Chronic kidney disease (CKD) is a prevalent dysfunction and renal transplant is the alternative for improving the lives of these patients. We seek to identify the factors that contribute to the loss of renal transplant in order to improve the management protocol in our population.
MethodologyRetrospective cohort study in patients with renal transplantation (deceased donor) at Hospital Universitario de Neiva, Colombia, with a year of follow-up period. Data were processed in STATA 11.1, using univariate analysis, odds ratio (OR), (95% CI) and Fisher test, with p<0.05 significance.
ResultsIn 160 patients, 49.38% with arterial hypertension (HTN) and diabetes mellitus (DM) as the cause for CKD, there was 20% failure incidence. Probable causes of transplant loss: age over 60 (OR: 2.3); time of cold ischemia greater than 13h (OR: 2); donor age greater than 50 (OR: 2.8). One-month complications: urologic (OR: 3.3), vascular (OR: 4), acute rejection (OR: 3.3). Six-month complications: vascular (OR: 4.5), urologic (OR: 3.3), infectious (OR: 2.8). One-year complications: acute rejection (OR: 11.3), chronic graft nephropathy (OR: 15.3), infection (OR: 9.4).
ConclusionsArterial hypertension and DM are the main etiologies of CKD. The causes of renal transplant failure were mainly vascular and infectious. Probable risk factors of statistical and clinical importance were suggested but a larger sample size is required for more robust statistical evidence.
La enfermedad renal crónica (ERC) es una patología prevalente, y el trasplante renal es la alternativa para mejorar la calidad de vida de estos pacientes. Buscamos identificar las causas que contribuyen a la pérdida del trasplante renal a fin de mejorar el protocolo de manejo en nuestra población.
MetodologíaEstudio de cohorte retrospectivo en pacientes con transplante renal (donante cadavérico) del Hospital Universitario de Neiva, Colombia, seguimiento a un año. Los datos se procesaron en STATA 11.1, se aplicó un análisis univariado, odds ratio (OR), IC 95% y la prueba de Fisher con significación p < 0,05.
ResultadosUn total de 160 pacientes, el 49,38% con hipertensión arterial (HTA) y diabetes mellitus (DM) como causa de ERC. Incidencia de fracaso del 20%. Probables causas de pérdida del trasplante: edad mayor de 60 años (OR: 2,3), tiempo de isquemia fría mayor de 13 h (OR: 2), edad del donante mayor a 50 años (OR: 2,8). Complicaciones al primer mes: urológicas (OR: 3,3), vasculares (OR: 4), rechazo agudo (OR: 3,3). Al sexto mes: vasculares (OR: 45), urológicas (OR: 3,3), infecciosas (OR: 2,8). Al año: rechazo agudo (OR: 11,3), nefropatía crónica del injerto (OR: 15,3) e infecciosas (OR: 9,4).
ConclusionesLa HTA y la DM son las principales etiologías de ERC. Las causas de fracaso de trasplante renal fueron vasculares e infecciosas. Se sugirieron probables factores de riesgo de importancia estadística y clínica, pero es necesario un mayor tamaño de muestra para hacer más robusta la evidencia estadística.
CKD has become one of the most prevalent diseases in the past decades. Estimated through the application of the modification of diet in renal disease (MDRD) formula, world prevalence ranges between 3% and 21.8%.1–3 However, this figure is relatively low in Colombia (0.87%), because early clinical stages are usually asymptomatic and go undetected and are also underestimated due to the lack of early detection.4 Consequently, renal transplant has become an alternative to dialysis for improving the quality of life of these patients.
According to the United States Organ Transplantation OPTN & SRTR Annual Data Report 2010, there were 17,588 patients on the waiting list in 1998 and this number had increased to 29,031 by 2009. The number of renal transplants increased by 34% between 2008 and 2009.5 In 2010, Colombia was 26 in the world in the number of deceased kidney donor transplants, with a rate of 19.2% for every one million inhabitants. In the first half of 2011, the waiting list for renal transplant grew by 46.5% compared with the same period in 2010, from 724 to 1061.6
There is a pressing challenge to optimize surgical and management protocols for renal transplants in order to ensure the highest success rates possible. A series of factors have been suggested to influence transplant outcomes, and they should be subject of tighter control and further study. These include age, gender, cold ischemia time, time in dialysis, HLA compatibility, and anemia, among others.7,8
The objective of this study was to determine the causes that contribute to the loss of deceased kidney donor transplants in a cohort of patients seen between February 2007 and November 2012 at Fundación Surcolombiana de Trasplantes.
Materials and methodsType of studyRetrospective cohort study.
Population and sampleThe study population were all patients with kidney transplantation at Hospital Universitario de Neiva, Colombia, between February 2007 and November 2011.
