75 (93.8) | 35 (83.3) | 41 (89.1) | 0.18 |
| Statin | 161 (95.8) | 79 (98.8) | 38 (90.5) | 44 (95.7) | 0.09 |
| Vasodilator | 35 (20.8) | 13 (16.3) | 16 (38.1) | 6 (13.0) | 0.005 |
COD: confirmed occlusion duration; IOD: indeterminate occlusion duration; PCI: percutaneous coronary intervention; ACEI: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker.
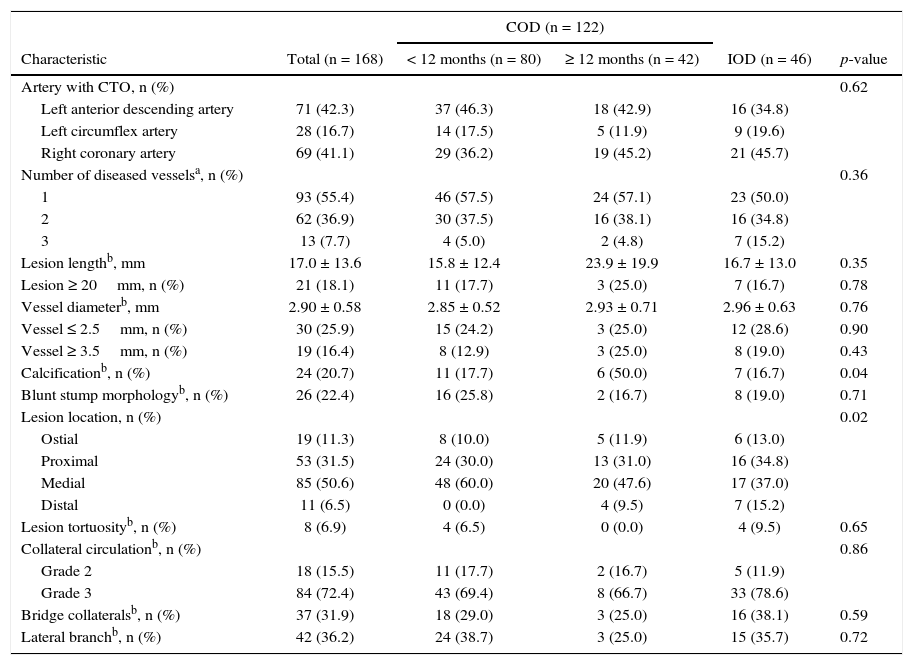
The most commonly treated artery was the left anterior descending artery (42.3%), followed by the right coronary artery (41.1%) and the left circumflex artery (Table 2). No significant difference was observed between groups regarding patients’ angiographic characteristics, except in the distribution of lesion location (p = 0.02), although there was no difference regarding the ostial location of lesions. Multivessel coronary artery disease was present in 44.6% of patients. The lesions had an occlusive segment on average 17.0 ± 13.6mm long in vessels of 2.90 ± 0.58mm in diameter. Collateral circulation grade 2 or 3 was present in approximately 90% of patients.
Angiographic characteristics.
