In Colombia, one out of five women between the ages of 15 and 19 years have been pregnant. Almost two-thirds (64%) of these pregnancies were unplanned.
ObjectivesTo examine the socio-demographic, psychosocial and clinical risk factors associated with adolescent pregnancy.
MethodsAn analytical prevalence study was performed using secondary data from the First Demographic Study of Mental Health in Medellin, Colombia. Female adolescents between 13 and 19 years of age were included in the study. The population was evaluated using the Composite International Diagnosis Interview, a structured interview developed by the World Health Organization, which establishes diagnoses according to the DSM-IV and ICD-10 criteria.
ResultsA sample of 499 female adolescents was obtained, in which 135 adolescent pregnancies were identified, representing a prevalence of 21.5%. The large majority (84.4%) were between 16 and 19 years old. The median age was 17 years, with an interquartile range of 2 years. Almost two-thirds (61.2%) of female adolescents had initiated sexual activity at the age of 15 or later. Almost one-third (31.9%) reported being physically abused during childhood, and 6.7% sexually abused. Of those who were pregnant, 66.7% reported previous sexual abuse. A bivariate analysis showed that sexual abuse (OR=7.68), childhood negligence (OR=4.33), and having a partner (OR=6.31) were factors associated with an adolescent pregnancy.
ConclusionsNegligence and sexual abuse in childhood and adolescence can be prevented, and adolescent pregnancies can be decreased. This finding has important implications for clinical management and prognosis, and requires public preventive policies.
En Colombia, 1 de cada 5 mujeres de 15–19 años ha estado embarazada. El 64% de estos embarazos no fueron planeados.
ObjetivoExplorar los factores sociodemográficos, psicosociales y clínicos asociados con el embarazo adolescente.
MétodosEstudio de prevalencia analítica, de fuente secundaria (Primer Estudio Poblacional de Salud Mental Medellín). La muestra fue evaluada usando el Compositum International Diagnosis Interview, instrumento desarrollado por la Organización Mundial de la Salud para realizar diagnósticos con base en criterios diagnósticos del DSM-IV y el CIE-10.
ResultadosSe obtuvo una muestra de 499 adolescentes. Se identificaron 135 embarazos adolescentes, lo que lleva a una prevalencia de embarazo adolescente del 21,5%. El 84,4% de las adolescentes embarazadas tenían entre 16 y 19 años, y la edad mediana era 17 [intervalo intercuartílico, 2] años. El 61,2% de ellas iniciaron la vida sexual a los 15 años. Del total de adolescentes, el 31,9% afirmaba haber sufrido maltrato físico y el 6,7%, haber sido violadas en la niñez. Del subgrupo de embarazadas, el 66,7% reportó haber sufrido violación. En el modelo bivariable, las variables que mostraron asociación con el embarazo adolescente fueron ser víctima de violación (odds ratio [OR]=7,68), negligencia en la niñez (OR=4,33) y tener pareja (OR=6,31).
ConclusionesLa negligencia y el abuso sexual en la infancia pueden evitarse buscando impactar positivamente el embarazo adolescente.
Adolescence is defined as the period between 10 and 19 years of age. According to the World Health Organization (WHO),1 in 2008 16 million babies were born to mothers aged 15–19 years worldwide, representing 11% of all births. 95% of these births were in low- and middle-income countries.
In Colombia, 1 in 5 girls between the ages of 15 and 19 has been pregnant and 64% of these pregnancies were unplanned. The 19.5% prevalence of adolescent pregnancies2,3 is a long way off the Millennium Development Goal (MDG) target of 15%, set by Colombia in 2000 in what has come to be known as the Millennium Declaration.4 The factors that have been associated with adolescent pregnancy in Colombia are a low level of education, family violence, poor access to information on sexual health and contraception, a low socio-economic level, poor communication with parental figures, level of urbanisation, supply of reproductive sexual health services, age at onset of sexual relations and cultural and regional factors.5,6
Among the various consequences of adolescent pregnancy is the increased prevalence of unsafe abortion, disability, maternal, neonatal and infant mortality, low birth weight newborns, increased drug use in pregnancy, low levels of education and higher fertility rates.7
As well as negative consequences on the biological side, pregnancy in adolescence entails severe risks that destabilises overall wellbeing and life expectancies: it leads to desertion and/or discrimination in educational and social contexts; an early connection to the labour market; greater likelihood of entering production chains of underemployment or other unstable forms of working relationships; family and emotional tensions; and rearranging or deviating from lifetime projects.7
The objective of this study was to determine the socio-demographic, clinical and familial factors and upbringing patterns associated with adolescent pregnancy in Medellín (Colombia).
