Coronary artery disease is a major cause of death in patients with chronic kidney disease. Moreover, due to the high prevalence of risk factors for atherosclerosis, many of these patients require percutaneous coronary intervention (PCI) even after renal transplantation. The aim of this study is to report the late follow-up of patients with renal transplantation treated with PCI and stenting.
MethodsPatients>18 years of age, with prior kidney transplantation, and treated with PCI were included. Clinical follow-up was evaluated by medical record analysis and telephone contact. The study endpoint was the incidence of major adverse cardiac events (MACE) during follow-up.
ResultsTwenty-nine patients were included. Mean age was 54.8±8 years and the majority male (72.4%). The prevalence of hypertension was 89.7%, dyslipidemia 69% and diabetes 51.7%. Most of them had multivessel disease (2-vessel: 44.8%; 3-vessel: 41.4%). Lesion complexity was high, being 84.3% type B2 or C lesions and 27.5% bifurcation lesions. Procedural success rate was 100%. Bare metal stents were used in 96.6% of cases. The follow-up time was 1,378±977 days. The mortality rate was 25.1%, target vessel revascularization rate was 15.9% and none of the patients presented nonfatal infarction. The incidence of MACE during follow-up was 34.5%.
ConclusionsLate follow-up after PCI in renal transplantation patients demonstrated a high probability of clinical events. However, the study population was a sample of high clinical and angiographic complexity.
Evolução Clínica após Intervenção CoronáriaPercutânea em Indivíduos com Transplante Renal Prévio
IntroduçâoA doença arterial coronária é uma das principaiscausas de óbito em pacientes com doença renal crônica Alémdisso, em decorrência da elevada prevalência de fatores de risco para aterosclerose, muitos desses pacientes necessitam de intervenção coronária percutânea (ICP) mesmo após o transplante renal. O objetivo deste estudo é descrever a evolução tardia de pacientes transplantados renais submetidos à ICP com stent.
MétodosForam incluídos pacientes transplantados renais, com idade>18 anos, tratados com ICP. O seguimento foi realizado por análise de prontuários e contato telefônico. O desfecho do estudo foi a incidência de eventos cardíacos adversos maiores (ECAM) durante o seguimento.
ResultadosForam incluídos 29 pacientes. A média de idade foi de 54,8±8 anos, sendo a maioria do sexo masculino (72,4%). A prevalênciade hipertensâo arterial sistèmica foi de 89,7%, de dislipidemia de 69%; e de diabetes, de 51,7%. A maior parte apresentava doença multiarterial (biarterial, 44,8%; triarterial, 41,4%). A complexidade das lesôes foi elevada, sendo 84,3% dos tipos B2 ou C e 2 7,5% com lesôes em bifurcaçâo. A taxa de sucesso do procedimento foi de 100%. Stents convencionais foram utilizados em 96,6% dos casos. O tempo de seguimento foi de 1.378±977 dias. A mortalidade foi de 25,1%, a taxa de revascularizaçâo do vaso-alvo foi de 15,9% e nenhum paciente apresentou infarto nâo fatal. A incidênciade ECAM durante a evoluçâo foi de 34,5%.
ConclusõesA evoluçâo clínica tardia após ICP em pacientes transplantados renais demonstrou elevada probabilidade de eventos clínicos. No entanto, a populaçâo estudada foi uma amostra de altacomplexidade clínica e angiográfica.
The increasing prevalence of chronic kidney disease and consequent increased demand for renal replacement therapy has induced increased rates of renal transplantation worldwide.1 Only in Brazil, in the first half of 2012, 2,689 kidney transplantations were performed.2 In this context, there is an increased concern regarding this specific part of the population, aiming to identify their clinical peculiarities and to understand the comorbidities that develop over time.3
In recent years, chronic kidney disease has been confirmed as a condition very frequently associated with coronary artery disease, which is one of leading causes of death in patients who require substitutive therapy.4 In a recent study of patients who underwent renal transplantation, after a period of 2.9years, 32.8% had altered non invasive tests for assessment of myocardial ischaemia and 14.5% had angiographically significant lesions in the coronary angiography.5
In this scenario, percutaneous coronary intervention (PCI) has been increasingly used in renal transplantation patients, especially because it is a less invasive procedure when compared with the surgical alternative, following its specific indications. Moreover, in general, mortality between percutaneous and surgical revascularization alternatives is very similar in this population.6
Few studies have analyzed the long-term evolution of patients with prior renal transplantation treated with PCI and stenting. Research on this subject is of considerable interest, since it not only allows for the evaluation of the influence of classical risk factors for the development of coronary artery disease, but also for speculation on the impact of the characteristics of renal transplantation recipients, including the use of already tested immunosuppressive drugs to reduce intrastent restenosis.7−9
This study aimed to describe the late evolution in patients with a history of renal transplantation submitted to PCI with stenting.