Definition of transplant lossTransplant loss was defined as every biopsy-confirmed graft loss that did not respond to medical or surgical treatment, having to return to dialysis therapy. Death of recipient with functional graft due to reasons related to their disease and the transplant was also included.
VariablesIndependent variables were age, donor and recipient age, marital status, gender, occupation, schooling, socioeconomic bracket, insurance, religion, area of residence, area of origin, recipient comorbidities, cause of renal disease, time in dialysis before transplantation, type of previous dialysis, number of HLA compatibilities, qualitative Panel Reactivity Antibody (PRA) I and II, time of cold ischemia, post-transplant complications, hemoglobin, blood pressure, triglycerides, total cholesterol, 24-h proteinuria, creatinine clearance, blood sugar, creatinine, blood urea nitrogen (BUN), and body mass index before transplant, 1 month, six months and 12 months after transplantation. Dependent variables: graft loss or recipient death.
Data collectionData were collected from a database supplied under authorization by Fundación Surcolombiana de Trasplantes. The information contained in the clinical records was validated using a checklist. Five clinical records were excluded by random selection for the pilot test.
Data processing and analysisThe information was processed using version 11.1 of the STATA software package. A descriptive univariate analysis was applied initially, and proportions, ratios and means were obtained. Then, a bivariate analysis was conducted using odds ratio (OR), 95% confidence interval (95% CI), Exact Fisher test, with a significance level of p<0.05.
Ethical considerationsThis was a no-risk research in accordance with Resolution 8430/1993, approved by the Ethics Committee of Universidad Surcolombiana, Neiva, Colombia.
ResultsDuring the study period, a total of 165 patients underwent renal transplantation. Of them, 5 were excluded for the pilot test, and 160 clinical records were finally included.
Univariate analysis- 1.
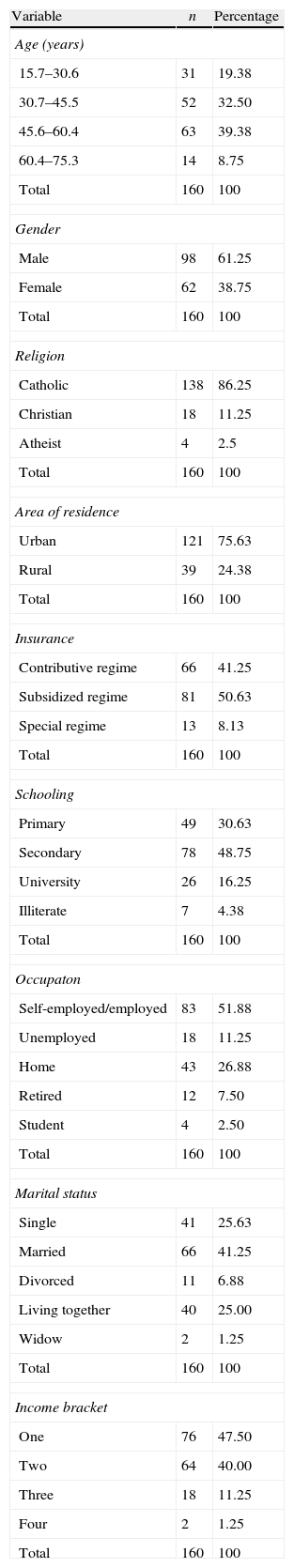
Socioeconomic characterization (Table 1). The study sample was heterogeneous in terms of the majority of the characteristics. Of the sample, 61.25% were males with ages ranging between 30 and 60 years (71.88%); however, extreme values were observed, at 15 and 75 years of age.
Table 1.Percent distribution of socioeconomic characteristics.
Variable n Percentage Age (years) 15.7–30.6 31 19.38 30.7–45.5 52 32.50 45.6–60.4 63 39.38 60.4–75.3 14 8.75 Total 160 100 Gender Male 98 61.25 Female 62 38.75 Total 160 100 Religion Catholic 138 86.25 Christian 18 11.25 Atheist 4 2.5 Total 160 100 Area of residence Urban 121 75.63 Rural 39 24.38 Total 160 100 Insurance Contributive regime 66 41.25 Subsidized regime 81 50.63 Special regime 13 8.13 Total 160 100 Schooling Primary 49 30.63 Secondary 78 48.75 University 26 16.25 Illiterate 7 4.38 Total 160 100 Occupaton Self-employed/employed 83 51.88 Unemployed 18 11.25 Home 43 26.88 Retired 12 7.50 Student 4 2.50 Total 160 100 Marital status Single 41 25.63 Married 66 41.25 Divorced 11 6.88 Living together 40 25.00 Widow 2 1.25 Total 160 100 Income bracket One 76 47.50 Two 64 40.00 Three 18 11.25 Four 2 1.25 Total 160 100 Source: Own.Patients in the medium-low socioeconomic brackets were 47.5%; 65% had secondary or higher education. In terms of occupation, 51.88% worked and only 11.25% appeared as unemployed. Three out of 4 patients lived in urban areas, considering that they hay to travel to the city in order to have easy access to follow-up. In terms of insurance, half of the sample (50.63%) belonged to the subsidized healthcare regime, less than 10% were under the special regime, and the rest belonged to the contributive regime.
