Rheumatoid arthritis is the most prevalent systemic autoimmune disease in the world. It usually manifests as a symmetrical chronic polyarticular inflammation that affects the small and medium size, with the metacarpophalangeal joint, proximal interphalangeal, and the carpus being the most affected. There is atlanto-axoid joint involvement late in the course of the disease. The case is presented of an 80 year-old patient that debuted with cervical compression myelopathy due to the presence of pannus in the atlanto-axoid joint.
La artritis reumatoide es la enfermedad autoinmune sistémica más prevalente del mundo. Suele manifestarse como una inflamación poliarticular crónica simétrica que afecta las articulaciones de pequeño y mediano tamaño, siendo las metacarpofalángicas, interfalángicas proximales y el carpo, las más afectadas. Usualmente afecta la articulación atlanto-axoidea de forma tardía en el trascurso de la enfermedad. Presentamos el caso de un paciente de 80 años que comienza con mielopatía compresiva cervical por la presencia de pannus en la articulación atlanto-axoidea.
Rheumatoid arthritis (RA) is the most prevalent systemic autoimmune disease around the world. It is estimated that up to 1% of the population suffers from this condition, with an incidence ranging between 20 and 50 per 100,000 inhabitants per year in North America and Europe.1 A prevalence study in Colombia reported a rate of 0.9/100 inhabitants in 2005.2 This disease usually manifests as chronic, symmetrical polyarticular inflammation affecting the small and medium size joints, with the metacarpal-phalangeal, proximal interphalangeal and the carpal being the most affected. However, other joints are usually involved such as the knee, the hip, the ankle, the elbow, and the shoulder.3 It seldom affects the axial skeleton, except for the involvement of the atlantoaxial joint which is highly specific in this condition, and presents late over the course of the disease.4
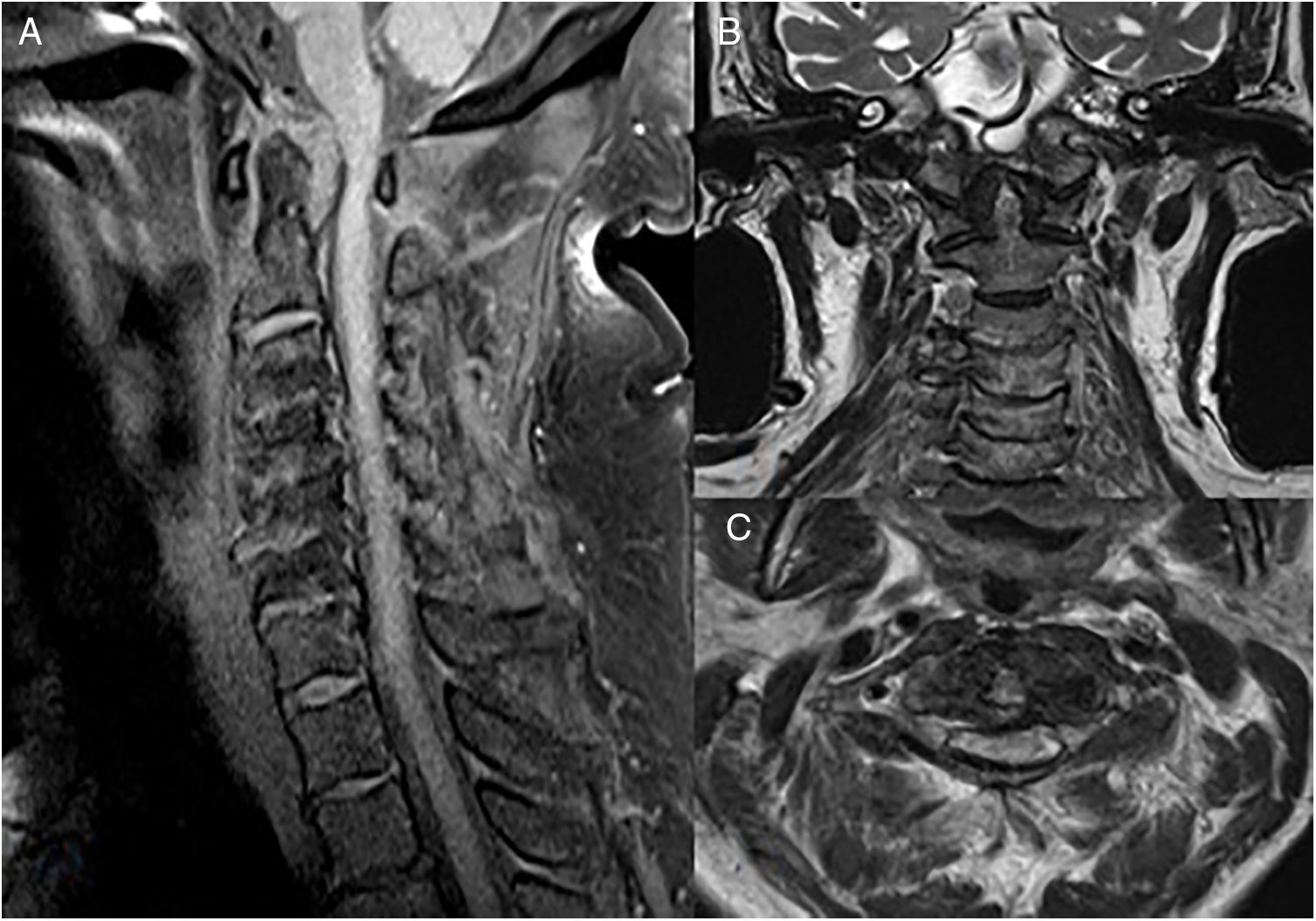
Case descriptionThis is an 80-year old male patient, hypertensive and long-time smoker. He presents with symptoms evolving over 5 months, with the presence of paresthesia and hypoesthesia of the fingers and forearms. The patient develops progressively dysesthesia of the lower extremities and is unable to walk due to weakness. He has been bed-ridden for 2 months and became dependent for all his activities of daily living. He experienced a fall and hence was referred to a 4th level hospital. The physical examination revealed symmetrical quadriparesis, generalized hyperreflexia, bilateral Babinski, generalized hypoesthesia with C3 level of sensitivity, and bilateral Hoffman. The plain MRI of the spine (Fig. 1) showed evidence of odontoid pannus causing acquired canal narrowing with severe stenosis of the spinal canal and bone marrow compression with acute myelopathy signs. Other findings included bone marrow edema in the cervical segment of the spine, as well as degenerative changes throughout the segments of the cervical spine. The laboratory analyses resulted in a positive rheumatoid factor (113IU/ml), negative anti-cyclic citrullinated peptide (4.1U/ml), acute phase reactants (globular sedimentation rate, C-reactive protein) and negative antinuclear antibodies. The hand and foot X-rays showed no bone erosions, with osteo-arthrosis changes. The patient underwent decompression and C1–C2 arthrodesis with good postoperative evolution and partial recovery of his motor deficit. Three weeks after admission the patient was discharged on a treatment with prednisolone 10mg, sulfasalazine 1000mg and leflunomide 20mg per day. The patient experienced clinical improvement and was able to walk unassisted.