MethodsAn analytical cross-sectional study based on a secondary information source. The study population was made up of non-institutionalised female adolescents residing in the city of Medellín who, according to the 2011 forecasts of the Colombian National Administrative Department of Statistics (DANE), accounted for 125,159 girls between the ages of 13 and 19 years.2 The study sample size was calculated with a population size estimation formula, with a 95% confidence level, 5% precision and an estimated prevalence of 6.9% (expected prevalence of depression, according to the results of the 2003 National Study of Mental Health) and a design effect of 1.0.8 The chosen design was probabilistic and multi-stage, the objective of which was the adolescent population aged between 13 and 19 years, selected using the sampling framework that comprised all homes located on the different socio-economic strata within the 16 boroughs (urban area) and five townships (rural area) of the city of Medellín. Out of 499 adolescent females, 135 were selected, who stated that they had had previous sexual relations.
The dependent variable of the study was adolescent pregnancy, which was constructed using the information yielded by the following questions: “How many living biological children do you have?”; “Have you ever lost a child due to miscarriage or stillbirth?”; and “Have you ever had an abortion?” The following independent variables were included: socio-demographic (age, level of education, marital status, place of residence, employment activity), neglect, physical or sexual abuse, parental history of mental problems (depression, anxiety, suicidal behaviour, alcohol consumption, upbringing-related situations), sexual activity (age at onset of sexual relations, condom use, number of partners in the past year), use of mental health services, mental disorders in the adolescent (major depression, bipolar I or II disorder, post-traumatic stress disorder, suicidal ideation and attempted suicide), disorders arising in infancy, childhood or adolescence (oppositional defiant disorder, behaviour disorder and attention deficit hyperactivity disorder).
The secondary information source was the database of the primary study known as the “First Population Mental Health Study of Medellín, 2011–2012”, conducted by CES University, Harvard University and the Health Secretariat of Medellín. The instrument employed was the Composite International Diagnostic Interview (CIDI 3.0), developed by the WHO and the Alcohol, Drug Abuse and Mental Health Administration (ADAMHA). The CAPI version was used, which was adapted in Medellín to ensure its cultural and linguistic sensitivity.9,10 The instrument was applied by non-clinical interviewers who were duly trained and standardised.
The instrument was composed of two parts: the first identified the subjects at risk of suffering some kind of mental disorder and the second estimated the prevalence and severity of 21 mental disorders in accordance with the criteria of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) and the International Classification of Diseases (ICD-10).
Qualitative variables were described with absolute and relative frequencies, while the median [interquartile range] was used for age due to the fact that the variable did not present normal distribution. In order to compare the dependent variable with other qualitative variables, the χ2 test of independence and the Mann–Whitney U test were used for age. Association was explored using the odds ratio (OR), considering statistical association if p is <0.05 and there is a 95% confidence interval (95% CI). The variables that showed statistical significance in the bivariate analysis were included in the binary logistic regression model to obtain adjusted odds ratios (ORa).
The polytomous variables (neglect, physical abuse, condom use, marital status and level of education) were recategorised for the bivariate and multivariate models, and grouped into two categories (yes and no). Neglect and physical abuse were grouped into the following categories: “often”, “sometimes” and “hardly ever”, in the “yes” category, and “never” in the “no” category. Condom use was grouped under the “yes” category for those who always used one during sexual relations and “no” for the remaining response options. For marital status, the “has a partner” variable was created with “yes” (all categories except single) and “no” (single) categories. For the level of education variable, the “secondary studies” variable was created; “no education” and “primary” were grouped under the “no” category, with the remaining response categories placed under “yes”. This recoding was performed with the agreement of the research psychiatrists. For the data analysis, the SPSS® software, version 21.0 (SPSS Inc., Chicago, Illinois, USA), licensed to CES University, was used.
To minimise bias, a highly trained professional managed the database. Selection bias was controlled with probabilistic sampling, while information bias was controlled with trained non-clinical interviewers and the approval of the adolescents. Moreover, a globally and locally validated instrument was used. Finally, potential confounding variables were controlled using the binary logistic regression model. The primary study was approved by the CES University Research and Ethics Committee. The informed consent of one parent was also requested.