| COD (n = 122) | |||||
|---|---|---|---|---|---|
| Characteristic | Total (n = 168) | < 12 months (n = 80) | ≥ 12 months (n = 42) | IOD (n = 46) | p-value |
| Artery with CTO, n (%) | 0.62 | ||||
| Left anterior descending artery | 71 (42.3) | 37 (46.3) | 18 (42.9) | 16 (34.8) | |
| Left circumflex artery | 28 (16.7) | 14 (17.5) | 5 (11.9) | 9 (19.6) | |
| Right coronary artery | 69 (41.1) | 29 (36.2) | 19 (45.2) | 21 (45.7) | |
| Number of diseased vesselsa, n (%) | 0.36 | ||||
| 1 | 93 (55.4) | 46 (57.5) | 24 (57.1) | 23 (50.0) | |
| 2 | 62 (36.9) | 30 (37.5) | 16 (38.1) | 16 (34.8) | |
| 3 | 13 (7.7) | 4 (5.0) | 2 (4.8) | 7 (15.2) | |
| Lesion lengthb, mm | 17.0 ± 13.6 | 15.8 ± 12.4 | 23.9 ± 19.9 | 16.7 ± 13.0 | 0.35 |
| Lesion ≥ 20mm, n (%) | 21 (18.1) | 11 (17.7) | 3 (25.0) | 7 (16.7) | 0.78 |
| Vessel diameterb, mm | 2.90 ± 0.58 | 2.85 ± 0.52 | 2.93 ± 0.71 | 2.96 ± 0.63 | 0.76 |
| Vessel ≤ 2.5mm, n (%) | 30 (25.9) | 15 (24.2) | 3 (25.0) | 12 (28.6) | 0.90 |
| Vessel ≥ 3.5mm, n (%) | 19 (16.4) | 8 (12.9) | 3 (25.0) | 8 (19.0) | 0.43 |
| Calcificationb, n (%) | 24 (20.7) | 11 (17.7) | 6 (50.0) | 7 (16.7) | 0.04 |
| Blunt stump morphologyb, n (%) | 26 (22.4) | 16 (25.8) | 2 (16.7) | 8 (19.0) | 0.71 |
| Lesion location, n (%) | 0.02 | ||||
| Ostial | 19 (11.3) | 8 (10.0) | 5 (11.9) | 6 (13.0) | |
| Proximal | 53 (31.5) | 24 (30.0) | 13 (31.0) | 16 (34.8) | |
| Medial | 85 (50.6) | 48 (60.0) | 20 (47.6) | 17 (37.0) | |
| Distal | 11 (6.5) | 0 (0.0) | 4 (9.5) | 7 (15.2) | |
| Lesion tortuosityb, n (%) | 8 (6.9) | 4 (6.5) | 0 (0.0) | 4 (9.5) | 0.65 |
| Collateral circulationb, n (%) | 0.86 | ||||
| Grade 2 | 18 (15.5) | 11 (17.7) | 2 (16.7) | 5 (11.9) | |
| Grade 3 | 84 (72.4) | 43 (69.4) | 8 (66.7) | 33 (78.6) | |
| Bridge collateralsb, n (%) | 37 (31.9) | 18 (29.0) | 3 (25.0) | 16 (38.1) | 0.59 |
| Lateral branchb, n (%) | 42 (36.2) | 24 (38.7) | 3 (25.0) | 15 (35.7) | 0.72 |
COD: confirmed occlusion duration; IOD: indeterminate occlusion duration; CTO: chronic total occlusion.
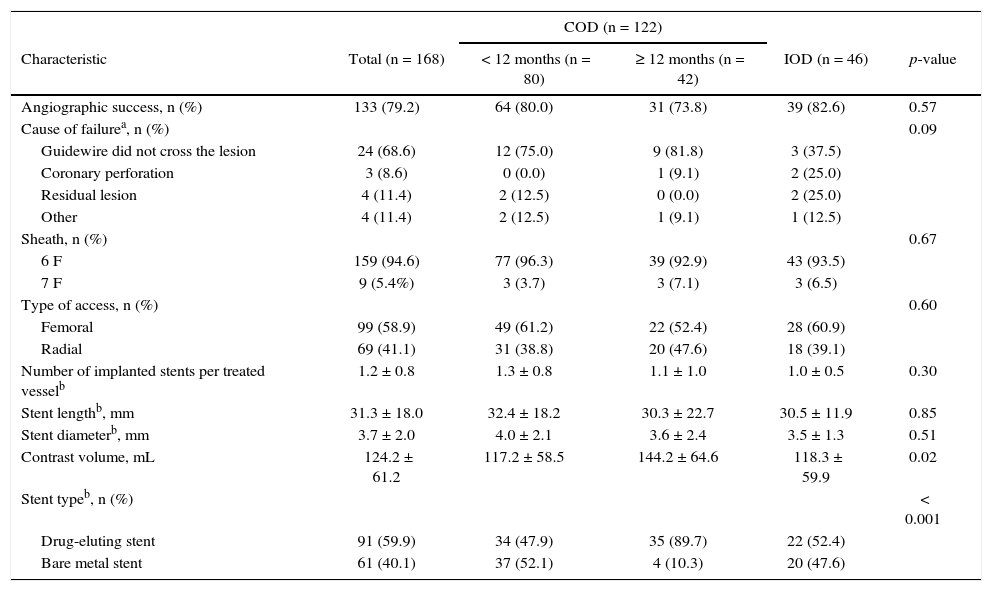
As for the procedural data (Table 3), the 6 F sheath was used in 94.6% of cases and the femoral access, in 58.9%. The antegrade approach was used in most cases (98.8%). A total of 152 stents was implanted in 133 patients, with a mean of 1.2 ± 0.8 stents implanted per lesion, with no significant difference between the groups. The most often used stent was the drug-eluting stent, especially in the groups with COD ≥ 12 months (89.7%; p < 0.001). During the procedure, 124.2 ± 61.2mL of contrast were used, with use of larger volumes in the group with COD ≥ 12 months, when compared with the group with COD < 12 months and IOD (117.2mL vs. 144.2mL vs. 118.3mL; p = 0.02). The main cause of procedural failure was the inability to cross the lesion with the guidewire (68.6%).
