Achenbach's syndrome is a vascular disorder of the hands and feet. It is of unknown etiology and has a benign course. Because of its low prevalence, available literature is limited, and most publications are case reports. No Latin-American publications were found on the subject. The case of a 58 year-old man is presented, along with a systematic review of the literature to describe its clinical characteristics.
MethodsA literature search was conducted in PubMed, Embase and Lilacs using free terms and controlled vocabulary (MeSH, Emtree, and DeCS).
ResultsAn analysis was made on a total of 23 articles, 19 of which were case reports, with a total of 46 patients, 43 women and 3 men, from 7 countries. The disorder occurs most often in women over 50 years, and is manifested by the sudden appearance of a blue coloration of the palmar surface of the fingers. It is less common in the feet.
ConclusionsAchenbach's syndrome is benign, and does not require medical intervention. Diagnostic methods are of little use. Therefore, identification is important to avoid unnecessary procedures.
El síndrome de Achenbach es un trastorno vascular de manos y pies, de etiología desconocida y de curso benigno. Dada su baja frecuencia de presentación, la literatura disponible es escasa; la mayoría son reportes de casos. No se encontraron publicaciones latinoamericanas sobre el tema. Aquí se presenta un caso clínico, en un hombre de 58 años, y se hace una revisión sistemática de la literatura para describir sus características clínicas.
MétodosSe realizó una búsqueda de literatura en PubMed, Embase y Lilacs utilizando términos libres y vocabulario controlado (MeSH, Emtree y DeCS).
ResultadosSe evaluaron 23 artículos de los cuales 19 fueron reportes de caso. Los reportes de caso muestran la historia de 46 pacientes, 43 mujeres y 3 hombres, en 7 países. El trastorno se presenta más frecuentemente en mujeres mayores de 50 años y se manifiesta por la aparición súbita de una coloración azul de la cara palmar de los dedos y menos frecuente en los pies.
ConclusionesEl síndrome de Achenbach es benigno y no requiere intervenciones médicas. Los métodos diagnósticos son de poca utilidad. Es necesario reconocerlo para evitar procedimientos innecesarios.
A 58-year old university professor attends medical consultation referring recurrent episodes, which began 25 years ago, that start with a sudden moderate sharp pain, usually located in the interphalangeal region of one of the hands (most commonly in the right, Fig. 1) and less frequently in the feet (Fig. 2), sometimes with commitment of the palm (thenar region, Fig. 3) or the sole. After a few seconds or minutes the pain is accompanied by an intense coloration change, which becomes ecchymotic and, sometimes, localized edema and heat appear. The episodes have a variable frequency, in some occasions several months elapse without symptoms, and in other, 3 and 4 episodes can occur in the same month. Although he does not describe clear precipitating factors, he considers that there is an association with cold and mild traumas.
The patient has a history of mild asthma, which started also 25 years ago, and 2 years ago was diagnosed with hypertension (in treatment with losartan 100mg and hydrochlorothiazide 25mg day). In the family history, he refers that a sister has similar episodes which have never led her to consult.
The physical examination, during an intercritical period, shows no alterations. However, the patient brings photographs taken during different episodes. Laboratory tests, which include blood count, blood glucose, electrolytes, lipid profile and liver and kidney function tests, are all normal.
IntroductionThere are different pathological conditions that occur with coloration changes of the extremities. Acute changes are of interest since they may be the underlying representation of a potentially serious disease.1 This broad group of diseases includes Achenbach's syndrome, also called paroxysmal finger hematoma. This syndrome is a clinical condition of low prevalence and unknown etiology.2 It appears as an edema of sudden onset, painful, in one or more fingers, associated with a coloration change, similar to an ecchymosis on the palmar side of the hand. The course of this condition is benign, the symptoms resolve without leaving permanent sequelae.3–5 The available literature on Achenbach's syndrome is scarce given its low frequency of presentation. Most of the publications that are found correspond to case reports. In Latin America there are no publications on the subject.
The limited knowledge and dissemination that this condition has had, added to the great variety of potentially serious diseases which occur with coloration changes of the extremities, highlights the importance of improving the information available in order to avoid misdiagnoses and unnecessary expenses for the healthcare systems.6 The objective of this study was to carry out a systematic literature review to provide an overall approach on Achenbach's syndrome, the possible causes, clinical course, diagnosis and management of the affected patients.
MethodsA literature search was conducted in 3 databases, PubMed, Embase and Lilacs. The following terms were used freely and as controlled vocabulary (MeSH, Emtree and DeCS): blue, purple, cianosis, cyanoses, cyanotic, hematoma, hematoma, ecchymosis, digit, fingers, toe, Achenbach. The search was not limited by language, location or date of publication. Two evaluators, in an independent manner, reviewed the titles and abstracts of the references found, excluding those that were clearly irrelevant and selecting those that brought data from individual patients, whether these were single cases or case series. Subsequently, a review of the references cited in each of the articles included was conducted in order to find additional articles.
ResultsThe search in the 3 databases evaluated yielded 7290 initial references, a number that was reduced to 7219 after eliminating the duplicates and to 44 after eliminating those that were considered irrelevant. After reviewing the full texts, 8 articles were selected2,4,5,7–11 which served to extract the information; when reviewing the references cited there, 4 additional articles were found,12–15 11 articles were found using other search sources.16–26 The first description dates back to 1958, by the German physician Walter Achenbach16 as a condition which he called “paroxismal hand hematoma” or “finger apoplexia”.24 He presented 6 cases of women who had suffered recurrent attacks on different fingers of the hands; all attacks started with pain of acute onset on the palmar region of the fingers, followed by coloration changes thereof.24 Who spoke first about Achenbach's syndrome was Korting, in 1967.19 The next publication, where it was described as acute blue finger, was made in England in 1982.7 As Griffiths et al. state, it is possible that this disorder is more common than what is reported in the literature.18
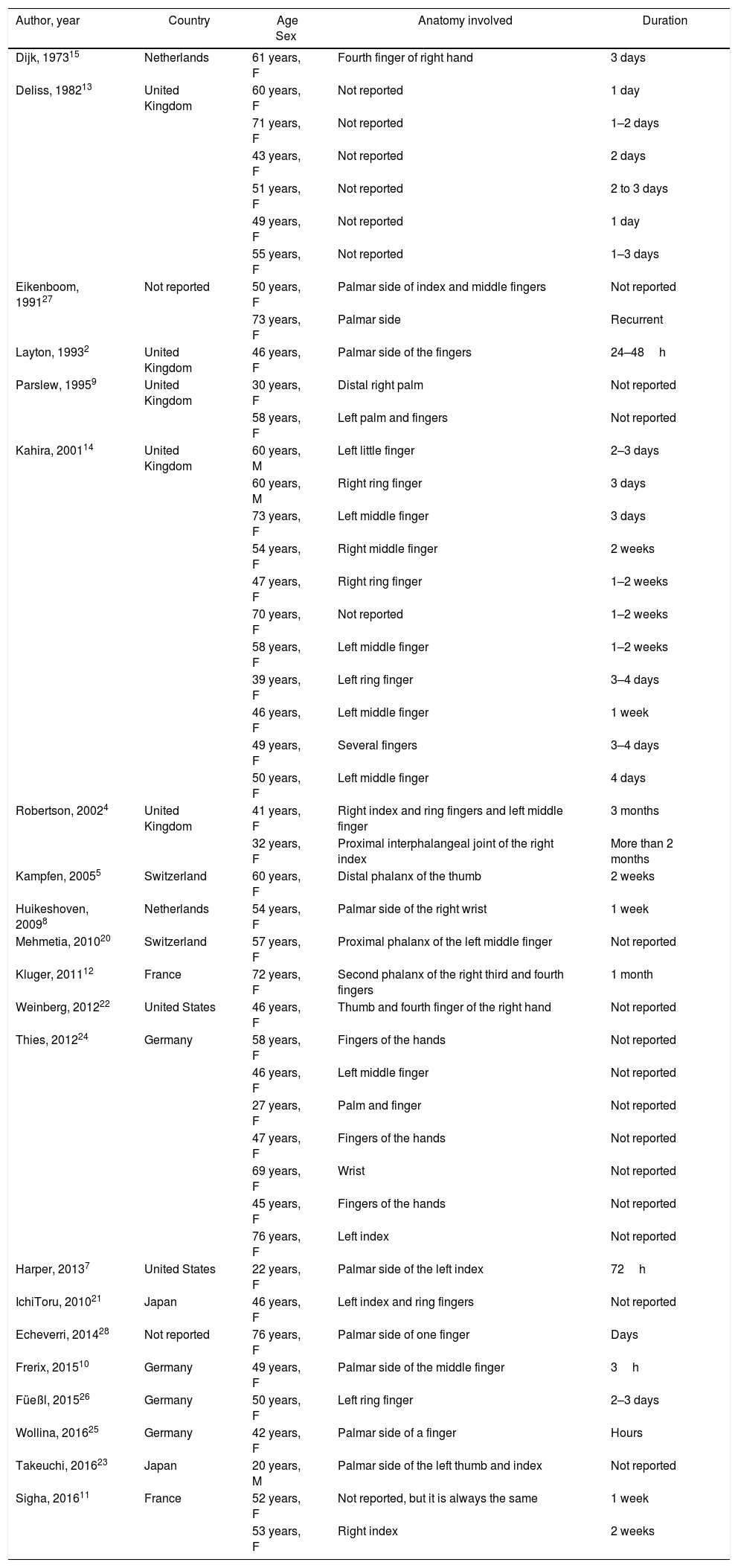
The clinical characteristics of the 46 patients (women 43; 93.4%) described in the 19 articles are shown in Table 1. The ages of the patients are between 22 and 76 years (mean: 52.3 years and median: 50 years) in women, and in men there are 2 cases with an age of 60 years and one case with an age of 20 years (mean: 46.6 years). Except for 2 cases published in the United States and other 2 in Japan, all the rest are European, mainly from the United Kingdom (22 cases), but also from France (3 patients) and 8 cases are from Germany, the Netherlands and Switzerland.
Case reports, Achenbach's syndrome, in chronological order of publication.
| Author, year | Country | Age Sex | Anatomy involved | Duration |
|---|---|---|---|---|
| Dijk, 197315 | Netherlands | 61 years, F | Fourth finger of right hand | 3 days |
| Deliss, 198213 | United Kingdom | 60 years, F | Not reported | 1 day |
| 71 years, F | Not reported | 1–2 days | ||
| 43 years, F | Not reported | 2 days | ||
| 51 years, F | Not reported | 2 to 3 days | ||
| 49 years, F | Not reported | 1 day | ||
| 55 years, F | Not reported | 1–3 days | ||
| Eikenboom, 199127 | Not reported | 50 years, F | Palmar side of index and middle fingers | Not reported |
| 73 years, F | Palmar side | Recurrent | ||
| Layton, 19932 | United Kingdom | 46 years, F | Palmar side of the fingers | 24–48h |
| Parslew, 19959 | United Kingdom | 30 years, F | Distal right palm | Not reported |
| 58 years, F | Left palm and fingers | Not reported | ||
| Kahira, 200114 | United Kingdom | 60 years, M | Left little finger | 2–3 days |
| 60 years, M | Right ring finger | 3 days | ||
| 73 years, F | Left middle finger | 3 days | ||
| 54 years, F | Right middle finger | 2 weeks | ||
| 47 years, F | Right ring finger | 1–2 weeks | ||
| 70 years, F | Not reported | 1–2 weeks | ||
| 58 years, F | Left middle finger | 1–2 weeks | ||
| 39 years, F | Left ring finger | 3–4 days | ||
| 46 years, F | Left middle finger | 1 week | ||
| 49 years, F | Several fingers | 3–4 days | ||
| 50 years, F | Left middle finger | 4 days | ||
| Robertson, 20024 | United Kingdom | 41 years, F | Right index and ring fingers and left middle finger | 3 months |
| 32 years, F | Proximal interphalangeal joint of the right index | More than 2 months | ||
| Kampfen, 20055 | Switzerland | 60 years, F | Distal phalanx of the thumb | 2 weeks |
| Huikeshoven, 20098 | Netherlands | 54 years, F | Palmar side of the right wrist | 1 week |
| Mehmetia, 201020 | Switzerland | 57 years, F | Proximal phalanx of the left middle finger | Not reported |
| Kluger, 201112 | France | 72 years, F | Second phalanx of the right third and fourth fingers | 1 month |
| Weinberg, 201222 | United States | 46 years, F | Thumb and fourth finger of the right hand | Not reported |
| Thies, 201224 | Germany | 58 years, F | Fingers of the hands | Not reported |
| 46 years, F | Left middle finger | Not reported | ||
| 27 years, F | Palm and finger | Not reported | ||
| 47 years, F | Fingers of the hands | Not reported | ||
| 69 years, F | Wrist | Not reported | ||
| 45 years, F | Fingers of the hands | Not reported | ||
| 76 years, F | Left index | Not reported | ||
| Harper, 20137 | United States | 22 years, F | Palmar side of the left index | 72h |
| IchiToru, 201021 | Japan | 46 years, F | Left index and ring fingers | Not reported |
| Echeverri, 201428 | Not reported | 76 years, F | Palmar side of one finger | Days |
| Frerix, 201510 | Germany | 49 years, F | Palmar side of the middle finger | 3h |
| Füeßl, 201526 | Germany | 50 years, F | Left ring finger | 2–3 days |
| Wollina, 201625 | Germany | 42 years, F | Palmar side of a finger | Hours |
| Takeuchi, 201623 | Japan | 20 years, M | Palmar side of the left thumb and index | Not reported |
| Sigha, 201611 | France | 52 years, F | Not reported, but it is always the same | 1 week |
| 53 years, F | Right index | 2 weeks |
Achenbach's syndrome is characterized by the appearance of hematomas, spontaneous or associated with minor trauma, on the palmar side of the fingers. It involves more frequently the fingers of the hands, although there are reports of commitment of the palms, soles or toes. It is associated with pain, sensation of pain and edema on the site of appearance of the hematoma.2–5,11,12
The female predominance of this condition is clear and has been described by Kampfen et al.,5 who speak of a ratio of 7 women for every man. Although it can occur at any age, its maximum peak seems to be around 50 years, the frequency of presentation increases in people older than 50 years.2,4,5,8,9,12 Its etiology is unknown, however, it has been found an association with conditions such as acrocyanosis, gastrointestinal diseases, biliary diseases and migraine.2 One case was associated with systemic lupus erythematosus.21 It is believed that this condition could have a vascular origin5; the capillary fragility associated with age could explain the symptoms presented by patients affected by this condition.12
The only systematic review of the subject, published in 2015, included 12 patients aged between 22 and 76 years. The discoloration of the fingers was present in all the patients, while the blue coloration only in 10; 7 had pain, 7 edema, 3 paresthesias and 3 itching. The mean time to symptom resolution was 4 days. The most frequently affected anatomical region was the palmar aspect of the fingers. All patients were studied with coagulation tests, blood count, sedimentation rate, electrolytes and immunological tests. In some of them, hand ultrasound, X-rays, angiography and biopsy were performed, which were always negative. In summary, none of the studies carried out on the patients showed conclusive physiopathological results, however, given the clinical characteristics that are alarming for the patient and the physician, it is usual that patients undergo multiple studies.
Cowen et al., in the United Kingdom, in a retrospective study, analyzed 22 patients who consulted for acute blue finger, 17 of them were women. Only in 3 of them, the episodes were recurrent (including a median follow-up of 19 months). The most frequently affected finger was the index. Other symptoms, in addition to the coloration change, that in average had been present for 6 days at the time of consultation, were pain, altered sensitivity, edema and sensation of cold finger. Five patients were hospitalized, one received intravenous heparin and subsequently warfarin, and 15 received antiplatelet therapy. At the week 6 of follow-up, the symptomatology persisted in only 2 patients. The authors conclude that acute blue finger syndrome is a rare condition that affects mainly women, that there are no effective diagnostic methods but that it is convenient to rule out cardiac or thrombotic alterations before establishing the diagnosis. There are no management interventions with proven outcomes.17
As part of a study of Raynaud's phenomenon, it was conducted a study in 3 geographic areas of France which included 802 patients, 548 women and 254 men, aged between 18 and 84 years, who were asked a series of questions that allowed to reach the diagnosis of paroxysmal hematoma of the fingers in the patients who reported a history of recurrent hematomas in the fingers of sudden spontaneous and painful onset. The results report prevalences for men and women of 12.4 and 1.2%, respectively; in total 71 patients were diagnosed with the condition. No geographical differences were found in the 3 regions despite the difference in climate. A strong relationship with age was evidenced, being more frequently reported by women over 40 years of age. Within the risk factors and associated conditions it was found a significant relationship with smoking, estrogen therapy and low consumption of alcohol; it was not possible to confirm this relationship when carrying out the age adjusted analysis. There was neither evidenced a relationship with variables associated with estrogens or menopause. The majority of patients did not report associated serious comorbidities. With regard to acrocyanotic syndromes, it was found a significant association with Raynaud's phenomenon and changes associated with cold. As for the clinical presentation, it was found that the mean age of presentation was 48 years, and the mean frequency of recurrences was 1.2 per year with an interquartile range of 0.8–2.9. The involvement of the fingers was greater in the third, followed by the second; however, any finger may be affected. The right hand was affected more frequently than the left and the involvement of the palmar side was more frequent. 100% of patients reported pain and ecchymosis. The average duration of the clinical picture was 3 days, interquartile range of 2–3.29
19 case reports published and available and a systematic review containing the information of 46 patients diagnosed with Achenbach's syndrome were found in the search of studies that was carried out. Of the 46 cases evaluated in the case reports, 43 patients were female; the minimum age for women was 22 years and the maximum age was 76, with a median of 50 years. Two of the 3 male subjects reported 60 years of age and the third 20 years. The hands were the most frequently affected anatomical site, 38 of the 46 cases reported symptoms or signs on one or more fingers, 8 cases did not report an anatomical site. Regarding the symptoms, pain was the most frequently reported symptom, in 20 cases, as well as coloration changes, in 40 cases; the presence of hematomas was reported in 19 cases. The time to resolution of symptoms was very varied, finding data from hours to days or weeks. There were 23 cases that reported recurrence of the symptomatology at non-regular time intervals. The studies report the performance of different diagnostic tests to the patients (Doppler ultrasonography of the arteries, angiography, X-rays, capillaroscopy, prothrombin time, thrombin time, INR, C-reactive protein, erythrocyte sedimentation rate, total leukocyte count, platelet count, complete blood count, immunological and biochemical profiles). None of the laboratory tests performed was conclusive. The skin biopsies were normal or showed results that did not provide conclusive information.2,9 In the patients who underwent capillaroscopy, no hemorrhages or other alterations in the morphology of the capillaries or in the blood flow were found. The results of the angiography showed that small vessel disease could exist.4,6,14,24 The arterial Doppler ultrasonography did not showed alterations in any patient.5,7,12,14
It was found that the symptoms and coloration changes appear more frequently in the hands, with greater involvement of the index and middle fingers. Three of the studies included describe that, although it is infrequent, there is a commitment of the palms or of one or several knuckles.2,11,12
The blue coloration on the fingers can be the manifestation of a potentially serious disease. Brown1 proposes a diagnostic algorithm for the patients who have a blue coloration on one or more fingers. Trauma or alterations in coagulation should be ruled out in the initial evaluation, as well as cyanosis secondary to hypoxemia or methemoglobinemia. It may also be a coloration change induced by cold, by vasospastic disorders such as Raynaud's phenomenon or by acrocyanosis secondary to hematological alterations, drugs, malignant conditions, metabolic, neurological, psychiatric or alimentary disorders or arsenic poisoning. The possibility of thrombosis or peripheral embolism should also be considered.
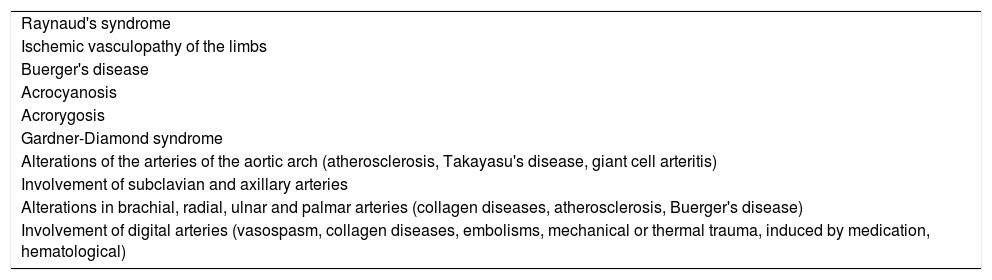
The differential diagnoses of Achenbach's syndrome include several conditions with similar clinical characteristics, associated with the presence of acute blue coloration of the fingers. Korzadeh et al.6 describe a diagnostic algorithm that allows the evaluation of the characteristics of some of the most common differential diagnoses. Thus, the authors propose to start from the symptoms (blue coloration, pain, edema and paresthesias), common to most of these conditions, and consider different aspects that help us to differentiate them. The absence of distal pulses indicates a probable acute ischemia of the limbs. The recurrent and chronic episodes, the progressive coloration changes in the fingers from blue to white and their relation with temperature changes suggest a picture of Raynaud's syndrome. It indicates that in young patients, usually children and individuals under 30 years of age, without gender predilection, who perform activities with exposure to low temperatures, the clinical reasoning should consider acrocyanosis as part of the differential diagnoses. The lesions that appear clinically with pain, edema, paleness, pruritus and ulceration should guide the diagnosis toward acrorygosis or pernio. The patients who have coloration changes associated with pain and edema in any part of the body, accompanied by personality changes, vagal symptoms and bleeding, point toward a picture of Gardner-Diamond syndrome. Finally, it shows that, in women over 60 years of age, with normal temperature of the limbs and a positive or negative antecedent of trauma, there is a high probability that it is Achenbach's syndrome.6
Below are described some of the characteristics of the diseases and Table 2 shows the main differential diagnoses of this entity. In Raynaud's syndrome, the average age of onset is 14 years, and the cases that start after age 30 are rare. The clinical findings include paleness, cyanosis and redness of the fingers of the hands and feet, secondary to a vasospastic phenomenon related to stress and cold.17 Peripheral vascular disease differs from Achenbach's syndrome by its predominance in males and an older age of presentation.17 When differentiating between paroxysmal hematoma of the fingers and spontaneous digital venous thrombosis, it is useful to highlight that the second rarely occurs in women and usually appears as a bluish and painful nodule in the proximal interphalangeal joint, however, the pain is less intense than that experienced by patients with Achenbach's syndrome.7 Patients with livedo reticularis show a speckled purpuric skin pattern characteristic of this disease.30
Main differential diagnoses of Achenbach's syndrome.
| Raynaud's syndrome |
| Ischemic vasculopathy of the limbs |
| Buerger's disease |
| Acrocyanosis |
| Acrorygosis |
| Gardner-Diamond syndrome |
| Alterations of the arteries of the aortic arch (atherosclerosis, Takayasu's disease, giant cell arteritis) |
| Involvement of subclavian and axillary arteries |
| Alterations in brachial, radial, ulnar and palmar arteries (collagen diseases, atherosclerosis, Buerger's disease) |
| Involvement of digital arteries (vasospasm, collagen diseases, embolisms, mechanical or thermal trauma, induced by medication, hematological) |
Acrocyanosis is an entity that is characterized by a blue coloration of the hands and feet, secondary to a low cardiac output or local vasomotor disorders; it differs from the paroxysmal hematoma of the fingers in that it has a clear etiology.1 Among the autoimmune diseases, there is the vasculitic purpura, a disease of unknown etiology that occurs most frequently in children, although it can occur in adults; it is characterized by inflammation of vessels of small caliber that gives rise to palpable purpuric lesions, arthralgias, crampy abdominal pain, gastrointestinal hemorrhages and nephritis, which is the most common manifestation in adults.31
FundingThis work did not receive any funding.
Conflict of interestThe authors declare they do not have any conflict of interest.
Please cite this article as: Jiménez PR, Ocampo MI, Castañeda-Cardona C, Rosselli D. Síndrome de Achenbach: presentación de un caso y revisión sistemática de la literatura. Rev Colomb Reumatol. 2017;24:230–236.