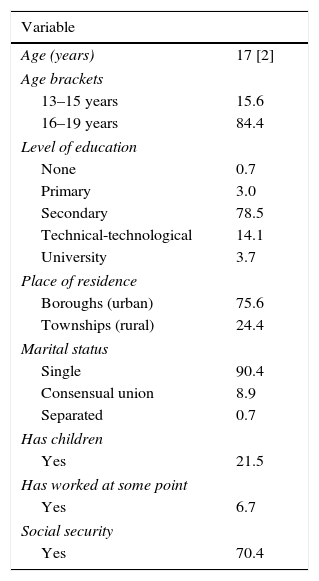
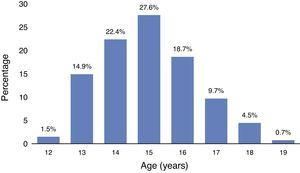
ResultsComplete information was obtained from 135 female adolescents aged between 13 and 19 years. 84.4% were aged between 16 and 19 years, while 15.6% were between 13 and 15 years. The median age was 17 [2] years. 75.6% lived in urban areas, 78.5% had completed their secondary education, 90.4% were single, 6.7% had worked at some point and 29.6% had no social security (Table 1).
Socio-demographic characteristics of adolescents with an adolescent pregnancy in the city of Medellín, 2011–2012.
| Variable | |
|---|---|
| Age (years) | 17 [2] |
| Age brackets | |
| 13–15 years | 15.6 |
| 16–19 years | 84.4 |
| Level of education | |
| None | 0.7 |
| Primary | 3.0 |
| Secondary | 78.5 |
| Technical-technological | 14.1 |
| University | 3.7 |
| Place of residence | |
| Boroughs (urban) | 75.6 |
| Townships (rural) | 24.4 |
| Marital status | |
| Single | 90.4 |
| Consensual union | 8.9 |
| Separated | 0.7 |
| Has children | |
| Yes | 21.5 |
| Has worked at some point | |
| Yes | 6.7 |
| Social security | |
| Yes | 70.4 |
The values are expressed as a percentage or median [interquartile range].
21.5% of the adolescents reported having been pregnant and 56.3% of these were aged between 16 and 17 years.
Upbringing-related variablesFor 88.1% of the adolescents, the most important maternal figure for most of their childhood was their biological mother, followed by another female relative (8.9%). As for the paternal figure, the biological father was the most important in 51.9% of cases, and in 24.9% the male figure was absent during childhood.