- 2.
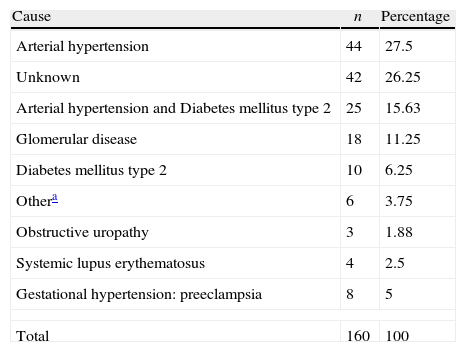
Causes of CKD. There were multiple causes of CKD. In the study, almost half (49.38%) were related to the two main chronic ailments of this century: HTN and DM. In a few cases, it was not clear which was the first to be diagnosed and which had been responsible for renal injury (Table 2).
Table 2.Percent distribution of the causes of end-stage chronic kidney disease.
Cause n Percentage Arterial hypertension 44 27.5 Unknown 42 26.25 Arterial hypertension and Diabetes mellitus type 2 25 15.63 Glomerular disease 18 11.25 Diabetes mellitus type 2 10 6.25 Othera 6 3.75 Obstructive uropathy 3 1.88 Systemic lupus erythematosus 4 2.5 Gestational hypertension: preeclampsia 8 5 Total 160 100 Source: Own. - 3.
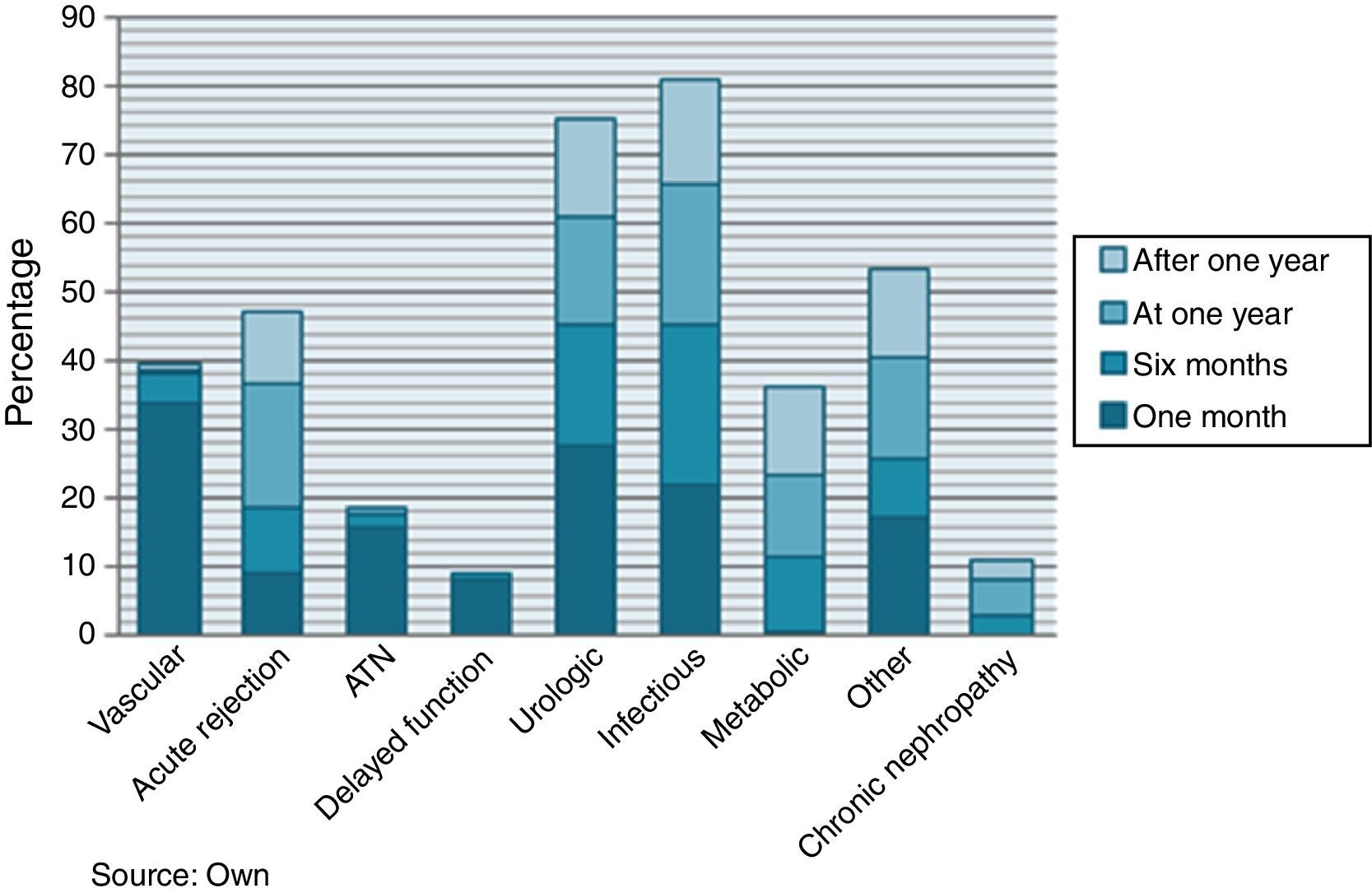
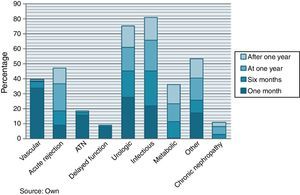
Post-transplant complications (Fig. 1). After 1 month, the two main complications were vascular (33.75%) and urologic (27.5%), associated with problems during surgery and surgical wound problems: infection, seroma, hematoma and eventration in 8.7%.