Characteristics of procedure.
| COD (n = 122) | |||||
|---|---|---|---|---|---|
| Characteristic | Total (n = 168) | < 12 months (n = 80) | ≥ 12 months (n = 42) | IOD (n = 46) | p-value |
| Angiographic success, n (%) | 133 (79.2) | 64 (80.0) | 31 (73.8) | 39 (82.6) | 0.57 |
| Cause of failurea, n (%) | 0.09 | ||||
| Guidewire did not cross the lesion | 24 (68.6) | 12 (75.0) | 9 (81.8) | 3 (37.5) | |
| Coronary perforation | 3 (8.6) | 0 (0.0) | 1 (9.1) | 2 (25.0) | |
| Residual lesion | 4 (11.4) | 2 (12.5) | 0 (0.0) | 2 (25.0) | |
| Other | 4 (11.4) | 2 (12.5) | 1 (9.1) | 1 (12.5) | |
| Sheath, n (%) | 0.67 | ||||
| 6 F | 159 (94.6) | 77 (96.3) | 39 (92.9) | 43 (93.5) | |
| 7 F | 9 (5.4%) | 3 (3.7) | 3 (7.1) | 3 (6.5) | |
| Type of access, n (%) | 0.60 | ||||
| Femoral | 99 (58.9) | 49 (61.2) | 22 (52.4) | 28 (60.9) | |
| Radial | 69 (41.1) | 31 (38.8) | 20 (47.6) | 18 (39.1) | |
| Number of implanted stents per treated vesselb | 1.2 ± 0.8 | 1.3 ± 0.8 | 1.1 ± 1.0 | 1.0 ± 0.5 | 0.30 |
| Stent lengthb, mm | 31.3 ± 18.0 | 32.4 ± 18.2 | 30.3 ± 22.7 | 30.5 ± 11.9 | 0.85 |
| Stent diameterb, mm | 3.7 ± 2.0 | 4.0 ± 2.1 | 3.6 ± 2.4 | 3.5 ± 1.3 | 0.51 |
| Contrast volume, mL | 124.2 ± 61.2 | 117.2 ± 58.5 | 144.2 ± 64.6 | 118.3 ± 59.9 | 0.02 |
| Stent typeb, n (%) | < 0.001 | ||||
| Drug-eluting stent | 91 (59.9) | 34 (47.9) | 35 (89.7) | 22 (52.4) | |
| Bare metal stent | 61 (40.1) | 37 (52.1) | 4 (10.3) | 20 (47.6) | |
COD: confirmed occlusion duration; IOD: indeterminate occlusion duration.
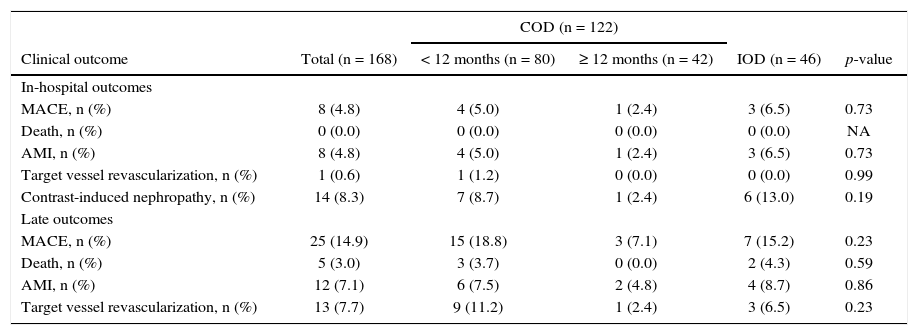
Angiographic success was achieved in 79.2% of cases, with no significant difference between groups (80.0% vs. 73.8% vs. 82.6%; p = 0.73; Fig. 1B). Regarding in-hospital complications, there was no significant difference between the groups regarding MACE (4.8% vs. 7.1% vs. 6.0%; p = 0.73), which was explained almost entirely by periprocedural AMI. There were no deaths and only one TVR was observed due to a stent thrombosis that occurred hours after the procedure. There were three coronary perforations, none of which required pericardiocentesis. Contrast-induced nephropathy rates (8.7% vs. 2.4% vs. 13.0%; p = 0.19) did not differ between the groups.