Perception of own mental health and seeking help for mental problemsWhere mental health problems are concerned, the professional most frequently consulted by the adolescent population was the psychologist (75%), followed by the psychiatrist and general practitioner (5.8%). None of the adolescents surveyed sought help from other specialist physicians, councillors or healers. As regards perceptions of their own mental health, 25.9% of the girls perceived it as “excellent”; 34.8% as “very good”; 31.9% as “good”; and 7.4% as “normal”.
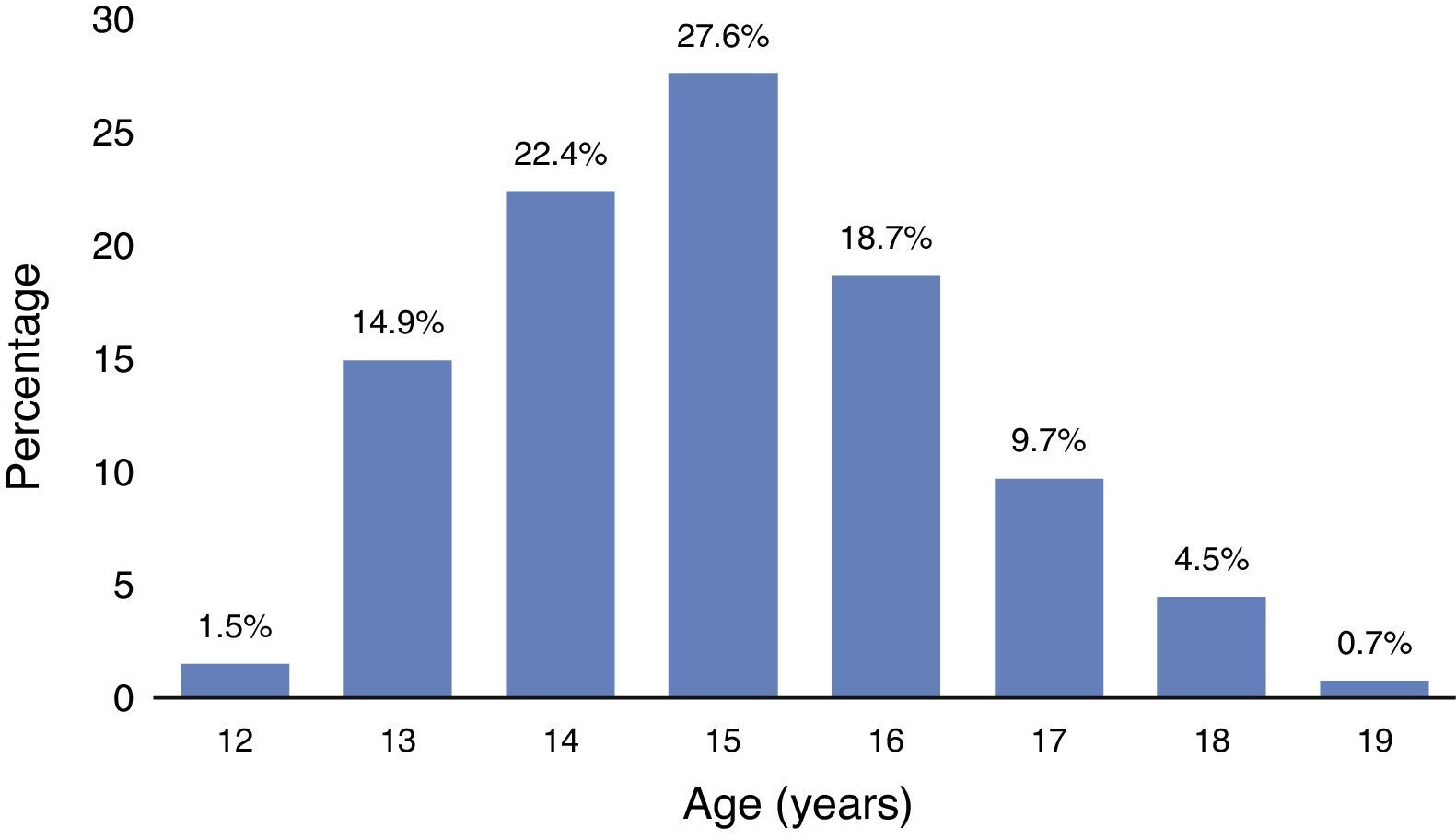
Sexuality-related elementsThe median age at onset of sexual relations was 15 [2] years (Fig. 1). In terms of the number of sexual partners in the past year, 72.0% had one partner; 10.6% two; and 3.8% three. Regarding condom use, 46.2% stated that they “always” used one; 20.5% “sometimes”; and 33.3% “never”.
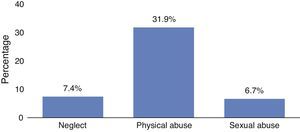
Neglect in childhood5.2% of the adolescents stated that their parents “often” failed to provide them with medical treatment when required; this “hardly ever” happened to 1.5%; and “sometimes” to 0.7%; it “never” happened to the rest of the population. 3.0% of the adolescents stated that their parents “often” gave them tasks that were too difficult or dangerous; this “sometimes” happened to 4.4%; and “almost never” happened to 8.9%; it “never” happened to the rest of the population. As regards not providing them with what they needed, such as clothes, shoes and school supplies, this “often” happened to 2.2%; “hardly ever” to 5.2%; and “never” to 92.6%. As for going hungry or not providing regular meals, this happened “often” to 1.5%; “sometimes” to 1.5%; “hardly ever” to 0.7%; and “never” to the rest of the population. 2.2% of the adolescents reported that their parents “often” left them alone when they were very young, without anyone to supervise them.