DiscussionThis is a patient in his ninth decade of life who began showing neurological involvement due to pannus in the atlantoaxial joint, with no evidence of peripheral joint involvement, which is quite unusual.
Cervical spine involvement is a frequent condition in RA, reported in up to 80% of the patients.5,6 It affects the atlanto-occipital, atlantoaxial or subaxial C3 to C7 joints, with the atlantoaxial joint being the segment of the cervical spine more frequently involved.7 It may be asymptomatic until headache and cervical pain manifestations develop, or with more severe manifestations such as compressive myelopathy, brain stem compression and vertebrobasilar insufficiency, which are life-threatening and require emergency management.4,6
Similar to what happens with the peripheral joints, the inflammation of the synovial tissue leads to the development of pannus and later erosion, as well as to joint destruction which affects juxta-articular structures and weakens the adjacent ligaments.8,9 The bone marrow compression or the compression of the encephalic trunk is the most severe complication derived from the cervical spine involvement in RA, and it could be the consequence of the direct compression caused by the pannus or due to joint subluxation as a result of instability.
Usually, the clinically significant cervical spine disorder occurs following a long-lasting active disease and presents with erosive peripheral joint involvement. Consequently, the onset of RA with cervical spine involvement is rare.10 There are few cases reported that start as a cervical marrow syndrome with no evidence of peripheral arthritis.11,12 Several studies have identified risk factors for axial joint involvement, including: age >45 years, use of corticosteroids, erosions and destructive changes in the peripheral joints, and non-responders to DMARDs.13
Images are critical to assess the axial involvement in RA. The cervical spine radiograph is useful in asymptomatic patients. Dynamic projections are needed to identify subluxations, however these images fail to identify any soft tissue abnormalities that may compromise the spinal canal, as it is the case with our patient with pannus-associated myelopathy. This drawback is also present in CT images and hence MRI becomes the modality of choice in symptomatic patients, due to its ability to detect soft tissue and bone marrow abnormalities.4
Treatment with DMARDs and biologics prevent the development of cervical spine involvement in RA. However, is becomes insufficient once the clinical manifestations set in, particularly in the presence of neurological deficit indicating myelopathy or brain stem compression, in which case surgical management is absolutely required.4,14 Whilst compressive myelopathy is rare, it leads to a poor prognosis, even after surgery, since there is limited possibility of recovering back to the normal functional levels present prior to the bone marrow involvement.8,9
The case herein discussed is part of the different modes of clinical presentation in RA. Early clinical diagnosis and the MRI findings in the cervical spine, forced the indication for immediate surgery, resulting in significant improvement of the patient's condition.
ConclusionThe atlantoaxial involvement in RA may be the first, and sometimes the only evidence of disease activity. The clinician should keep in mind this differential diagnosis when dealing with patients presenting with cervical spine involvement.
Conflict of interestNone of the authors have any conflict of interest to disclose with regards to this paper.
Please cite this article as: Castaño-Quintero S, Rivillas J-A, Santos VA, Echeverri A. Mielopatía compresiva por pannus en articulación atlanto-axoidea como primera manifestación de artritis reumatoide. Reporte de caso. Rev Colomb Reumatol. 2020;27:112–115.