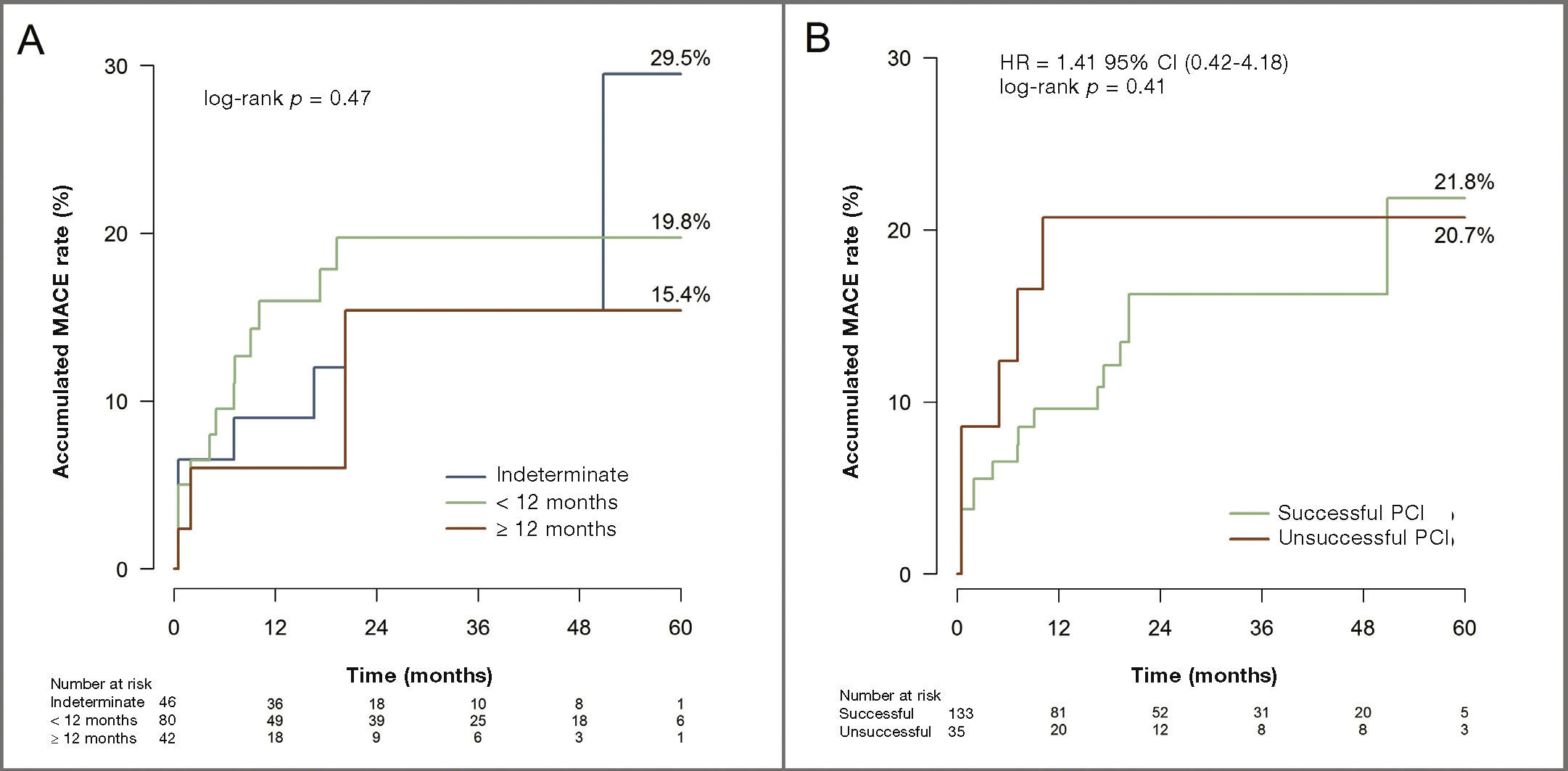
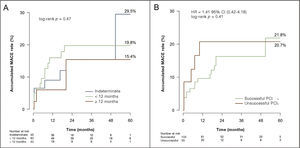
The median clinical follow-up was 21.3 months (interquartile range: 5.9 to 36.5 months). There was no significant difference between groups at the end of follow-up regarding rates of MACE (18.8% vs. 7.1% vs. 15.3%; p = 0.23), death (3.7% vs. 0% vs. 4.3%; p = 0.59), AMI (7.5% vs. 4.8% vs. 8.7%; p = 0.86), or new TVR (11.2% vs. 2.4% vs. 6.5%; p = 0.23; Table 4 and Fig. 2A). Similarly, there was no significant difference in the cumulative rate of MACE at the end of follow-up between patients who had a successful PCI and those who did not (21.8% vs. 20.7%; hazard ratio - HD = 1.41; 95% confidence interval - 95% CI 0.42-4.18, log-rank p = 0.41; Fig. 2B).