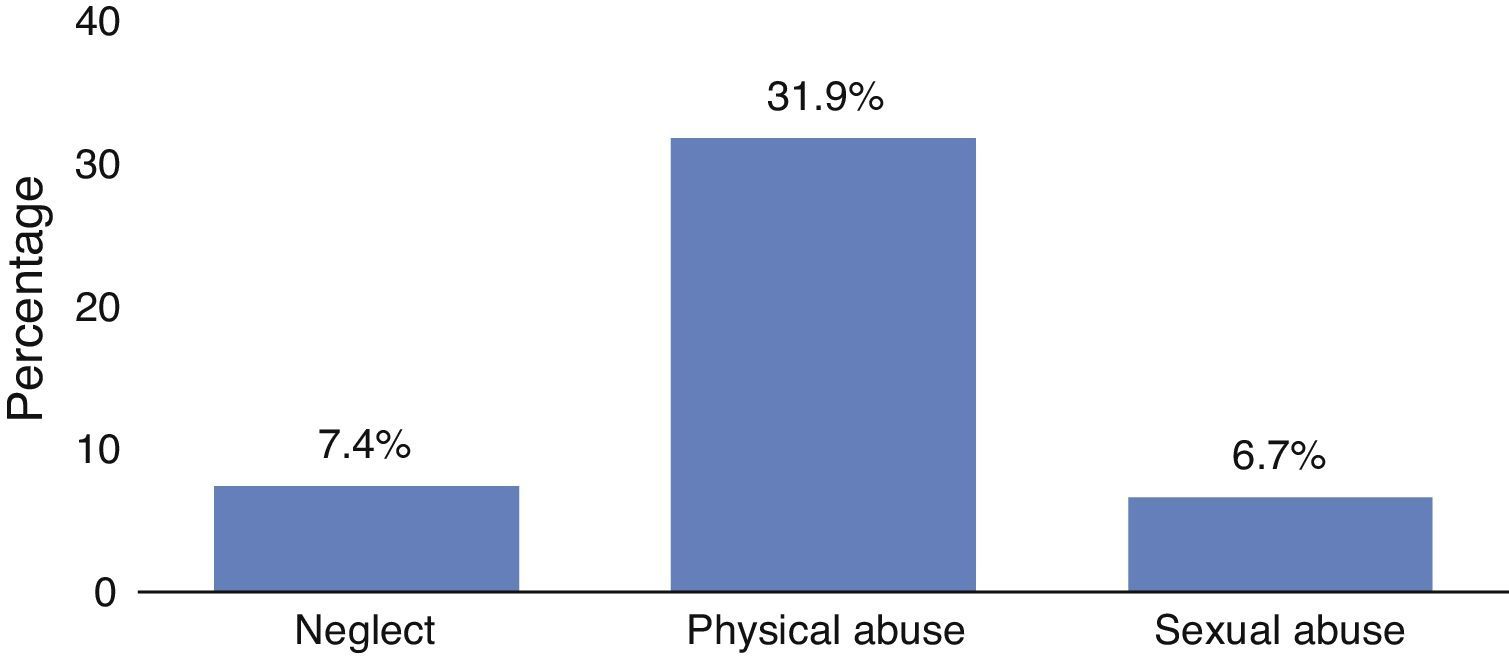
Situations of physical and sexual abuse31.9% of the adolescents stated that they were physically abused in childhood and 6.7% said they had been raped (Fig. 2). In the pregnancy subgroup, it was found that 66.7% had a history of rape.
Mental illness in the parentsFor some of the adolescents’ parents, histories of psychiatric illness were evaluated. According to the adolescents, 25.2% of mothers and 4.4% of fathers were depressed. According to the adolescents, 16.3% of mothers and 5.2% of fathers were anxious. 3.7% of mothers and 7.4% of fathers consumed alcohol and drugs, and 3% of mothers and fathers had attempted suicide at some point.
Mental disorders arising in childhood and adolescence11.9% of the adolescents met the criteria for oppositional defiant disorder; 6.7% for attention deficit hyperactivity disorder; and 3.7% for behaviour disorder.
Other mental disordersAs regards affective disorders, 19.3% of the adolescents met the criteria for major depression; 7.4% for post-traumatic stress disorder; 3.7% for bipolar I or II disorder; and 0.7% for generalised anxiety disorder. As for suicidal behaviour, 36.3% had had suicidal ideation and 21.5% had attempted suicide at least once.
In terms of substance use disorders, 5.9% met the criteria for alcohol abuse and 3.0% for alcohol dependence. As regards drugs, 7.4% presented abuse and 3.0% dependence.