One year after transplantation, there was an increase in the proportion of acute rejection episodes (18.38%) and chronic graft nephropathy (5.15%). Infectious complications remained constant throughout the follow-up period, as was also the case with metabolic complications (dyslipidemia and de novo diabetes), although in a smaller percentage. Neoplasms (skin and cervix) appeared after the first year in 3.9% of cases.
Vascular complications during the first three months included post-operative bleeding requiring transfusion (11.2%) and perirenal hematoma (10.6%).
Urinary tract infection (UTI) was the most frequent urologic complication found throughout the entire follow-up period (21.8% at one month, 17.1% at six months and 11.7% at one year). Other urologic complications included urinary leak (6.2% at one month; 1.3% at 6 months) and urinoma (1.2% at one month).
Bacteria were the main etiologic factor in post-transplant infections (17.5% at one month, 16.44% at 6 months and 16.18% at one year), followed by cytomegalovirus (CMV) (2.5% at one month, 8.22% at six months and 2.94% at one year).
- 4.
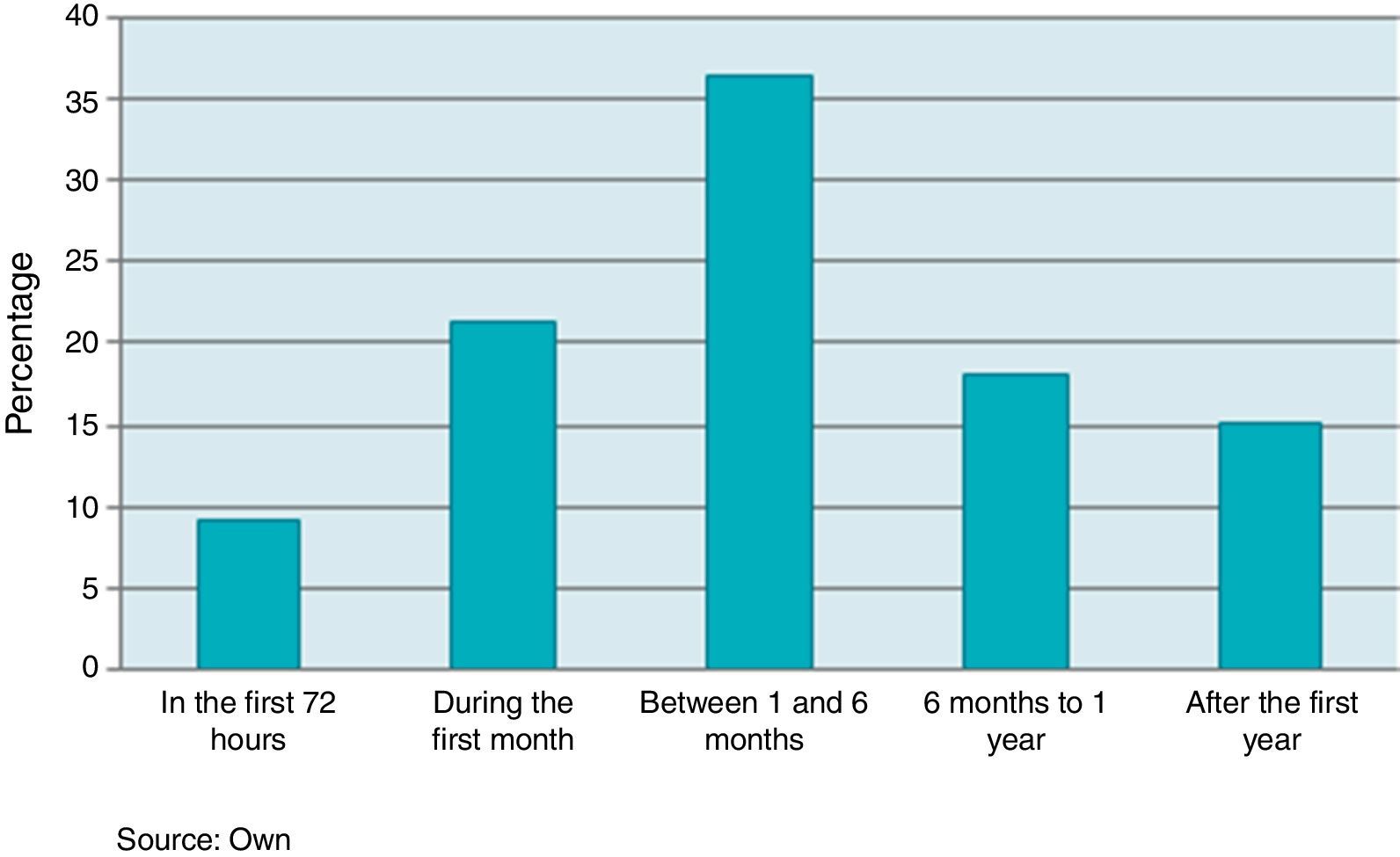
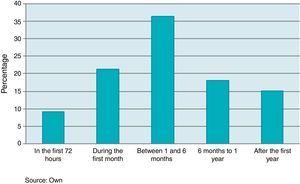
Success/failure prevalence in renal transplants. Failure prevalence was 20% with a ratio of 1 failure for every 5 transplants. Of those, 33.3% were related to recipient demise.
- 5.