In-hospital and late clinical outcomes.
| COD (n = 122) | |||||
|---|---|---|---|---|---|
| Clinical outcome | Total (n = 168) | < 12 months (n = 80) | ≥ 12 months (n = 42) | IOD (n = 46) | p-value |
| In-hospital outcomes | |||||
| MACE, n (%) | 8 (4.8) | 4 (5.0) | 1 (2.4) | 3 (6.5) | 0.73 |
| Death, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | NA |
| AMI, n (%) | 8 (4.8) | 4 (5.0) | 1 (2.4) | 3 (6.5) | 0.73 |
| Target vessel revascularization, n (%) | 1 (0.6) | 1 (1.2) | 0 (0.0) | 0 (0.0) | 0.99 |
| Contrast-induced nephropathy, n (%) | 14 (8.3) | 7 (8.7) | 1 (2.4) | 6 (13.0) | 0.19 |
| Late outcomes | |||||
| MACE, n (%) | 25 (14.9) | 15 (18.8) | 3 (7.1) | 7 (15.2) | 0.23 |
| Death, n (%) | 5 (3.0) | 3 (3.7) | 0 (0.0) | 2 (4.3) | 0.59 |
| AMI, n (%) | 12 (7.1) | 6 (7.5) | 2 (4.8) | 4 (8.7) | 0.86 |
| Target vessel revascularization, n (%) | 13 (7.7) | 9 (11.2) | 1 (2.4) | 3 (6.5) | 0.23 |
COD: confirmed occlusion duration; IOD: indeterminate occlusion duration; MACE: major adverse cardiovascular events; NA: not applicable; AMI: acute myocardial infarction.
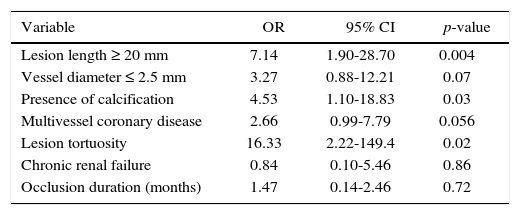
Predictors associated with angiographic failure in the univariate model were lesion length ≥ 20mm, reference vessel diameter ≤ 2.5mm, calcified lesion, multivessel coronary disease, presence of tortuosity in the occluded segment, and chronic renal failure. Of these, lesion length ≥ 20mm (OR = 7.27; 95% CI 1.94-29.1; p = 0.003), presence of calcification (OR = 4.72; 95% CI 1.19-19.1; p = 0.02), and tortuosity in the occluded segment (OR = 15.98; 95% CI 2.18-144.7; p = 0.007) were independent predictors of angiographic failure in the multivariate model (Table 5).
Independent predictors of angiographic failure.
| Variable | OR | 95% CI | p-value |
|---|---|---|---|
| Lesion length ≥ 20 mm | 7.14 | 1.90-28.70 | 0.004 |
| Vessel diameter ≤ 2.5 mm | 3.27 | 0.88-12.21 | 0.07 |
| Presence of calcification | 4.53 | 1.10-18.83 | 0.03 |
| Multivessel coronary disease | 2.66 | 0.99-7.79 | 0.056 |
| Lesion tortuosity | 16.33 | 2.22-149.4 | 0.02 |
| Chronic renal failure | 0.84 | 0.10-5.46 | 0.86 |
| Occlusion duration (months) | 1.47 | 0.14-2.46 | 0.72 |
Hosmer-Lemeshow statistics = 0.14.