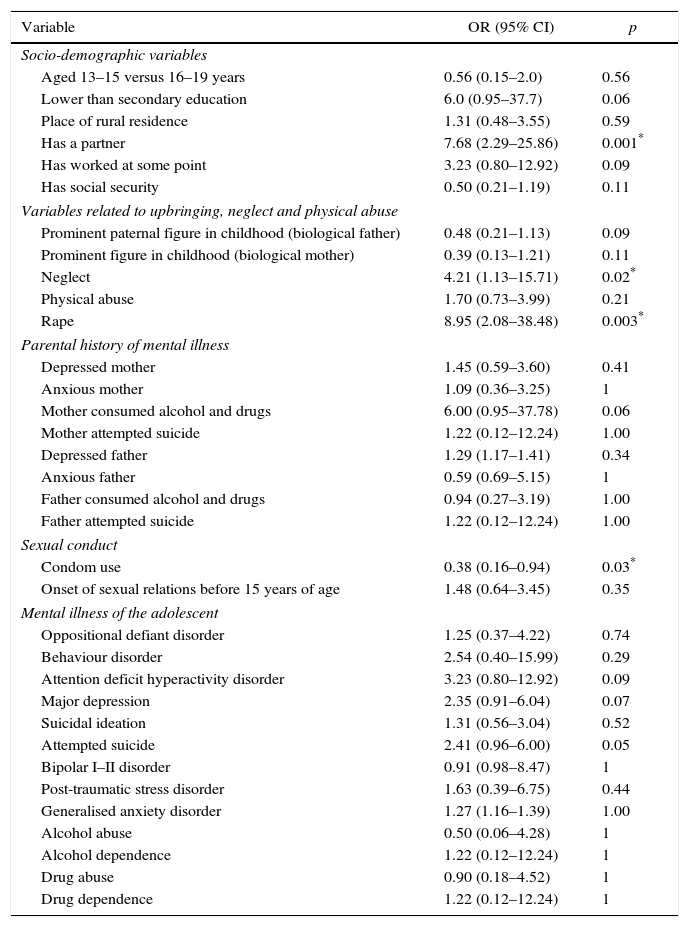
Bivariate analysisThe dependent variable (adolescent pregnancy) was compared to all the variables included in the study. The following were found to be risk factors for pregnancy: history of rape (OR=8.95; 95% CI, 2.1–38.4; p<0.003), situations of childhood neglect (OR=4.21; 95% CI, 1.1–15.7; p<0.022), and having a partner (OR=7.68; 95% CI, 2.29–25.86; p=0.001). Condom use was found to be a protective factor (OR=0.38; 95% CI, 0.16–0.94; p=0.03) (Table 2).
Bivariate model. Association between adolescent pregnancy and the socio-demographic, socio-familial and clinical variables included in the study.
| Variable | OR (95% CI) | p |
|---|---|---|
| Socio-demographic variables | ||
| Aged 13–15 versus 16–19 years | 0.56 (0.15–2.0) | 0.56 |
| Lower than secondary education | 6.0 (0.95–37.7) | 0.06 |
| Place of rural residence | 1.31 (0.48–3.55) | 0.59 |
| Has a partner | 7.68 (2.29–25.86) | 0.001* |
| Has worked at some point | 3.23 (0.80–12.92) | 0.09 |
| Has social security | 0.50 (0.21–1.19) | 0.11 |
| Variables related to upbringing, neglect and physical abuse | ||
| Prominent paternal figure in childhood (biological father) | 0.48 (0.21–1.13) | 0.09 |
| Prominent figure in childhood (biological mother) | 0.39 (0.13–1.21) | 0.11 |
| Neglect | 4.21 (1.13–15.71) | 0.02* |
| Physical abuse | 1.70 (0.73–3.99) | 0.21 |
| Rape | 8.95 (2.08–38.48) | 0.003* |
| Parental history of mental illness | ||
| Depressed mother | 1.45 (0.59–3.60) | 0.41 |
| Anxious mother | 1.09 (0.36–3.25) | 1 |
| Mother consumed alcohol and drugs | 6.00 (0.95–37.78) | 0.06 |
| Mother attempted suicide | 1.22 (0.12–12.24) | 1.00 |
| Depressed father | 1.29 (1.17–1.41) | 0.34 |
| Anxious father | 0.59 (0.69–5.15) | 1 |
| Father consumed alcohol and drugs | 0.94 (0.27–3.19) | 1.00 |
| Father attempted suicide | 1.22 (0.12–12.24) | 1.00 |
| Sexual conduct | ||
| Condom use | 0.38 (0.16–0.94) | 0.03* |
| Onset of sexual relations before 15 years of age | 1.48 (0.64–3.45) | 0.35 |
| Mental illness of the adolescent | ||
| Oppositional defiant disorder | 1.25 (0.37–4.22) | 0.74 |
| Behaviour disorder | 2.54 (0.40–15.99) | 0.29 |
| Attention deficit hyperactivity disorder | 3.23 (0.80–12.92) | 0.09 |
| Major depression | 2.35 (0.91–6.04) | 0.07 |
| Suicidal ideation | 1.31 (0.56–3.04) | 0.52 |
| Attempted suicide | 2.41 (0.96–6.00) | 0.05 |
| Bipolar I–II disorder | 0.91 (0.98–8.47) | 1 |
| Post-traumatic stress disorder | 1.63 (0.39–6.75) | 0.44 |
| Generalised anxiety disorder | 1.27 (1.16–1.39) | 1.00 |
| Alcohol abuse | 0.50 (0.06–4.28) | 1 |
| Alcohol dependence | 1.22 (0.12–12.24) | 1 |
| Drug abuse | 0.90 (0.18–4.52) | 1 |
| Drug dependence | 1.22 (0.12–12.24) | 1 |
95% CI: 95% confidence interval; OR: odds ratio.
The subgroup of adolescents with a history of rape was analysed. 66.7% of the cases occurred when the girls were aged ≤12 years. 43.3% reported having been raped “more than once”, with no correlation to adolescent pregnancy (OR=1.00; 95% CI, 0.53–18.91; p=1). The prevalence of major depression in this subgroup was 19.2%, and a significant association was found with a history of rape (OR=6.25; 95% CI, 1.54–25.23; p=0.013). Attempted suicide was seen in 20.7% of this subgroup and was significantly associated with adolescent pregnancy (OR=8.95; 95% CI, 2.085–38.48; p=0.003).
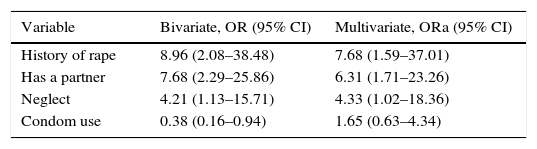
Multivariate analysisThe variables that showed statistical association in the bivariate model (history of rape, having a partner, history of neglect in childhood and condom use) were included in a binary logistic regression model that controlled confounding variables and calculated adjusted odds ratios (Table 3).
Factors associated with adolescent pregnancy: bivariate model versus binary logistic regression model.
| Variable | Bivariate, OR (95% CI) | Multivariate, ORa (95% CI) |
|---|---|---|
| History of rape | 8.96 (2.08–38.48) | 7.68 (1.59–37.01) |
| Has a partner | 7.68 (2.29–25.86) | 6.31 (1.71–23.26) |
| Neglect | 4.21 (1.13–15.71) | 4.33 (1.02–18.36) |
| Condom use | 0.38 (0.16–0.94) | 1.65 (0.63–4.34) |
95% CI: 95% confidence interval; OR: odds ratio; ORa: adjusted odds ratio.
This study explored the association between adolescent pregnancy and multiple demographic, familial, social and clinical variables. The main finding was the significant association with a history of neglect and rape.
Child abuse has been associated with negative physical and mental outcomes.11,12 The association between violence and women's reproductive lives has generated significant interest in the past 25 years.13 This association may be studied from the perspective of adult women (violence during pregnancy, perinatal outcomes, condom use, transmission of the human immunodeficiency virus and abortion, among other aspects), but also from the perspective of girls and adolescents who fall victim to other types of violence or child abuse.14–16
Goicolea and Marianne17 found that the main risk factor for adolescent pregnancy is a history of sexual abuse (OR=3.06; 95% CI, 1.08–8.68). Likewise, Noll et al.18, in a meta-analysis of 21 studies, found that sexual abuse significantly increased the likelihood of having an adolescent pregnancy (OR=2.21; 95% CI, 1.94–2.51). Hillis et al.19 analysed various negative experiences in childhood, including sexual abuse, and concluded that there was a strong association with pregnancy (hazard ratio=1.6; 95% CI, 1.4–1.7).
In a classic study, Boyer and Fine20 reported that, in a sample of 535 pregnant adolescents, two thirds had suffered sexual abuse in childhood. In turn, these adolescents presented earlier onset of sexual relations, greater substance use, lower contraception use and a higher risk of prostitution than those who did not have this history. In a recent meta-analysis that included 38 studies and 75,390 participants, Madigan et al.21 found that physical abuse (OR=2.06; 95% CI, 1.75–2.38) and sexual abuse (OR=1.48; 95% CI, 1.24–1.76) was associated with a higher risk of adolescent pregnancy.
In Colombia, according to information dating back to 2010 from the Colombian Gender Issues Observatory (OAG), 19.5% of adolescents had been pregnant at some point (26.7% in the rural area and 17.3% in the urban area). Our study found a prevalence of 21.5%, which is higher than the national figure. This prevalence distances Colombia from its target to reduce adolescent pregnancies to 15%, as set by the Millennium Development Goals.2,4
Woodward et al.22 found that girls aged between 14 and 15 years had a lower cumulative risk of adolescent pregnancy (0.19–1.88) compared to those aged between 16 and 19 years (3.95–21.99), consistent with our findings. The age at onset of sexual activity has been described as another factor associated with adolescent pregnancy.23 Our study found no association with the onset of sexual relations before 15 years of age.
As regards marital status, Sharma et al.24 found that young married women were three times more likely to become adolescent mothers than women who married after 20 (OR=2.92; 95% CI, 1.27–6.79). Alemayehu et al.25 reported that delayed marriage was a protective factor against adolescent pregnancy. Similar results have been published from other studies26,27 consistent with the information reported herein.
The use of family planning methods has been identified as an early determinant of adolescent fertility. Kotchick et al.28 reported that 10–20% of sexually active individuals use condoms.28 In Colombia, knowledge of family planning methods is almost universal and peaks at 99.8%.29 In the aforementioned study, 7 in 10 adolescents reported that they use condoms, but in our study this variable did not act as a protective factor.
As regards the connections between sexual abuse and adolescent pregnancy Blinn-Pike et al. proposed that adolescent pregnancy is a direct result of: a) sexual abuse; b) a dysfunctional family pattern; c) sexual and gender-related socialisation that teaches women that their value is determined by sex; d) low self-esteem, feelings of inefficacy and poor mental health; e) an adolescent's solution to escape abusive domestic situations; and f) interrupted emotional and cognitive development caused by sexual trauma. This study also performed an exploratory analysis of the subgroup of adolescents with a history of rape, and found a strong link between this and major depression (OR=6.25). This association has been reported in numerous cross-sectional and longitudinal studies, which have linked a history of sexual abuse in childhood with anxiety disorders and depression in adulthood.30 Moreover, a strong link was found between a history of rape and attempted suicide (OR=8.95). These figures are consistent with several studies that describe similar findings worldwide, indicating that adolescent mothers present higher rates of pre- and post-natal depression (16–44%) than adult mothers or non-pregnant peers (5–20%). Furthermore, high rates of psychoactive substance abuse have also been found in these subjects (11–52%).31,32 A study in Brazil found a 6% prevalence of cocaine and marijuana use among pregnant adolescents, which was even higher than the prevalence detected in non-pregnant adolescent females.33 This study found no association between adolescent pregnancy and the mental disorders of the adolescent or her parents.
Finally, our findings must be interpreted taking into account the following limitations: firstly, the results are based on the report given by the respondent, which may be affected by memory bias. Secondly, although participation in the study was voluntary, we cannot guarantee that the adolescents answered the questions truthfully. Nor is it possible to guarantee the stability of the psychiatric diagnoses, given the changing nature of the adolescents’ moods, thoughts and behaviours in light of numerous familial, social and individual variables. As such, we cannot guarantee that the adolescents identified as control subjects for this study did not, within a short time frame, become cases themselves. Thirdly, this study did not consider all of the familial, social and individual factors associated with adolescent pregnancy. Fourthly, given that the age at onset of the pregnancy was not available and the fact that this was a cross-sectional study, we cannot guarantee that the factors considered occurred before the adolescent pregnancy, so in this sense we cannot discuss causality. Nevertheless, despite these limitations, this study provides valuable information in relation to adolescent pregnancy in the study population.
ConclusionsThe main finding of this research project is the significant association between adolescent pregnancy and histories of sexual abuse and neglect during childhood and adolescence.
Among the numerous factors associated with this significant negative outcome on adolescent girls’ reproductive health, two factors have been identified for intervention on the family, social and legal levels that broaden the perspective on adolescent pregnancy prevention, which has traditionally focused on sex education.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors thank the Centre for Excellence on Research in Mental Health, Medellín (Colombia), and the Health Secretariat of Medellín.
Please cite this article as: Restrepo Martínez M, Trujillo Numa L, Restrepo Bernal D, Torres de Galvis Y, Sierra G. Abuso sexual y situaciones de negligencia como factores de riesgo de embarazo adolescente. Rev Colomb Psiquiat. 2017;46:74–81.
The wording of the conclusions in the abstract does not have a clear meaning (e.g. you cannot avoid something in childhood by taking action in adolescence). Moreover, the English version is not equivalent (the title is missing).