Time during which cases occurred (Fig. 2). Over the first 72h, 9% of the transplants were lost; the peak of highest prevalence occurred during the first 6 months (66.6%).
- 6.
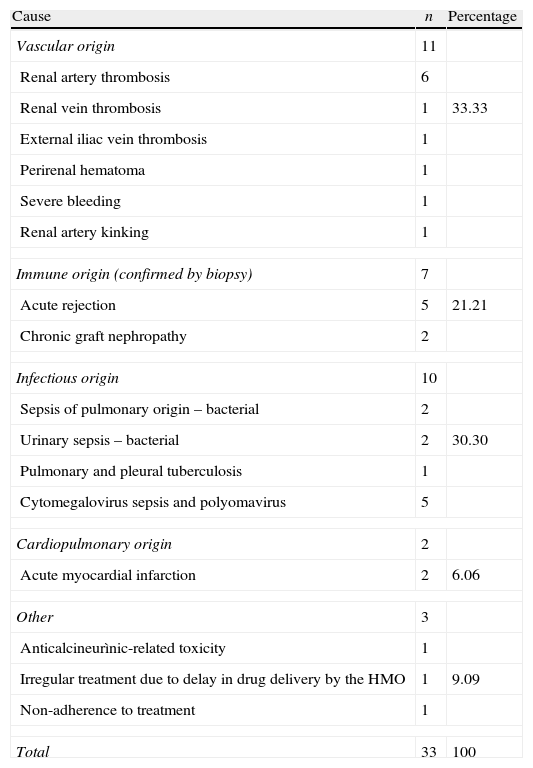
Immediate cause of recipient death or graft loss (Table 3). The main cause of immediate transplant loss was of vascular origin (33.3%), but no correlation was found with the organ rescue procedure; the second cause was infection (30.3%). One out of every five losses was due to immune failure.
Table 3.Percent distribution of immediate causes of recipient demise or graft loss.
Cause n Percentage Vascular origin 11 Renal artery thrombosis 6 Renal vein thrombosis 1 33.33 External iliac vein thrombosis 1 Perirenal hematoma 1 Severe bleeding 1 Renal artery kinking 1 Immune origin (confirmed by biopsy) 7 Acute rejection 5 21.21 Chronic graft nephropathy 2 Infectious origin 10 Sepsis of pulmonary origin – bacterial 2 Urinary sepsis – bacterial 2 30.30 Pulmonary and pleural tuberculosis 1 Cytomegalovirus sepsis and polyomavirus 5 Cardiopulmonary origin 2 Acute myocardial infarction 2 6.06 Other 3 Anticalcineurìnic-related toxicity 1 Irregular treatment due to delay in drug delivery by the HMO 1 9.09 Non-adherence to treatment 1 Total 33 100 Source: Own. - 7.
Other variables. Of the donors, 76.87% were under 50 years of age. This means that 1 out of every 4 donors had expanded criteria. Cold ischemia time was less than 13h in 62.5% of patients, and only 2.5% were in the borderline range of 25–30h.
Of the total number of patients, 88.13% were in dialysis for more than 1 year, only 25% were in dialysis for less than 7.5 months, and 53.13% had hemodialysis.
Three patients were retransplanted (1.88%). PRA classes I and II were negative in more than 75% and 92.5% of patients, respectively. The number of HLA compatibilities ranged between a minimum of 2 and a maximum of 6.
- 8.
Follow-up of paraclinical variables. Creatinine showed greater pre-transplant variability when compared with the 1-year results, going from 4mg/dl in 90% of patients to 2mg/dl in 9.4%.There was a tendency to develop anemia in patients with transplant failure, with median values below 11.5g/dl. There was good control of blood sugar, triglycerides and cholesterol during the follow-up period, with a median below 100mg/dl, 200mg/dl and 196mg/dl, respectively. Body mass index varied during follow-up, with a peak at 6 months in the cases (median of 26) and at 1 month in the controls (25).
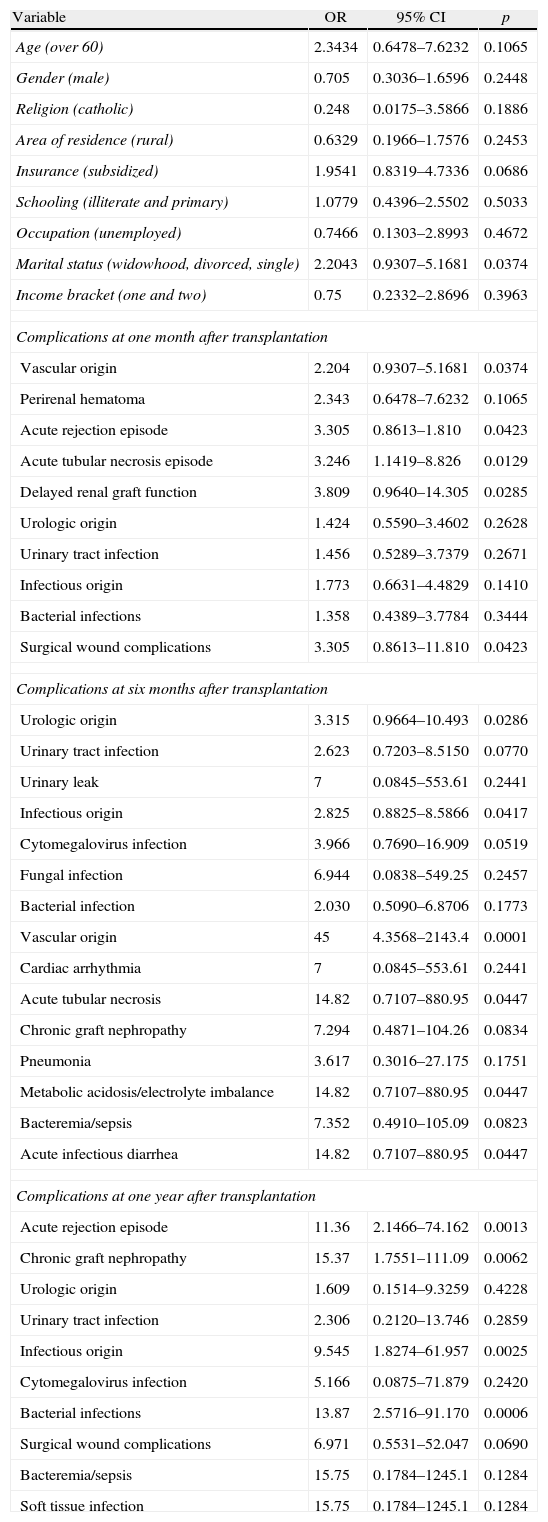
Age over 60 (OR: 2.34), belonging to the subsidized health regime (OR: 1.95), and single or divorced marital status (OR: 2.2) were probable risk factors, but it is believed that the latter may be a confounding variable.
Bivariate model of socioeconomic characteristics and post-transplant complications in relation to renal transplant outcomes.
| Variable | OR | 95% CI | p |
| Age (over 60) | 2.3434 | 0.6478–7.6232 | 0.1065 |
| Gender (male) | 0.705 | 0.3036–1.6596 | 0.2448 |
| Religion (catholic) | 0.248 | 0.0175–3.5866 | 0.1886 |
| Area of residence (rural) | 0.6329 | 0.1966–1.7576 | 0.2453 |
| Insurance (subsidized) | 1.9541 | 0.8319–4.7336 | 0.0686 |
| Schooling (illiterate and primary) | 1.0779 | 0.4396–2.5502 | 0.5033 |
| Occupation (unemployed) | 0.7466 | 0.1303–2.8993 | 0.4672 |
| Marital status (widowhood, divorced, single) | 2.2043 | 0.9307–5.1681 | 0.0374 |
| Income bracket (one and two) | 0.75 | 0.2332–2.8696 | 0.3963 |
| Complications at one month after transplantation | |||
| Vascular origin | 2.204 | 0.9307–5.1681 | 0.0374 |
| Perirenal hematoma | 2.343 | 0.6478–7.6232 | 0.1065 |
| Acute rejection episode | 3.305 | 0.8613–1.810 | 0.0423 |
| Acute tubular necrosis episode | 3.246 | 1.1419–8.826 | 0.0129 |
| Delayed renal graft function | 3.809 | 0.9640–14.305 | 0.0285 |
| Urologic origin | 1.424 | 0.5590–3.4602 | 0.2628 |
| Urinary tract infection | 1.456 | 0.5289–3.7379 | 0.2671 |
| Infectious origin | 1.773 | 0.6631–4.4829 | 0.1410 |
| Bacterial infections | 1.358 | 0.4389–3.7784 | 0.3444 |
| Surgical wound complications | 3.305 | 0.8613–11.810 | 0.0423 |
| Complications at six months after transplantation | |||
| Urologic origin | 3.315 | 0.9664–10.493 | 0.0286 |
| Urinary tract infection | 2.623 | 0.7203–8.5150 | 0.0770 |
| Urinary leak | 7 | 0.0845–553.61 | 0.2441 |
| Infectious origin | 2.825 | 0.8825–8.5866 | 0.0417 |
| Cytomegalovirus infection | 3.966 | 0.7690–16.909 | 0.0519 |
| Fungal infection | 6.944 | 0.0838–549.25 | 0.2457 |
| Bacterial infection | 2.030 | 0.5090–6.8706 | 0.1773 |
| Vascular origin | 45 | 4.3568–2143.4 | 0.0001 |
| Cardiac arrhythmia | 7 | 0.0845–553.61 | 0.2441 |
| Acute tubular necrosis | 14.82 | 0.7107–880.95 | 0.0447 |
| Chronic graft nephropathy | 7.294 | 0.4871–104.26 | 0.0834 |
| Pneumonia | 3.617 | 0.3016–27.175 | 0.1751 |
| Metabolic acidosis/electrolyte imbalance | 14.82 | 0.7107–880.95 | 0.0447 |
| Bacteremia/sepsis | 7.352 | 0.4910–105.09 | 0.0823 |
| Acute infectious diarrhea | 14.82 | 0.7107–880.95 | 0.0447 |
| Complications at one year after transplantation | |||
| Acute rejection episode | 11.36 | 2.1466–74.162 | 0.0013 |
| Chronic graft nephropathy | 15.37 | 1.7551–111.09 | 0.0062 |
| Urologic origin | 1.609 | 0.1514–9.3259 | 0.4228 |
| Urinary tract infection | 2.306 | 0.2120–13.746 | 0.2859 |
| Infectious origin | 9.545 | 1.8274–61.957 | 0.0025 |
| Cytomegalovirus infection | 5.166 | 0.0875–71.879 | 0.2420 |
| Bacterial infections | 13.87 | 2.5716–91.170 | 0.0006 |
| Surgical wound complications | 6.971 | 0.5531–52.047 | 0.0690 |
| Bacteremia/sepsis | 15.75 | 0.1784–1245.1 | 0.1284 |
| Soft tissue infection | 15.75 | 0.1784–1245.1 | 0.1284 |
The cause of renal disease of idiopathic origin was a probable risk factor (OR: 10.5, p: 0.0006). PRA class II (OR: 4.48), cold ischemia time longer than 13h (OR: 2.07) and donor age greater than 50 (OR: 2.8) were probable risk factors for transplant failure. However, only the first two variables were statistically significant.
Creatinine levels higher than 2mg/dl and blood urea nitrogen greater than 20mg/dl were associated with transplant failure at one month and at 6 months. Likewise, proteinuria>300mg/dl and hemoglobin lower than 12g/dl were associated with transplant failure at 6 months.
DiscussionIn an effort to improve quality of life for patients with end-stage CKD, renal transplant has become the best option. The surgical technique and the immunosuppressive therapies have come to play a key role in the success of this form of treatment. This study assessed the most relevant factors in the literature and characterized the transplanted population in southern Colombia.
In patients 1 year after transplant and a sample of 85,135 people, Siddiqi et al.8 found that older donor age, male gender and HLA incompatibility were risk factors for renal transplant failure. In this work, 61.25% were males but that variable was not found to be a risk factor (OR: 0.705, p: 0.2448). The percentage of donors with expanded criteria in the sample was 23.13%, and it was associated as a possible risk factor (OR: 2.8, p: 0.0501). No association was found with HLA (OR: 1.096, p: 0.50).
In the study by Hernández et al.9 there was predominance of male patients between the ages of 35 and 48 years with similar characteristics as those in this study. The most frequent medical complication was UTI, while surgical complications included surgical wound problems (16.87%), perirenal hematoma (10%) and urinary leak (6.87%). They suggest donor and recipient age, recipient gender, cause of donor death, cold ischemia times, cause of the CKD, preservation solution, time on dialysis and acute tubular necrosis (ATN) as possible factors associated with survivorship.
In the local study, donor and recipient age and time on dialysis were not significant (p>0.05); however, cold ischemia time (OR: 2.07, p: 0.0492), the cause of CKD (OR: 10.5, p:0.0006) and ATN (OR 3.24, p: 0.0129) were probable risk factors for transplant failure.
Ruiz-George et al.10 conducted a cross-sectional study to assess prolonged cold ischemia as a potential factor for acute graft rejection in deceased donor graft. In a sample of 33 patients, they found prolonged cold ischemia time (OR=8.4, CI=1.5–44.2, p=0.02) as a possible risk factor for acute rejection. Our results at Fundación Surcolombiana de Trasplantes were similar, although in 62.5% of cases, ischemia time was shorter than 13h.
Our findings in this study were similar to those of Álvarez González et al.11 In our study, 88.13% of the patients had been on dialysis for more than 12 months before transplantation, and this is a probable risk factor for failure (OR: 1.44, p: 0.418).
In a retrospective cohort study with 1676 patients followed out to one year, Regina de Sousa et al.12 found a 49% incidence of infection, with a higher frequency during the first months after transplantation. Infections included UTIs (31.3%), CMV (12%), surgical wound infection (10.3%), and herpes simplex (9.1%). In our study population, bacterial infections were more frequent, including UTIs, most of them with septic complications and bacteremias, followed by CMV.
Between 2007 and 2009, Rivera et al.13 conducted a case series study at Hospital Universitario de Neiva with 54 patients on the anesthetic complications in renal transplant. Their findings correlate with the current results where 61% were males, 50% between 40 and 60 years of age. HTN was the most frequent comorbidity (94%), followed by de glomerulonephritis (22%) and DM (17%). However, we believe that it is difficult to determine comorbidity significance from the clinical standpoint, because there may be diseases secondary to renal disease and/or causes of it.
ConclusionsDiabetes mellitus Type 2 and arterial hypertension continue to be the main causes of end-stage chronic kidney disease.
The main surgical complications in the group of transplanted patients were surgical wound problems, post-operative bleeding and perirenal hematoma. The main medical complication was infection, with a peak at six months after transplantation, due to the susceptibility to opportunistic infections following immunosuppressive therapy, comparable to the literature.
The main factors leading to graft loss or death of the recipient were vascular and infectious during the first six months after transplantation.
Failure:success ratio in patients transplanted at Hospital Universitario de Neiva between February 2007 and November 2012 was approximately 1 for every 5 transplants.
We suggest conducting clinical and laboratory follow-up on a weekly basis following transplantation during the first two months, and then biweekly for the first six months, with tighter infection control.
We suggest potential risk factors of clinical importance and relevance, but a larger sample size is needed in order to produce more statistically robust evidence.
FundingNo funding.
Conflict of interestThe authors have no conflicts of interest to declare.
To the Fundación Surcolombiana de Transplantes, to professors Dolly Castro Betacourth, Fabio Rivas and Alexandra Porras, advisers of the Epidemiology Program of the Universidad Surcolombiana.
Please cite this article as: Cubillos Gutiérrez J, Sandoval Riveros CL, Andrade Cerquera E, Hermida Gutiérrez NH. Causas que contribuyen a la pérdida del trasplante renal de donante cadavérico en la Fundación Surcolombiana de Trasplantes. Febrero 2007 a noviembre de 2012, Neiva, Colombia. Rev Colomb Anestesiol. 2014;42:83–89.