METHODSThis was a retrospective, single-center study, conducted at a tertiary care, high-complexity cardiology service. The research was based on the analysis of the database, medical records review, and telephone contact.
Study populationBetween March 2002 and June 201 1, 36 patients with prior renal transplantation were treated with PCI at the Instituto do Coragao do Hospital das Clínicas, School of Medicine, Universidade of Sao Paulo (Incor/ HCFMUSP, Sao Paulo, SP, Brazil). Seven patients were excluded, as they did not have any new consultations recorded in their medical charts and it was not possible to complete the follow-up by telephone. A total of 29 subjects comprised the final population of the analysis.
ProcedureUnfractionated heparin at a dose from70 U/kg to 100 U/kg was previously administered in all the procedures, aimed at obtaining activated clotting time between 250–300 seconds; the patients were receiving dual antiplatelet therapy with acetylsalicylic acid 100mg and clopidogrel 75mg.
The choice of access route, techniques, and materials, as well as diagnostic and intervention methods was made at the surgeon's discretion. All cases received at least one bare-metal stent (BMS) or drug-eluting stent (DES) with diameters varying between 2.5mm and 4mm. Angiographic success was considered with residual stenosis<30% after PCI.
Data collectionClinical and angiographic characteristics were obtained from the database of the Service of Hemodynamics and Interventional Cardiology of InCor/HCFMUSP. Information on the use of immunosuppressants was also assessed in each case.
The investigation of the events was performed using information obtained through medical record review and telephone contact. For cases in which the same event occurred more than once for the same patient, the repeated event was disregarded in the temporal analysis.
The study outcome was the occurrence of major adverse cardiac events (MACE) during follow-up, defined as death from any cause, acute myocardial infarction, and target vessel reintervention.
Statistical analysisAnalysis of the clinical and angiographic data was performed using the SPSS software (IBM Corp. - New York, United States). Continuous variables were described as mean and standard deviation, while categorical variables were described as frequencies and percentages. The event rate was estimated by Kaplan-Meier method.
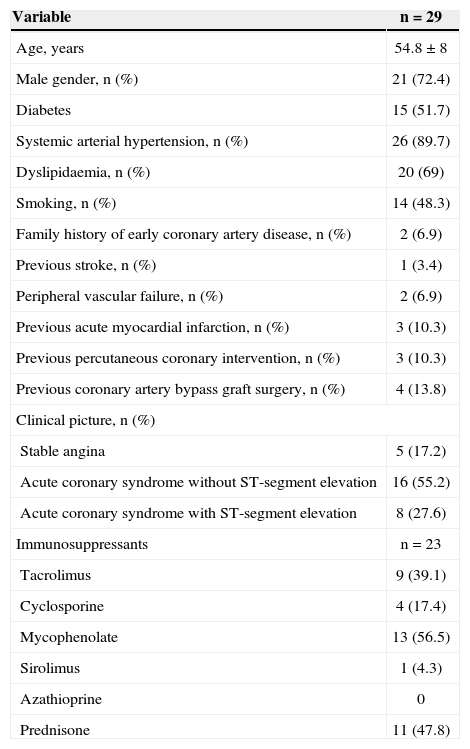
RESULTSThe mean age was 54.8±8 years and most of the subjects were males (72.4%). The prevalence of hypertension was 89.7%; dyslipidemia, 69%; diabetes, 51.7%; and previous or current history of smoking, 48.3%. The clinical picture that motivated the PCI was, in most cases, acute coronary syndrome without ST-segment elevation, observed in 55.2% of cases, followed by acute coronary syndrome with ST-segment elevation in 27.6%. All others were diagnosed with stable angina (Table 1).
Clinical characteristics
| Variable | n=29 |
|---|---|
| Age, years | 54.8±8 |
| Male gender, n (%) | 21 (72.4) |
| Diabetes | 15 (51.7) |
| Systemic arterial hypertension, n (%) | 26 (89.7) |
| Dyslipidaemia, n (%) | 20 (69) |
| Smoking, n (%) | 14 (48.3) |
| Family history of early coronary artery disease, n (%) | 2 (6.9) |
| Previous stroke, n (%) | 1 (3.4) |
| Peripheral vascular failure, n (%) | 2 (6.9) |
| Previous acute myocardial infarction, n (%) | 3 (10.3) |
| Previous percutaneous coronary intervention, n (%) | 3 (10.3) |
| Previous coronary artery bypass graft surgery, n (%) | 4 (13.8) |
| Clinical picture, n (%) | |
| Stable angina | 5 (17.2) |
| Acute coronary syndrome without ST-segment elevation | 16 (55.2) |
| Acute coronary syndrome with ST-segment elevation | 8 (27.6) |
| Immunosuppressants | n=23 |
| Tacrolimus | 9 (39.1) |
| Cyclosporine | 4 (17.4) |
| Mycophenolate | 13 (56.5) |
| Sirolimus | 1 (4.3) |
| Azathioprine | 0 |
| Prednisone | 11 (47.8) |
On average, patients had 6±6years since the transplantation. The prescription of immunosuppressants was available for 23 patients, and the drugs most often prescribed were mycophenolate (56.5%), prednisone (47.8%), and tacrolimus (39.1%) (Table 1).