OR: odds ratio; 95% CI: 95% confidence interval.
The present study has several important findings. First, a success rate of 79.2% in PCI was identified in a selection of contemporary patients with coronary lesions with CTO using the antegrade approach, which is comparable to those found in other recent large studies.23–26 Additionally, this study showed that PCI in CTO is a safe procedure with a low rate of in-hospital complications, no deaths, and no need for emergency coronary artery bypass surgery or cardiac tamponade requiring pericardial drainage during in-hospital stay, a finding similar to that of previous studies.17,27,28
The main finding of this study was that neither a long occlusion duration nor IOD affected the success rate or the long-term prognosis of patients undergoing PCI in CTO. The analysis of initial studies showed an association between long occlusion duration and angiographic failure of the procedure.15,16 More recently, Olivari et al. showed that occlusion duration superior to 6 months was associated with percutaneous intervention failure in an analysis of 376 consecutive patients with CTO, although, in that study, not all patients had occlusion duration superior to 3 months.29 Similarly, Barlis at al. demonstrated that an IOD determines a five-fold increase in the risk of angiographic failure in an analysis of 202 patients undergoing PCI in CTO.17 Currently, with the increased experience of interventionists and the development and improvement of new devices, the occlusion duration has shown less impact on the success rate of PCI in CTO. In fact, Tomasello at al. showed no association between estimated occlusion duration, or even IOD, and procedural success rate in the analysis of 303 patients with CTO,18 in agreement with the results of the present study, which showed that the occlusion duration should not be considered as determining factor for decision-making regarding intervention in CTO.
The prognostic effect of PCI in CTO remains controversial and to date there is no published randomized study to elucidate this question. Many nonrandomized studies have shown favorable results in the short and long-term prognosis for patients successfully submitted to PCI in CTO, when compared to those whose procedure was unsuccessful.14,17,23,24,29 Similarly, recent meta-analyses have shown that successful PCI in CTO is associated with lower rates of mortality, need for revascularization, and residual or recurrent angina, with no difference in the AMI rate when compared to patients with procedural failure.12,30,31 However, the present study showed no difference in the late follow-up regarding the rate of combined events of death from any cause, AMI, or new TVR between patients who had successful PCI, when compared to those with procedural failure. Possible explanations for this divergent finding of literature are the observational and retrospective design of most previous studies, as well as of the present study, which may have introduced a selection bias, creating heterogeneous groups that may have generated differences in prognosis after the intervention; the size of this study's population may not have been enough to detect a significant difference in the clinical event rate, even with a long-term follow-up; and finally, the use of different definitions of clinical outcomes between studies.
Several angiographic variables were identified in previous studies as independent predictors of procedural failure, such as lesion with long occlusion segment, presence of calcification, tortuosity in the lesion segment, lateral branch at the occlusion site, blunt stump, small reference vessel diameter, multivessel disease, and ostial location of the occlusion.17,18,23,32,33 The present study confirmed some of these variables (long occlusion segment, tortuosity in the lesion segment and presence of calcification). However, making comparisons of predictors among various studies may be difficult, because most studies have a small number of patients and consequently little statistical power to identify independent predictors. Moreover, the duration definition for CTO shows significant difference between studies, ranging from 2 weeks to 3 months as a criterion to define CTO. Furthermore, many studies showed incomplete angiographic data, with different definitions for lesion characteristics and inclusion of patients with TIMI grade 1 flow in the analyses.
LimitationsThe present study has some limitations, as follows: first, its nonrandomized and retrospective study design may have introduced a selection bias; second, the results reflected the experience of a single center, with intermediate-volume CTO operators; third, the low rate of the retrograde technique use, which is associated with higher success rates, may also have affected the results; and finally, due to the small sample size, this study did not have enough statistical power to draw conclusions on the rate of clinical events between the assessed groups and thus, the findings are considered only as hypothesis generator.
ConclusionsOcclusion duration was associated with neither increased failure rate of the procedure nor worse late outcomes in patients submitted to percutaneous coronary intervention in chronically occluded coronary arteries. Therefore, occlusion duration should not limit the therapeutic approach in patients with chronic total occlusions.
Funding sourceNone declared.
Conflicts of interestThe authors declare no conflicts of interest.
Peer review under the responsibility of Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista.