Acropachy, also called clubbed fingers, presents as increased nail convexity over a thickened distal phalanx. Its origin is multifactorial, with the most frequent cause being neoplasms, although it can also be idiopathic. They can be found in isolation, or as part of hypertrophic osteoarthropathy. The importance of its diagnosis lies in the high frequency of underlying malignant pathology, so it must be rapid and comprehensive. Two cases are presented of patients with acropachy associated with underlying neoplasia.
Las acropaquias, también llamadas dedos en palillo de tambor, se presentan como un aumento de la convexidad ungueal sobre una falange distal engrosada. Su origen es multifactorial, siendo la causa más frecuente las neoplasias, aunque también puede ser idiopático. Pueden encontrarse de forma aislada o formando parte de la osteoartropatía hipertrófica. La importancia de su diagnóstico radica en la alta frecuencia de enfermedad maligna subyacente, por lo que debe ser rápido y exhaustivo. Presentamos 2 casos de pacientes con acropaquias asociados a neoplasia subyacente.
Acropachy is a sign characterized by an increase of the nail convexity over a thickened distal phalanx. Although it can be unilateral, it is usually bilateral and asymptomatic. Its origin is multifactorial, being the most frequent cause the neoplasms, especially of the lungs, but it could be of infectious or vascular origin, and there are also idiopathic cases. We present 2 patients with acropachy and subsequent diagnosis of underlying neoplasia.
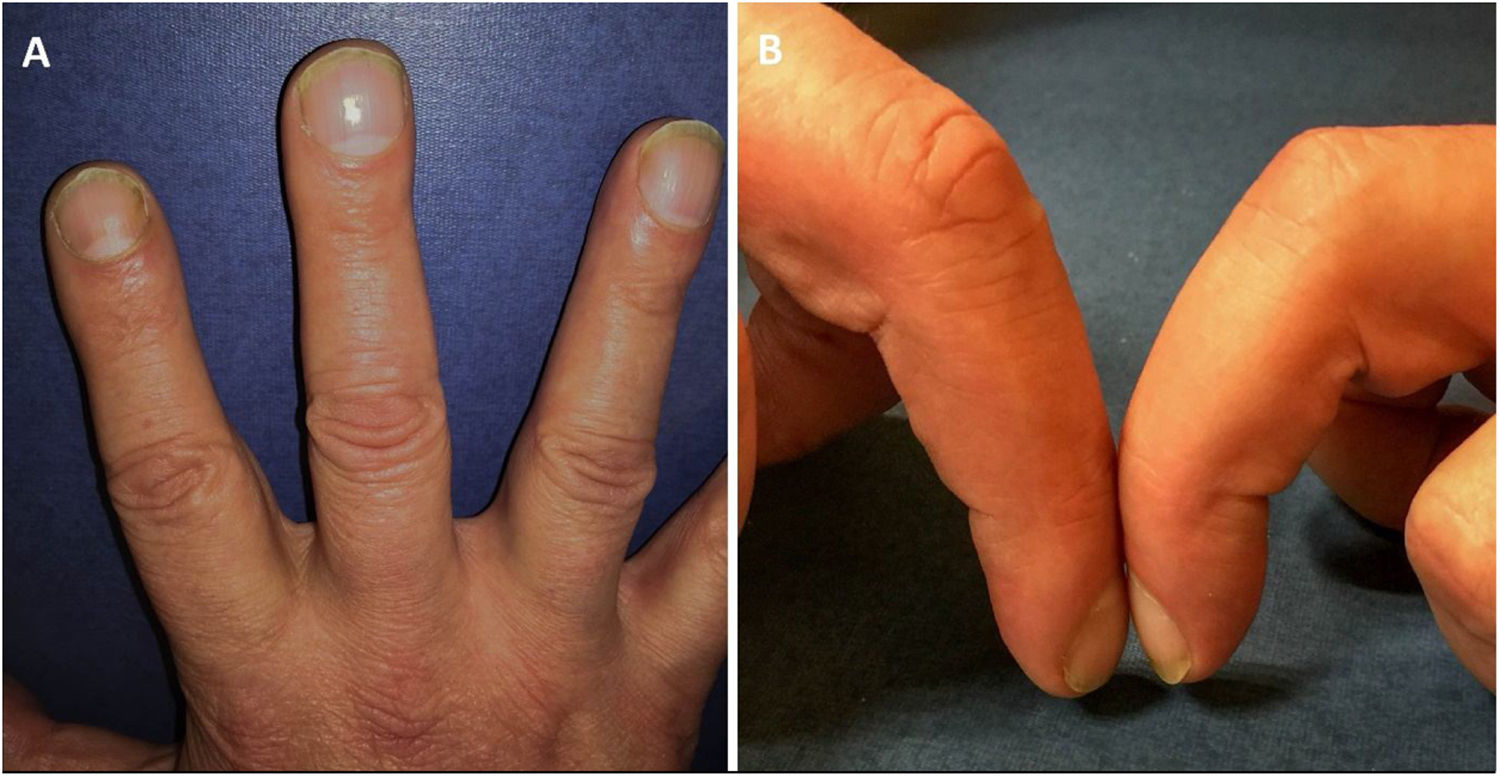
Clinical casesThe first case is a 55-year-old male patient who consulted to rheumatology for bilateral knee pain, which was diagnosed as gonalgia of mechanical origin. During the examination it was observed acropachy on both hands, which had not been evidenced by the patient (Fig. 1A). The patient reported mild pain in the finger pads of the hands and associated significant loss weight. Blood tests were requested, which showed a slight increase in ESR; and brain, thoracic, abdominal and pelvic CT scans were also requested, which revealed mediastinal lymphadenopathies and wall thickening of the esophagus, whose biopsy confirmed the diagnosis of esophageal neoplasia.
The second case was a 51-year-old man, smoker, who consulted for tinea pedis. During the visit, a slight increase in volume of the distal phalanges of both hands and loss of the nail window were casually observed (Schamroth’s sign) (Fig. 1B). Laboratory tests were requested, in which an increase of the CEA tumor marker stood out; the occult blood in stool was positive, and therefore a colonoscopy and biopsy were performed, after which the diagnosis of rectal neoplasia was confirmed.
DiscussionAcropachy, also known as digital hippocratism, drumstick fingers or watch glass nails, have a multifactorial origin and their etiopathogenesis is not well defined. There are several overlapping hypotheses1: the humoral theory (the most accepted), the theory of hypoxia and the neurogenic theory, which lead to increased production of growth factors (VEGF and PDGF) that cause an overproduction of bone and soft tissue. In such a way, acropachy are formed.
They can appear isolated or associated with hypertrophic osteoarthropathy, acquired or hereditary disease characterized by the triad of acropachy, periostosis of long bones and synovitis.
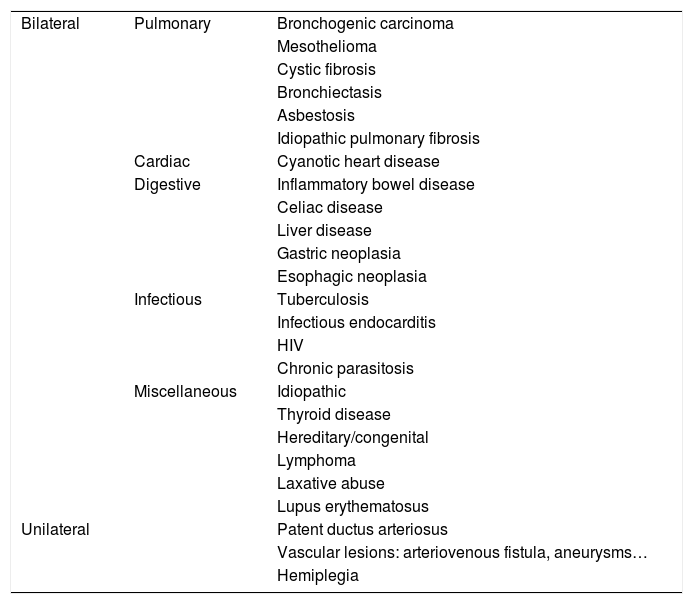
As for their etiology,2 in most of them there is an underlying cause (Table 1). In the unilateral forms of presentation, the presence of patent ductus arteriosus, vascular lesions or hemiplegia must be ruled out. In bilateral cases, the most frequent cause is lung disease, especially of malignant origin. Lung cancer is the most frequent cause of acropachy, in which this sign appears with an incidence of 5%–17% of the cases. Although in some publications the cause of acropachy has been attributed to chronic obstructive pulmonary disease, this does not justify the presence of this finding, so another underlying disease should be ruled out. Other causes of bilateral acropachy are inflammatory bowel disease, infectious causes such as tuberculosis or HIV, or thyroid diseases, among others.
Etiology of acropachy.
| Bilateral | Pulmonary | Bronchogenic carcinoma |
| Mesothelioma | ||
| Cystic fibrosis | ||
| Bronchiectasis | ||
| Asbestosis | ||
| Idiopathic pulmonary fibrosis | ||
| Cardiac | Cyanotic heart disease | |
| Digestive | Inflammatory bowel disease | |
| Celiac disease | ||
| Liver disease | ||
| Gastric neoplasia | ||
| Esophagic neoplasia | ||
| Infectious | Tuberculosis | |
| Infectious endocarditis | ||
| HIV | ||
| Chronic parasitosis | ||
| Miscellaneous | Idiopathic | |
| Thyroid disease | ||
| Hereditary/congenital | ||
| Lymphoma | ||
| Laxative abuse | ||
| Lupus erythematosus | ||
| Unilateral | Patent ductus arteriosus | |
| Vascular lesions: arteriovenous fistula, aneurysms… | ||
| Hemiplegia |
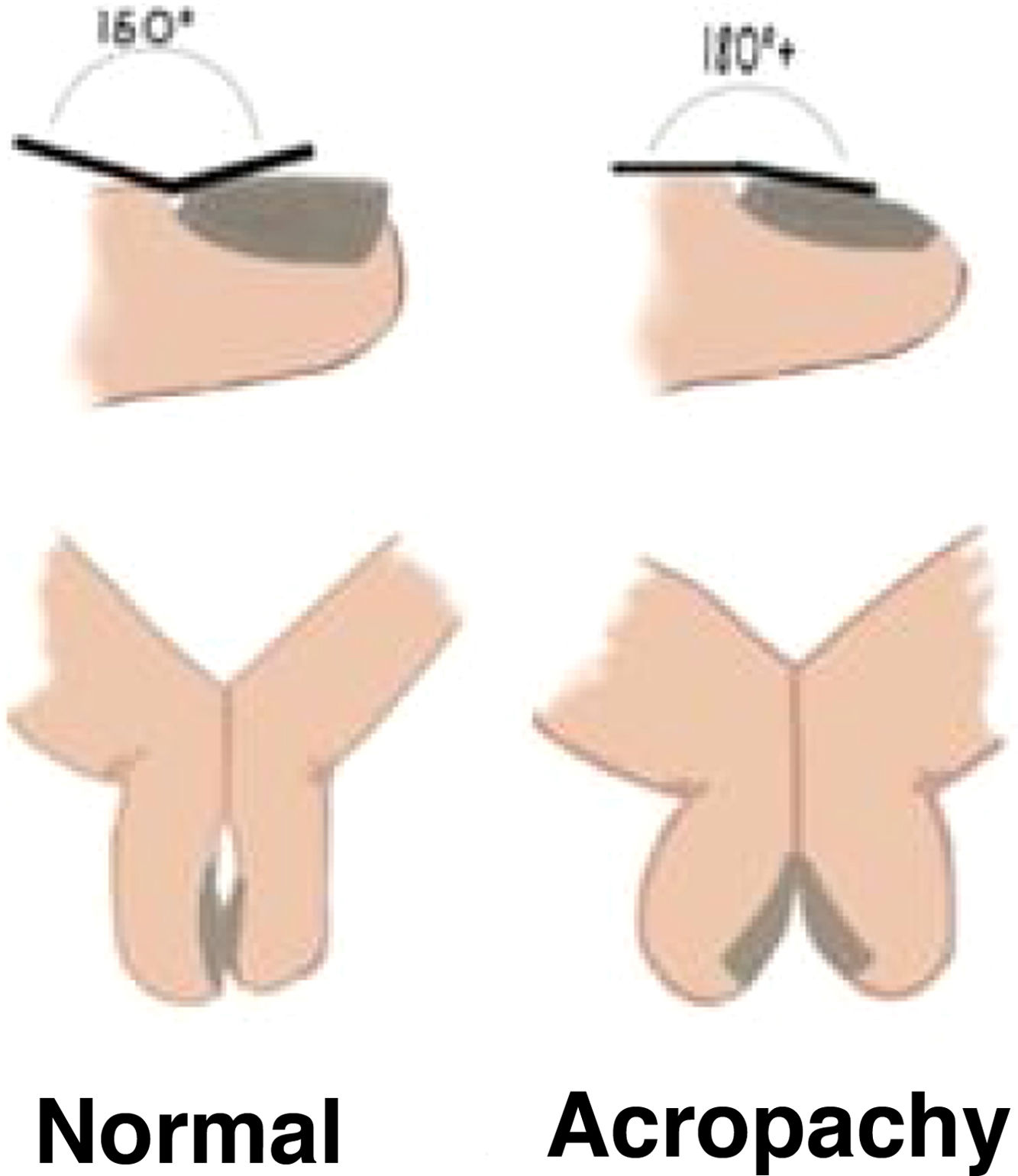
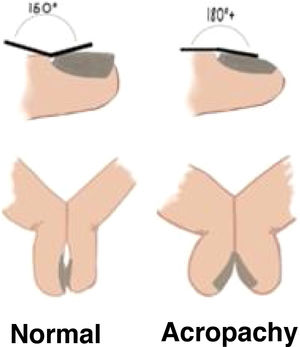
Its clinical diagnosis is established by measuring the Lovibond’s angle (angle created between the skin proximal to the cuticle and the nail bed, which is pathological when it is >180°), and the Schamroth’s sign (which is the loss of the window formed between the nail bed of two opposite fingers) (Fig. 2). In case of diagnostic doubts, ultrasound can be very useful.3
There are different degrees or stages of acropachy:4 grade 1) periungual erythema and softening of the nail bed; grade 2) increase in the normal angle between the nail bed and the proximal nail fold; grade 3) increased nail convexity; grade 4) increased thickness of the distal phalanx, with which the distal interphalangeal joint can become hyperextensible (appearance of acropachy); and grade 5) brilliant or ground glass coloration of the nail and the adjacent skin. Although these degrees do not have clinical significance, they would allow us their early identification.
Once the diagnosis of acropachy has been established, it is important to assess initially whether they are unilateral, and thus perform a MRI to rule out vascular lesions, or bilateral. In the latter group, if they occur in isolation, the study should be started with a chest X-ray or CT scan and tumor markers, to detect underlying malignant disease, while if they present with synovitis we should request an X-ray and ultrasound of the affected fingers for the diagnosis of HOA. If after this initial study no cause for the drumstick fingers is found, other complementary tests should be requested according to the medical history of the patient before being able to ensure that they have an idiopathic origin (Supplementary material).
The differential diagnosis includes pseudoclubbing5 (with causes such as subungual hemangioma, sarcoidosis, limited scleroderma, or hyperparathyroidism secondary to insufficiency with acroosteolysis), chronic paronychia, enchondroma of the distal phalanx or dactylitis. For this purpose, the medical record would be of vital importance, together with the associated physical findings and the complementary tests.
As for their treatment, to date there are no specific therapeutic options for acropachy, although they usually subside after the cure of the underlying disease if it exists.
ConclusionsWe highlight the importance of early recognition of acropachy for a rapid and comprehensive study of underlying malignant disease, as in our cases.
Conflict of interestThe authors declare that they have no conflict of interest.
Please cite this article as: Corral-Forteza M, Iglesias-Sancho M, García-Miguel J, Salleras-Redonnet M. Acropaquias: del signo a la enfermedad. Rev Colomb Reumatol. 2021;28:227–229.