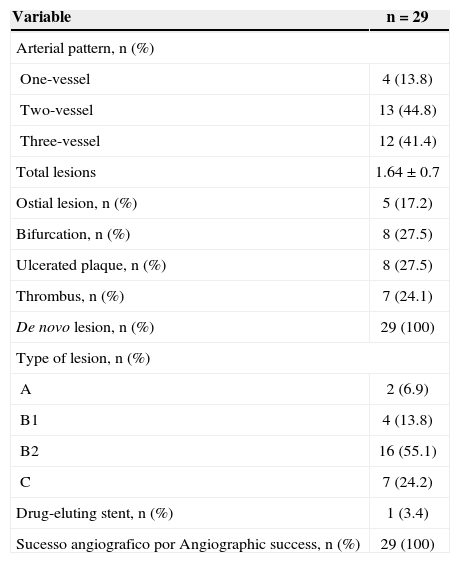
Most cases had a multivessel obstructive pattern (two-vessel, 44.8%; three-vessel, 41.4%). Lesion complexity was high; 79.3% were type B2 or C lesions, and 27.5% involved bifurcations lesions,24.1% lesions with thrombus, and 17.2% ostial lesions. De novo lesions were treated in all cases. BMS were used in 96.6%of the cases, and angiographic success was attained in 100% of cases (Table 2).
Angiographic characteristics
| Variable | n=29 |
|---|---|
| Arterial pattern, n (%) | |
| One-vessel | 4 (13.8) |
| Two-vessel | 13 (44.8) |
| Three-vessel | 12 (41.4) |
| Total lesions | 1.64±0.7 |
| Ostial lesion, n (%) | 5 (17.2) |
| Bifurcation, n (%) | 8 (27.5) |
| Ulcerated plaque, n (%) | 8 (27.5) |
| Thrombus, n (%) | 7 (24.1) |
| De novo lesion, n (%) | 29 (100) |
| Type of lesion, n (%) | |
| A | 2 (6.9) |
| B1 | 4 (13.8) |
| B2 | 16 (55.1) |
| C | 7 (24.2) |
| Drug-eluting stent, n (%) | 1 (3.4) |
| Sucesso angiografico por Angiographic success, n (%) | 29 (100) |
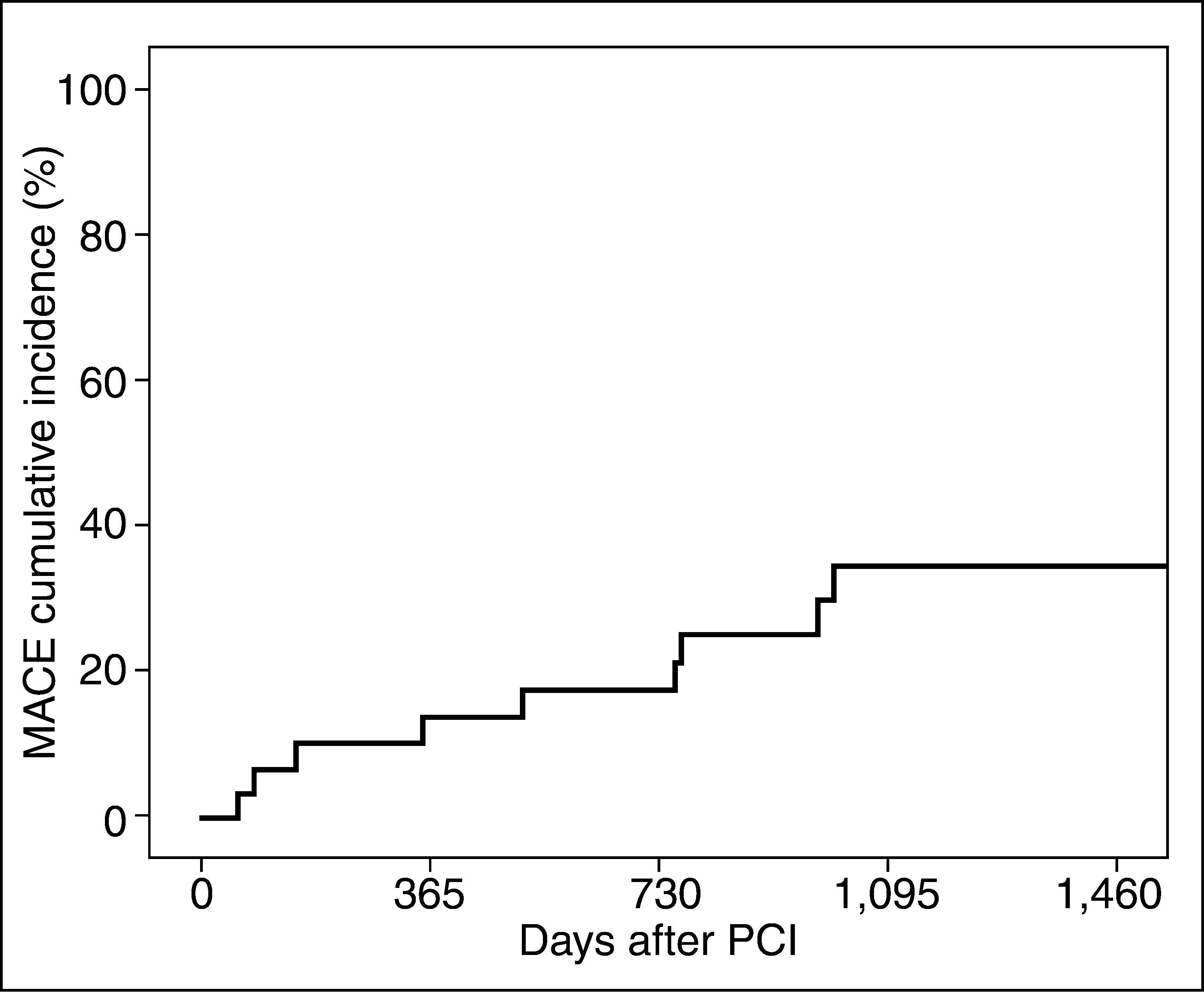
The meantime of follow-up after PCI was 1,378±977 days. During this period, 34.5% of patients had at least one MACE. The incidence of adverse events occurred throughout the study period (Fig. 1). Mortality during follow-up was 25.1%. None of the patients had nonfatal acute myocardial infarction in the period, and 15.9% required target vessel reintervention.
DISCUSSIONAccording to previous studies, the incidence of coronary atherosclerosis substantially higher in renal transplantation patients than in the general population.10 Moreover, the risk for development of coronary artery disease is high, even before the progression to end-stage renal disease.11
This study evaluated the long-term evolution of patients treated with PCI and stenting in this specific population of transplanted patients. The authors consider the research relevant, as it allows for a better evaluation of the results of percutaneous treatment in patients with such particular characteristics, through the analysis of a significant sample of patients with these characteristics.
The occurrence of MACE in approximately one-third of patients over a period of more than three years indicates that, even with partial renal function or fully recovered, the sample reflects a population at high risk for developing severe events.12
Considering that only one study patient was treated with DES, where as all the others were treated with BMS (96.6%), the need for target vessel reintervention in 15.9% of cases was an interesting result. In the general population, intrastent restenosis (which results from excessive neointimal proliferation after BMS implantation)occurs in 20% to 30% of cases, determining higher rates of target vessel reintervention than those observed in the present study.13−15 This result may be associated with a potential benefit of the immunosuppressive therapy, reaffirming what has been suggested in previous studies7−16
During the follow-up period,in one-quarter of the patients, mortality from all causes was the major component of the high occurrence of MACE. This high death rate is expected in this population group, since, in addition to the high underlying cardiovascular risk, the impaired immune capacity (caused by the chronic kidney disease itself and the use of immunosuppressants) is associated with a higher risk of developing severe comorbidities, such as infections and malignancies, which are potentially life-threatening.3,17
Study limitationsThe study has some limitations, including the fact that it was retrospective, based on information obtained from a database and medical records, as well as telephone contact, which was not possible in all cases. There was, therefore, loss of a non-negligible portion of patients who could not be included the final analysis. Moreover, the inclusion of patients who had their procedures performed at very different times, especially in an area of cardiology in which there are constant advances in the methods, materials, and medications, caused some individuals to receive slightly differentiated treatment.
CONCLUSIONSIn the present study, late clinical outcome after PCI in renal transplantation patients showed a high likelihood of clinical events. However, the population studied was a sample of high clinical and angiographic complexity. The rate of target vessel revascularization was reduced, but this finding needs to be better evaluated in studies with larger sample sizes.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.